21 Oct Utilization of an Innovative Decision Support Software System to Enhance Detection of Decompensating Patients A4

Utilization of an Innovative Decision Support Software System to Enhance Detection of Decompensating Patients A4
Background
Patients requiring transfer from the medical wards to an intensive care unit (ICU) have increased morbidity and mortality compared to patients who are admitted to the ICU directly from the emergency department (ED). More specifically, patients requiring transfer from the hospital ward to the ICU within 24 hours of admission from the ED may have higher rates of adverse events and death. Delayed recognition of early decompensation and intervention can lead to increased morbidity and mortality; some reports indicate an increase in mortality of up to 30%. Rapid response teams and systems were developed to identify and respond to these decompensation events and decrease hospital mortality and non-ICU cardiac arrests.
Methods
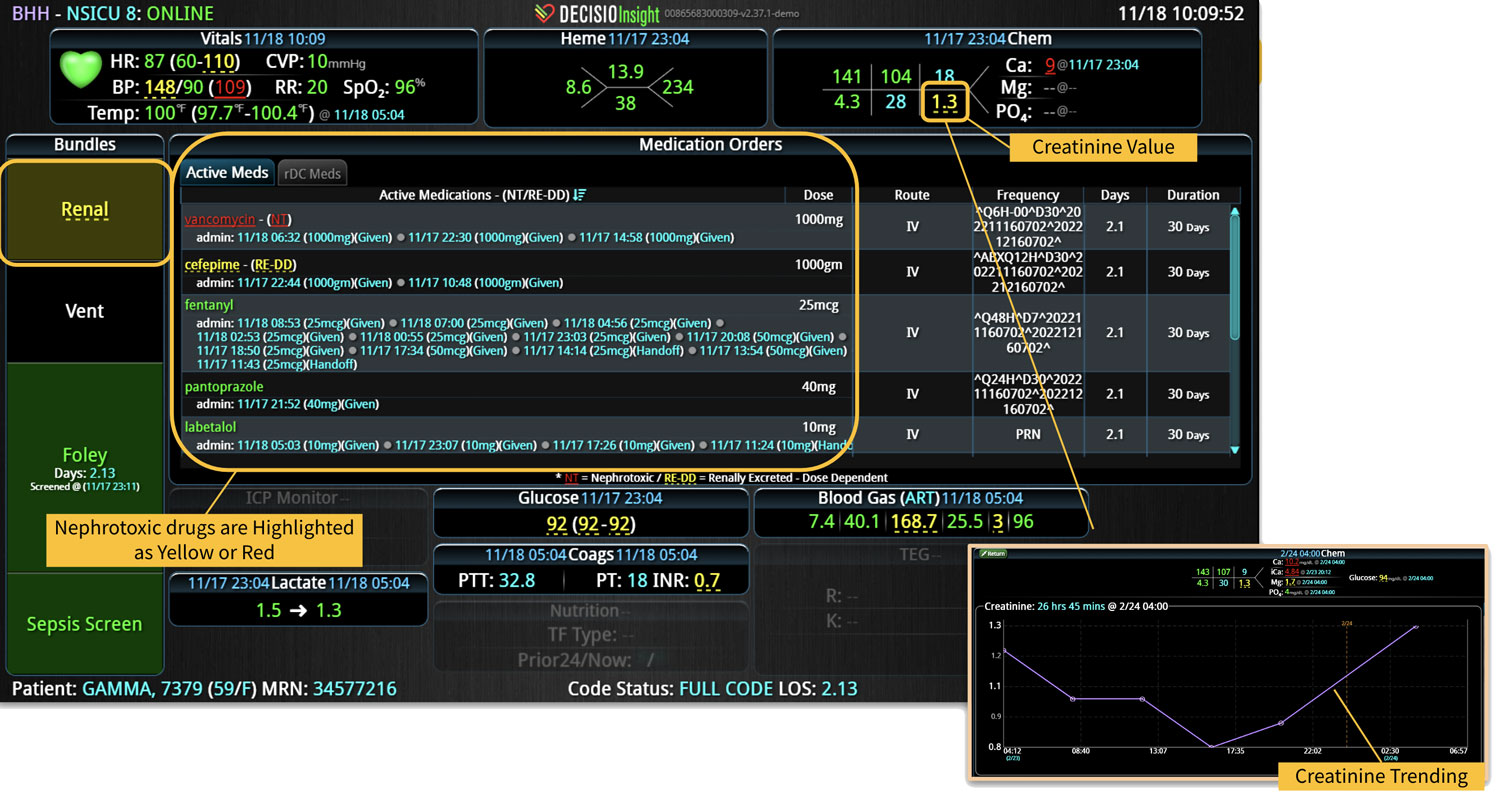
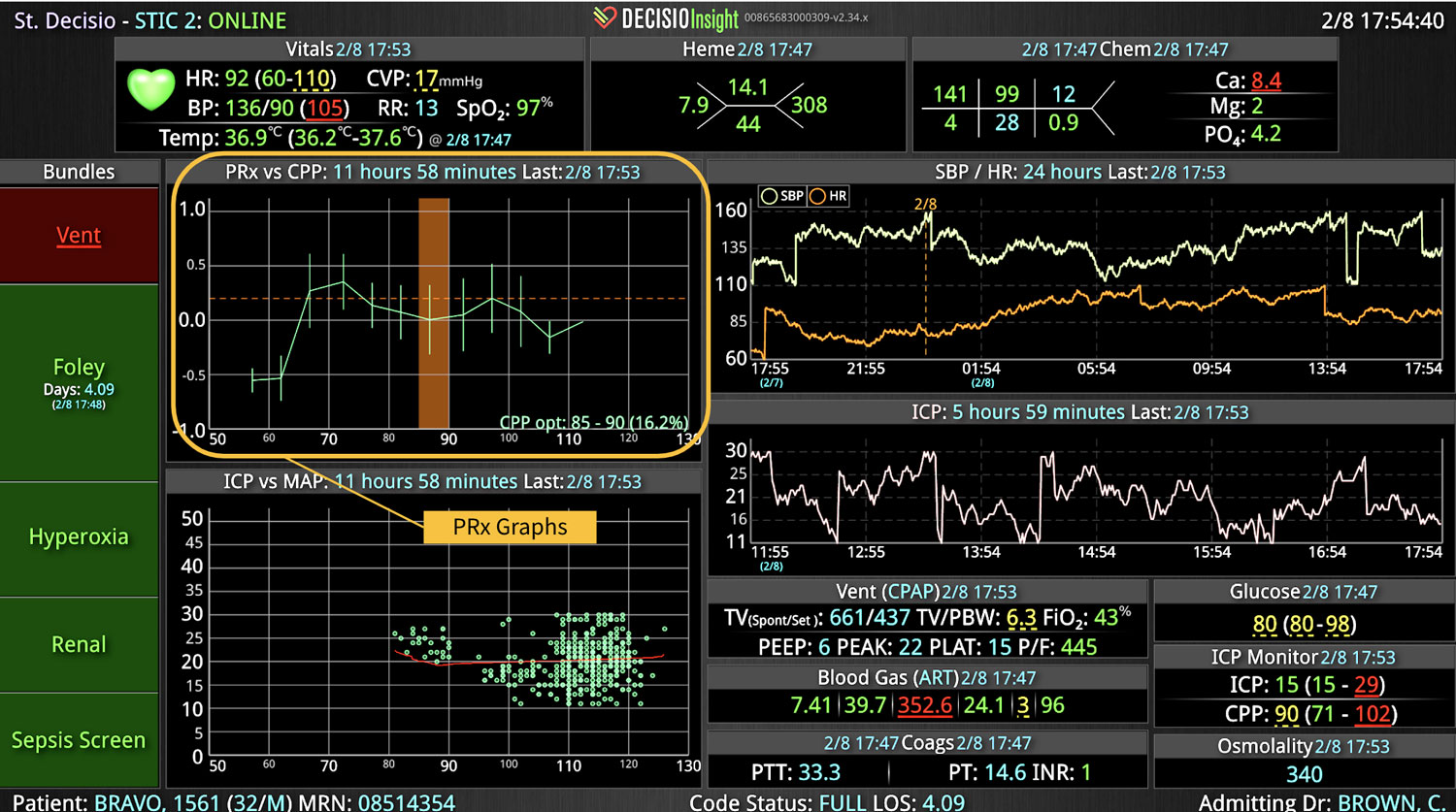
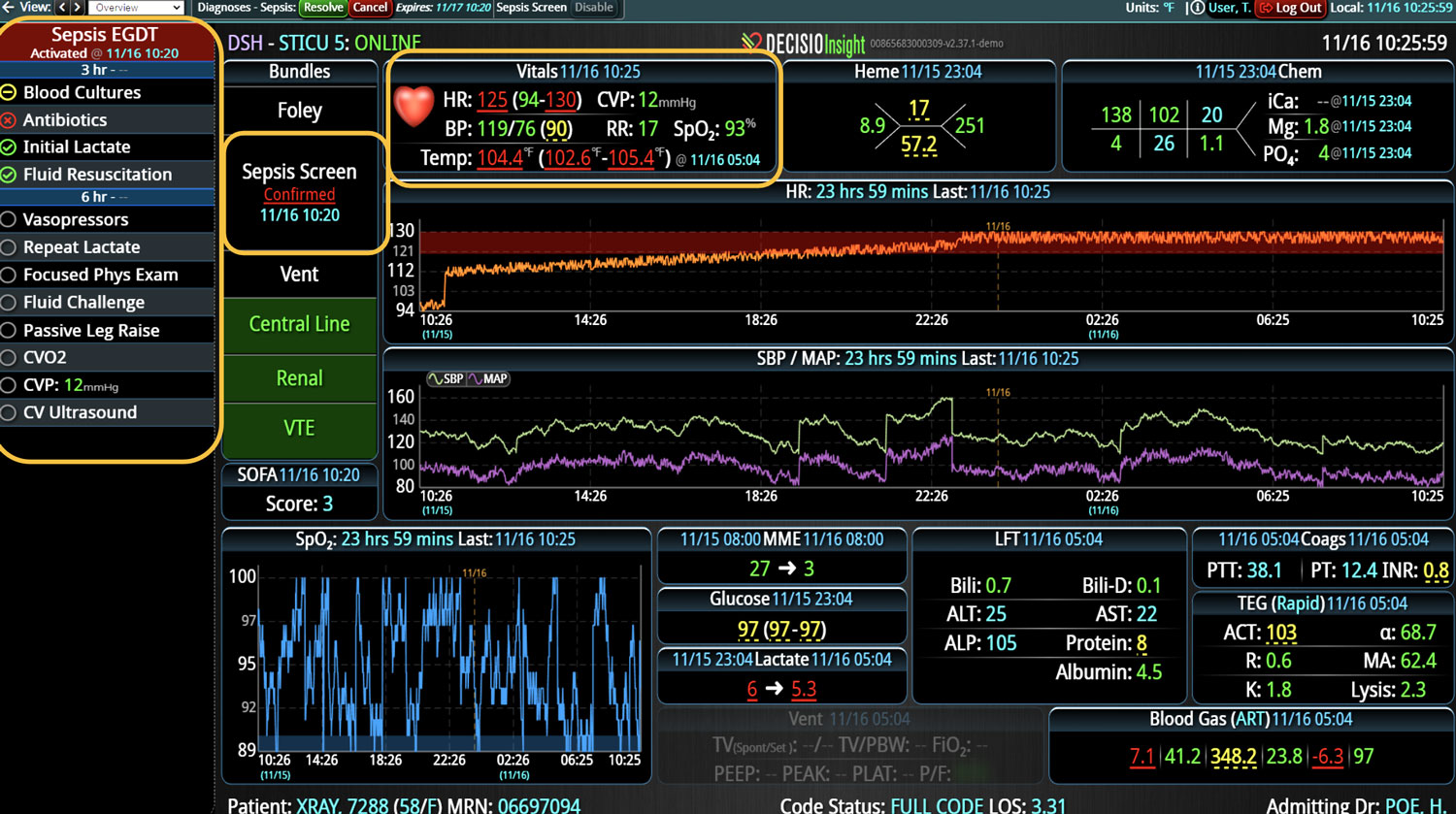
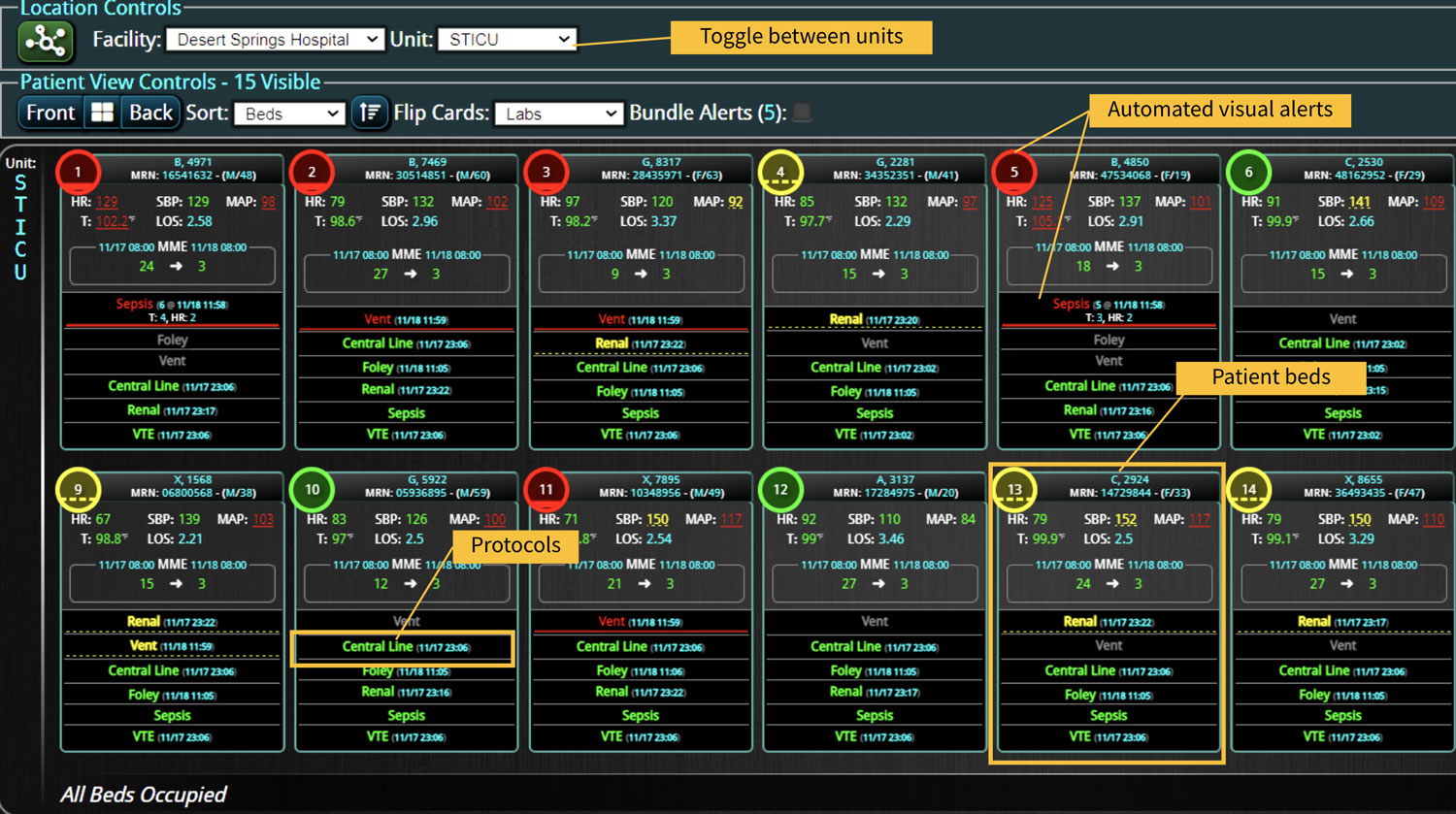
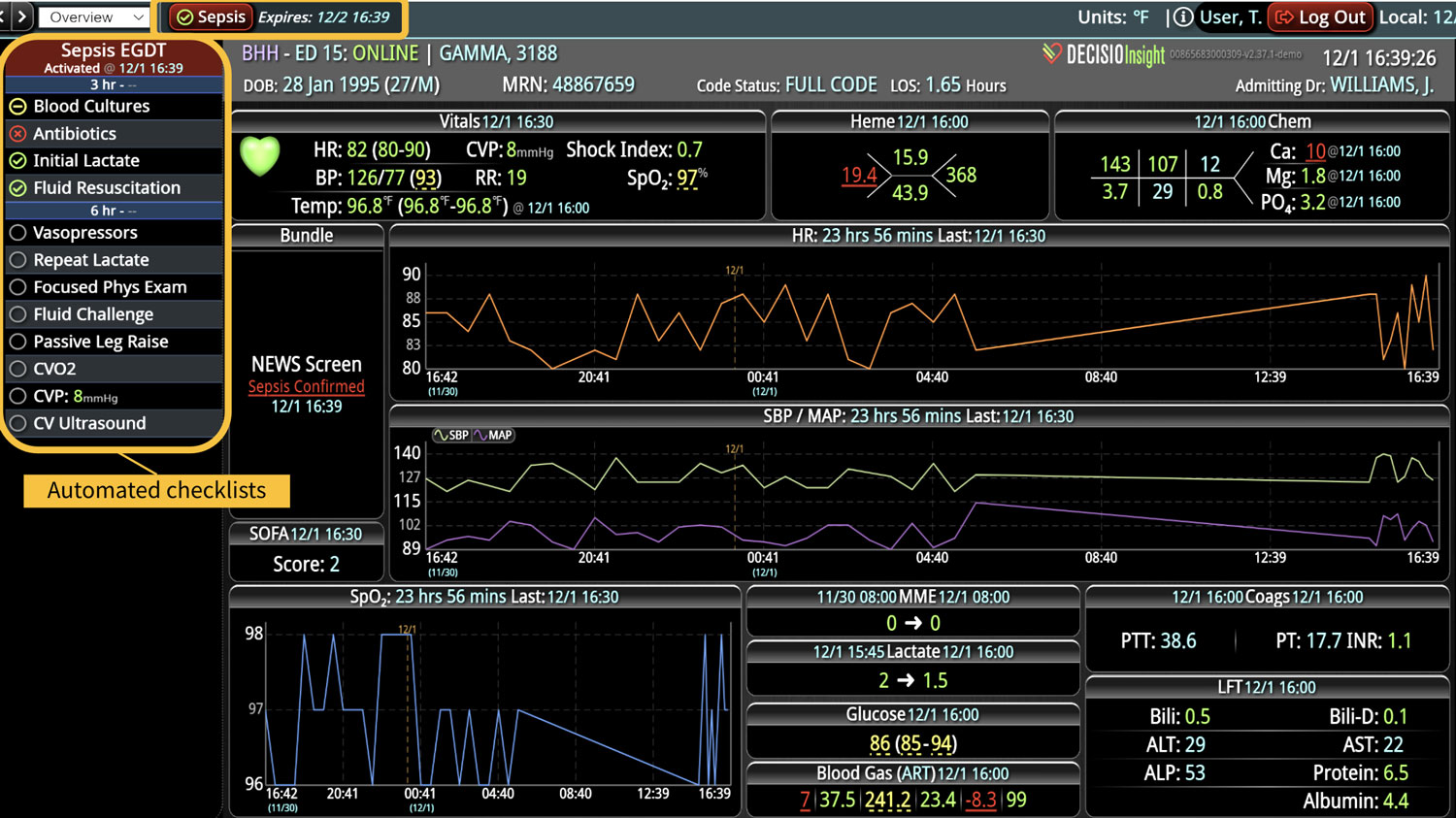
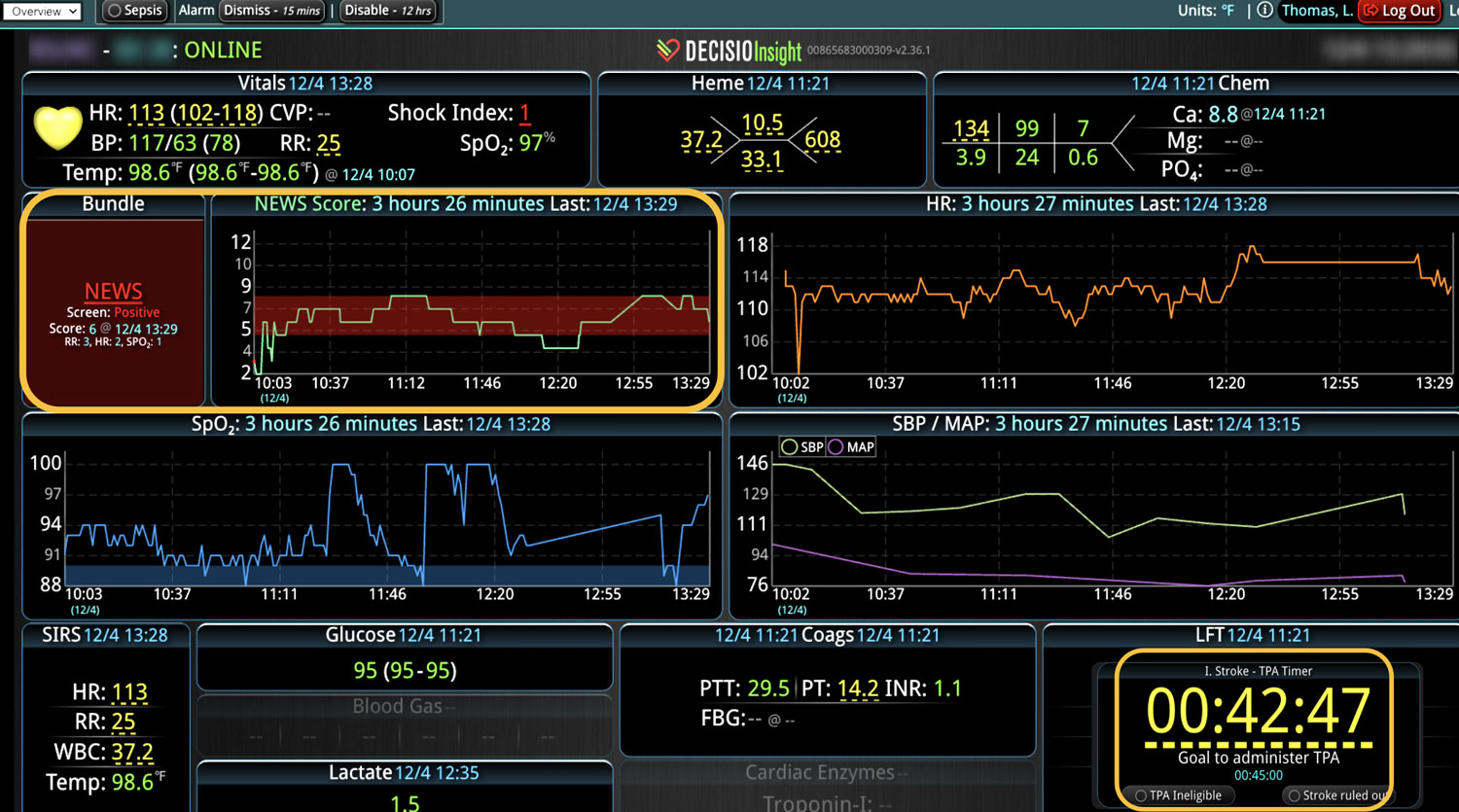
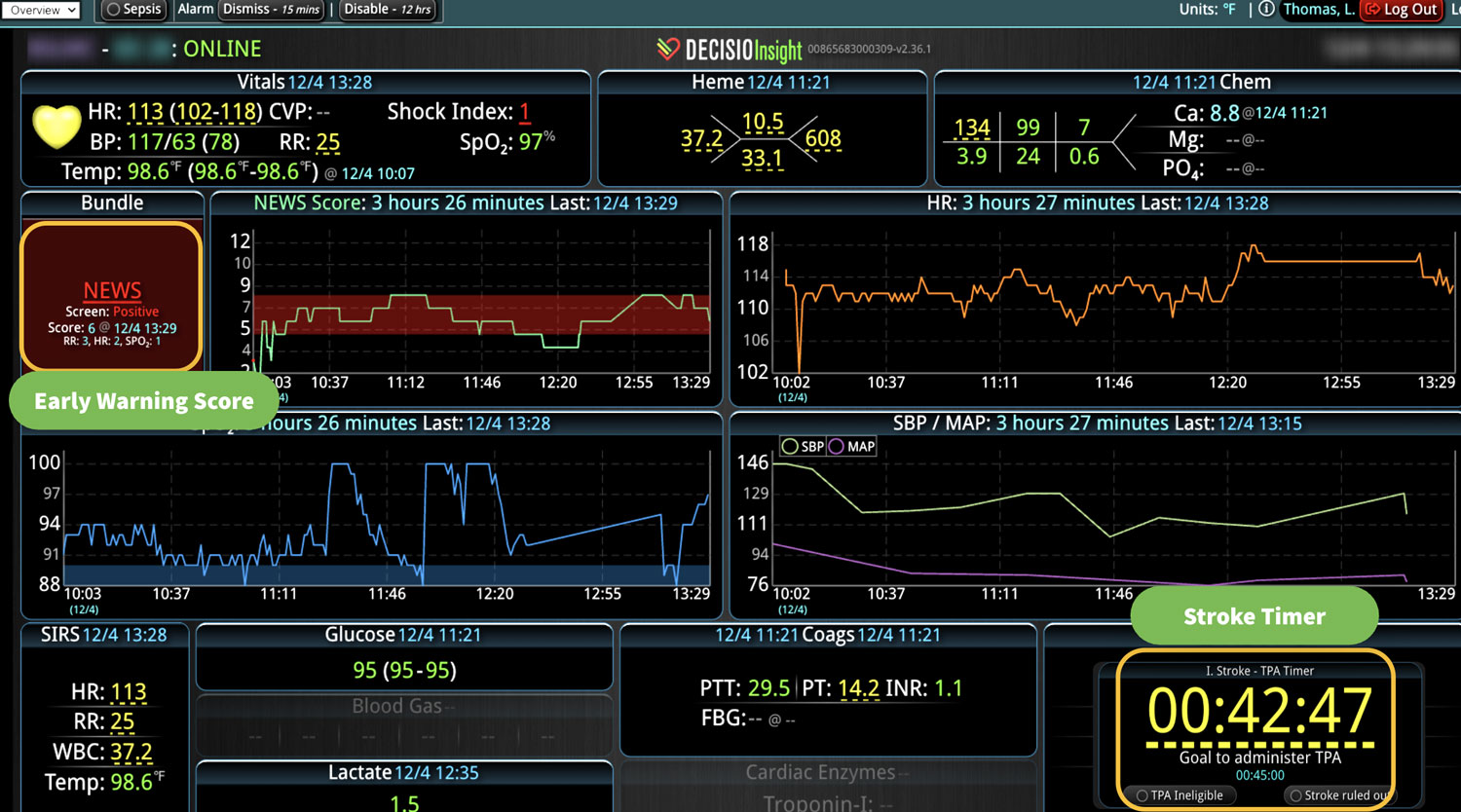
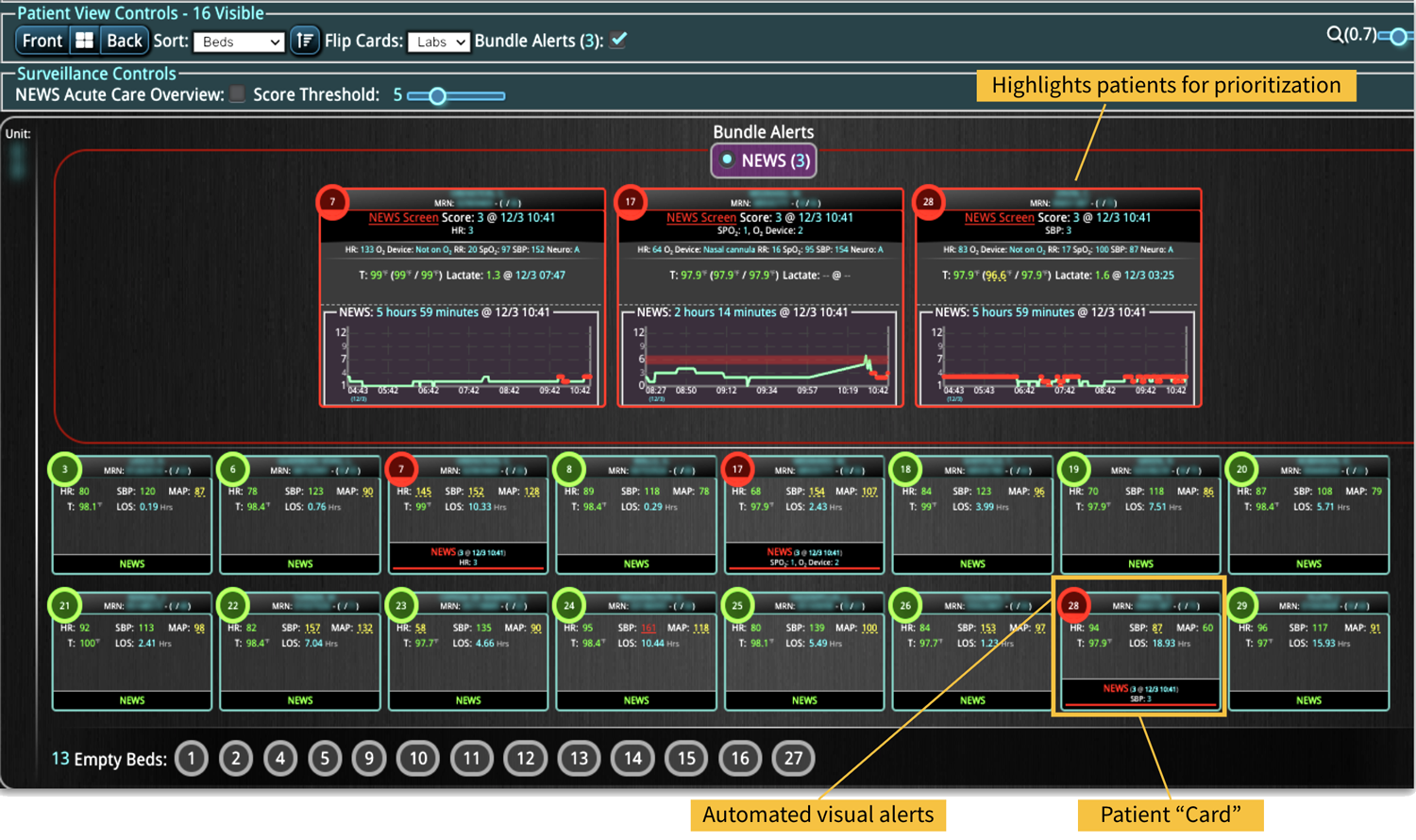
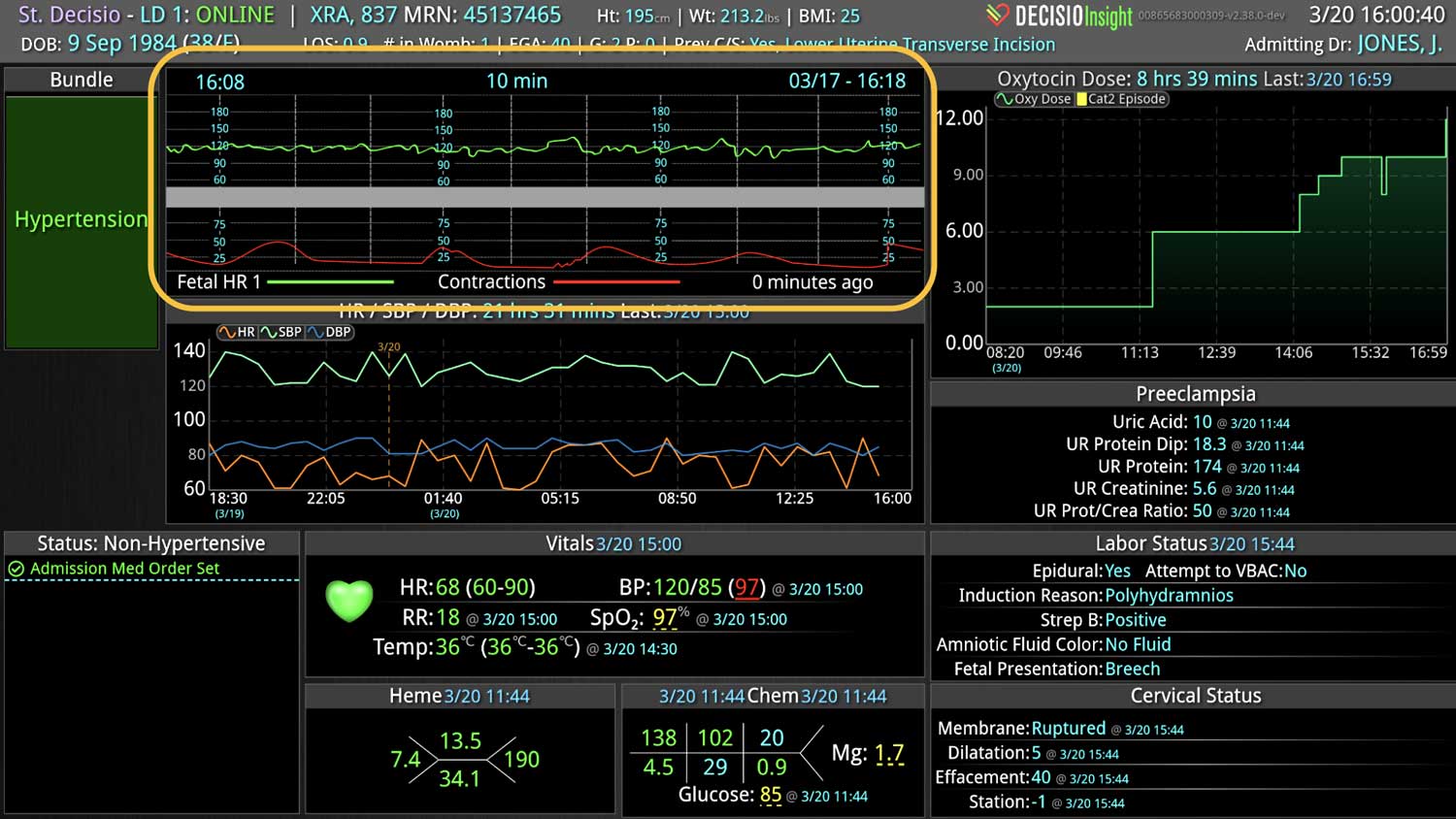
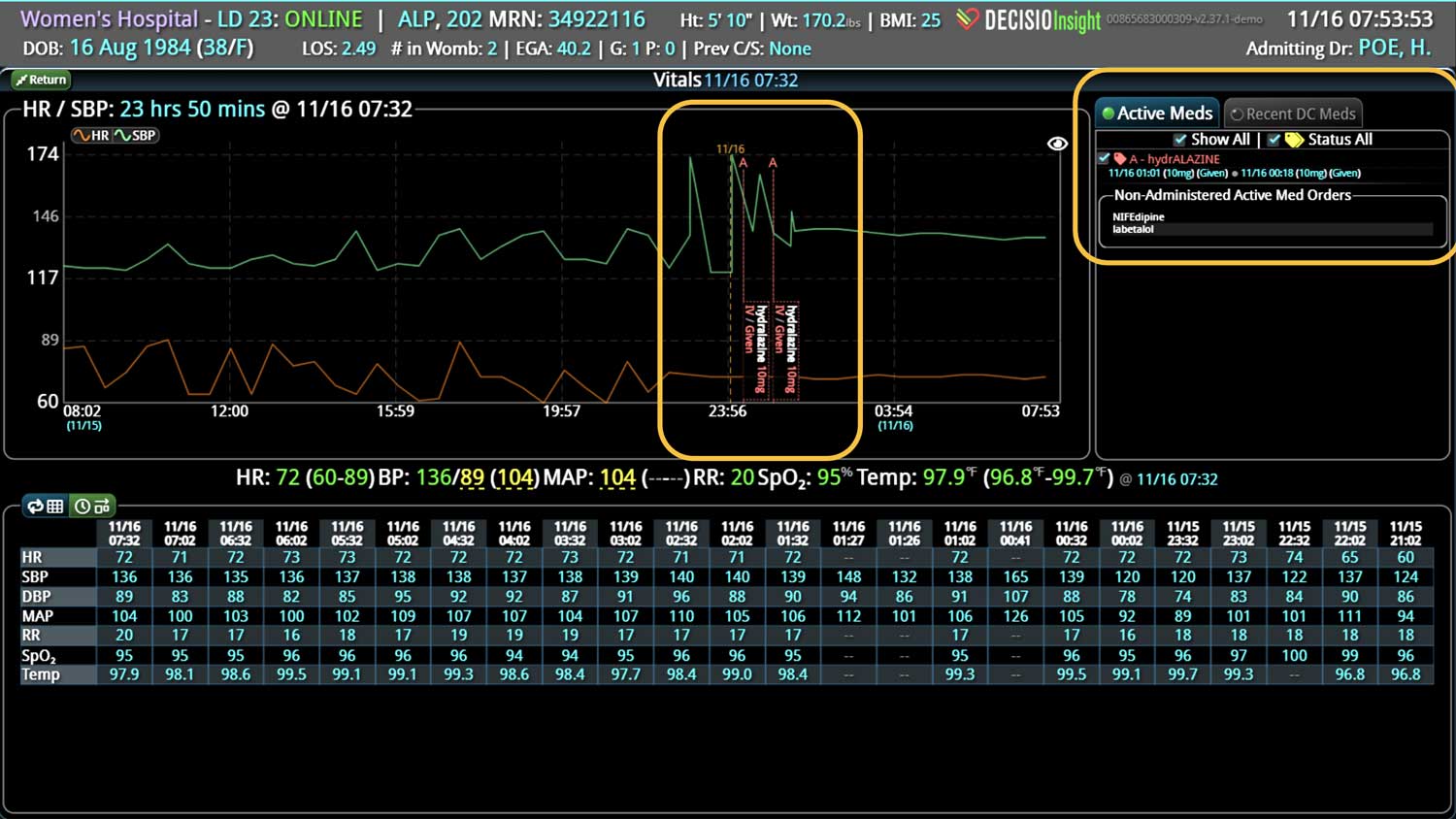
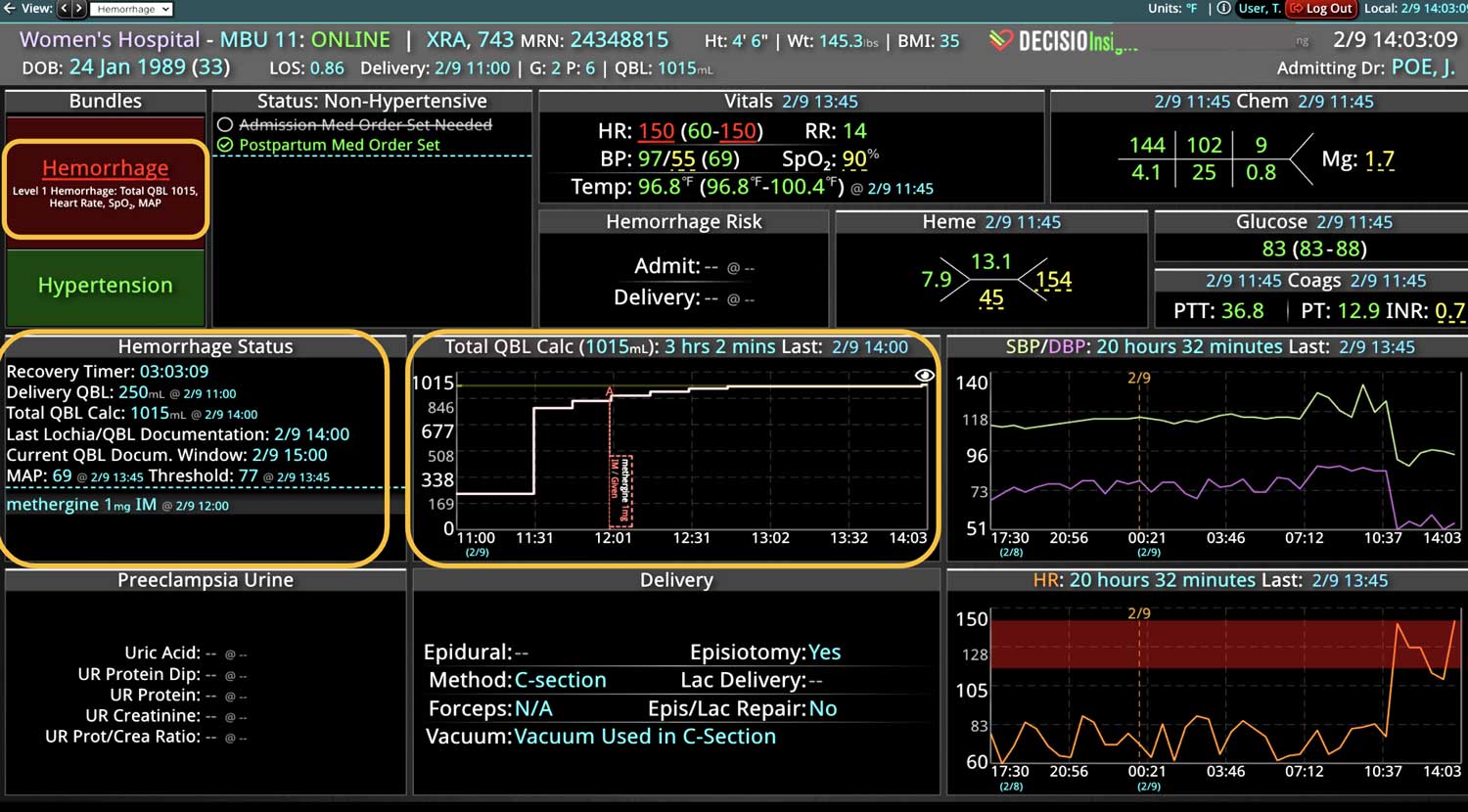
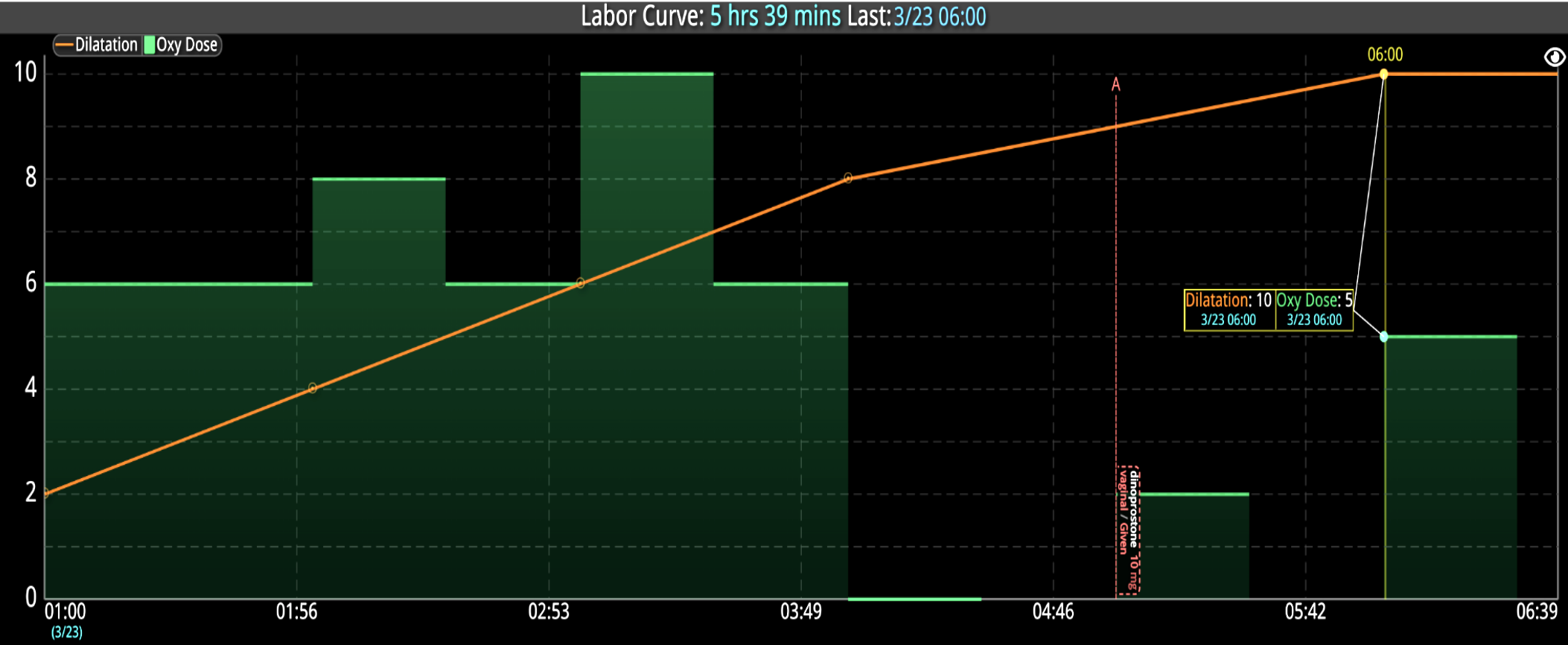
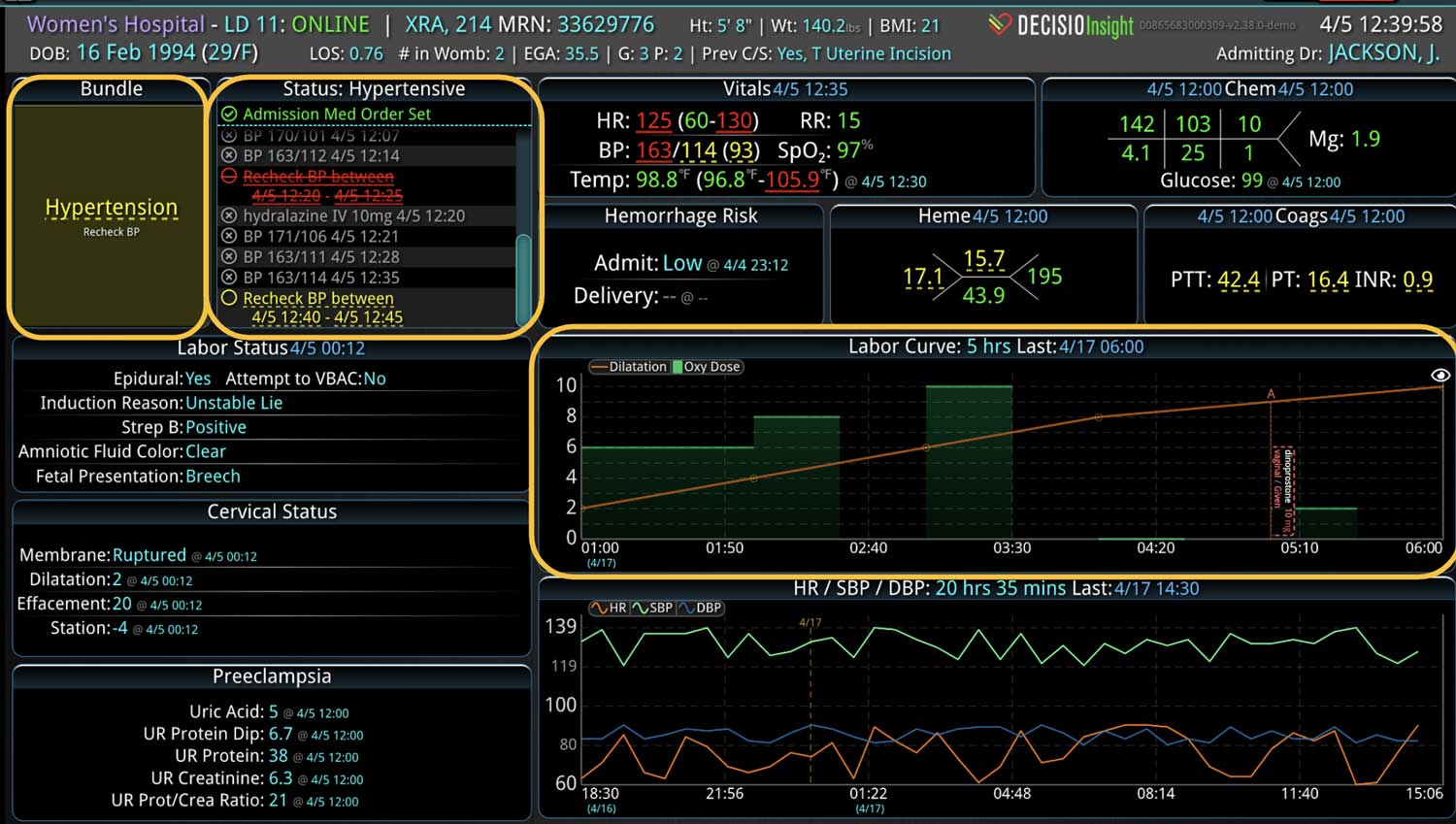
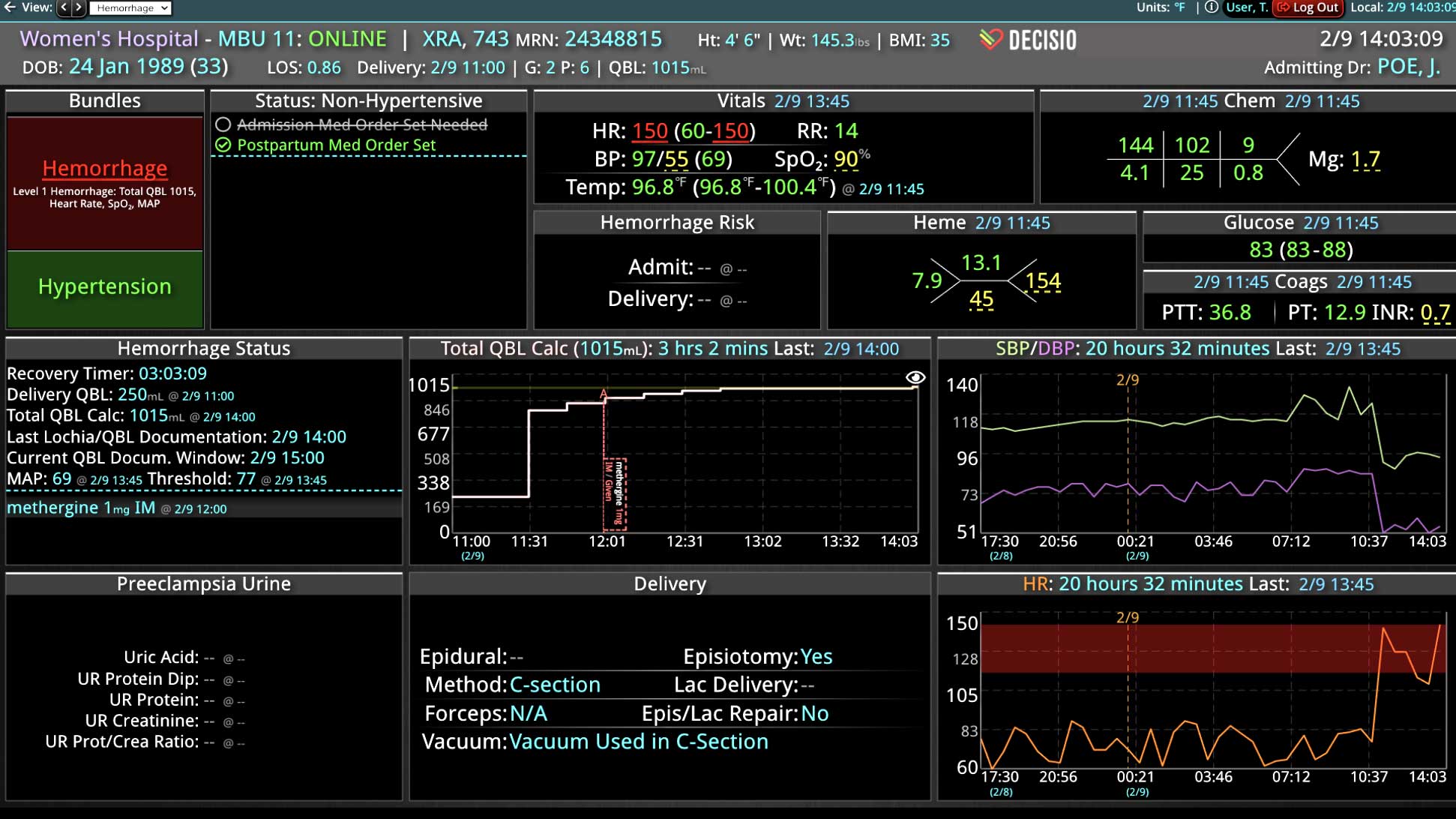
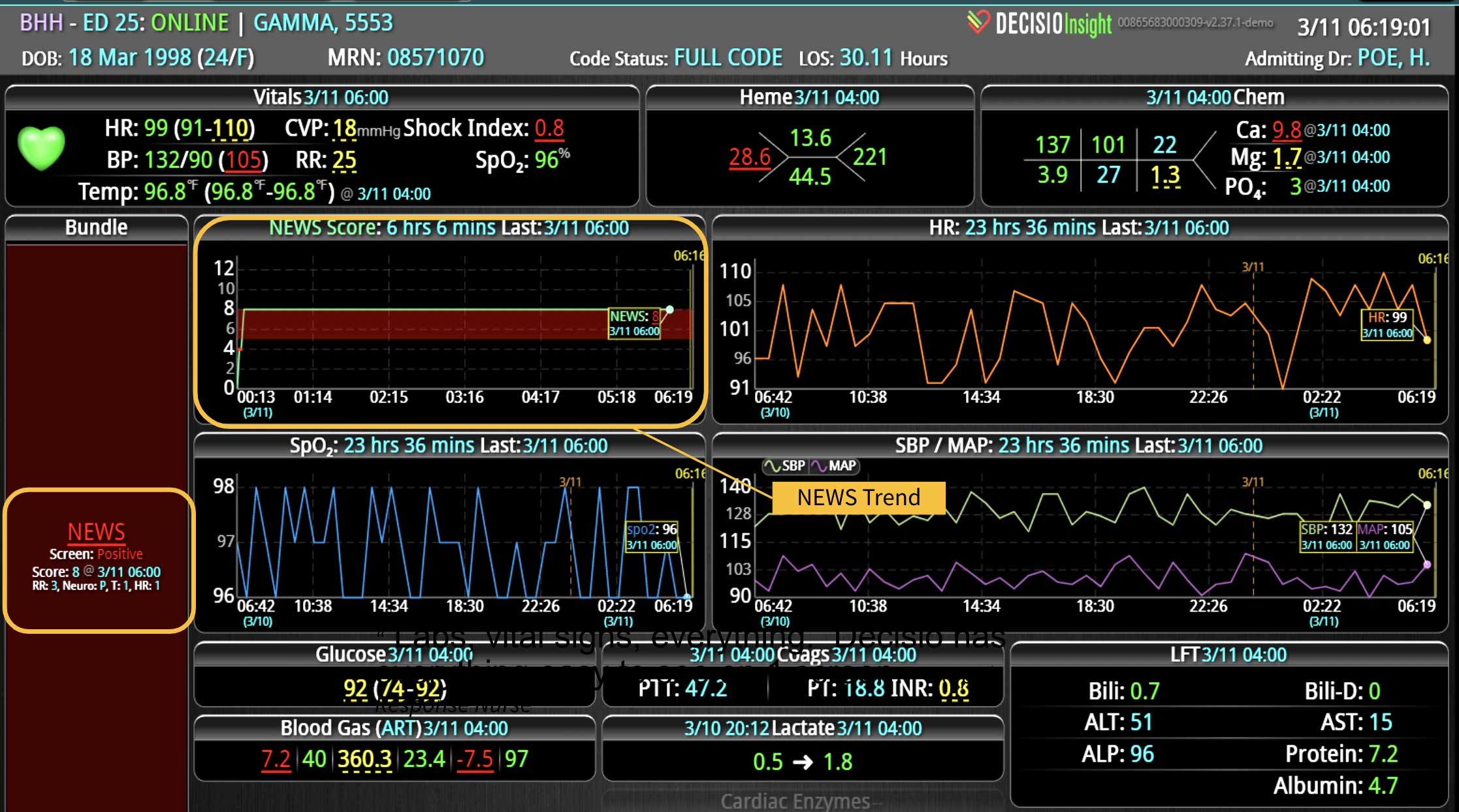
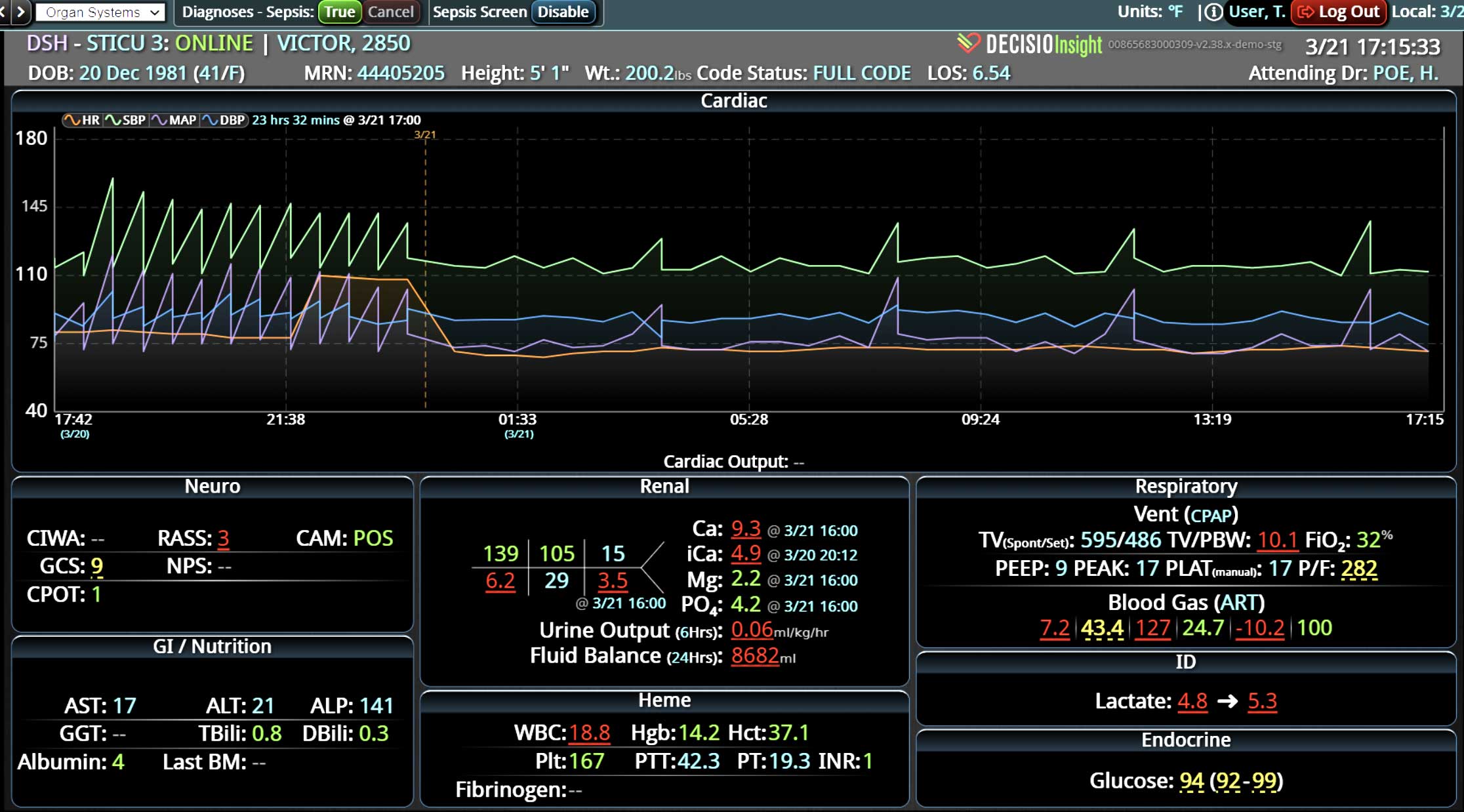
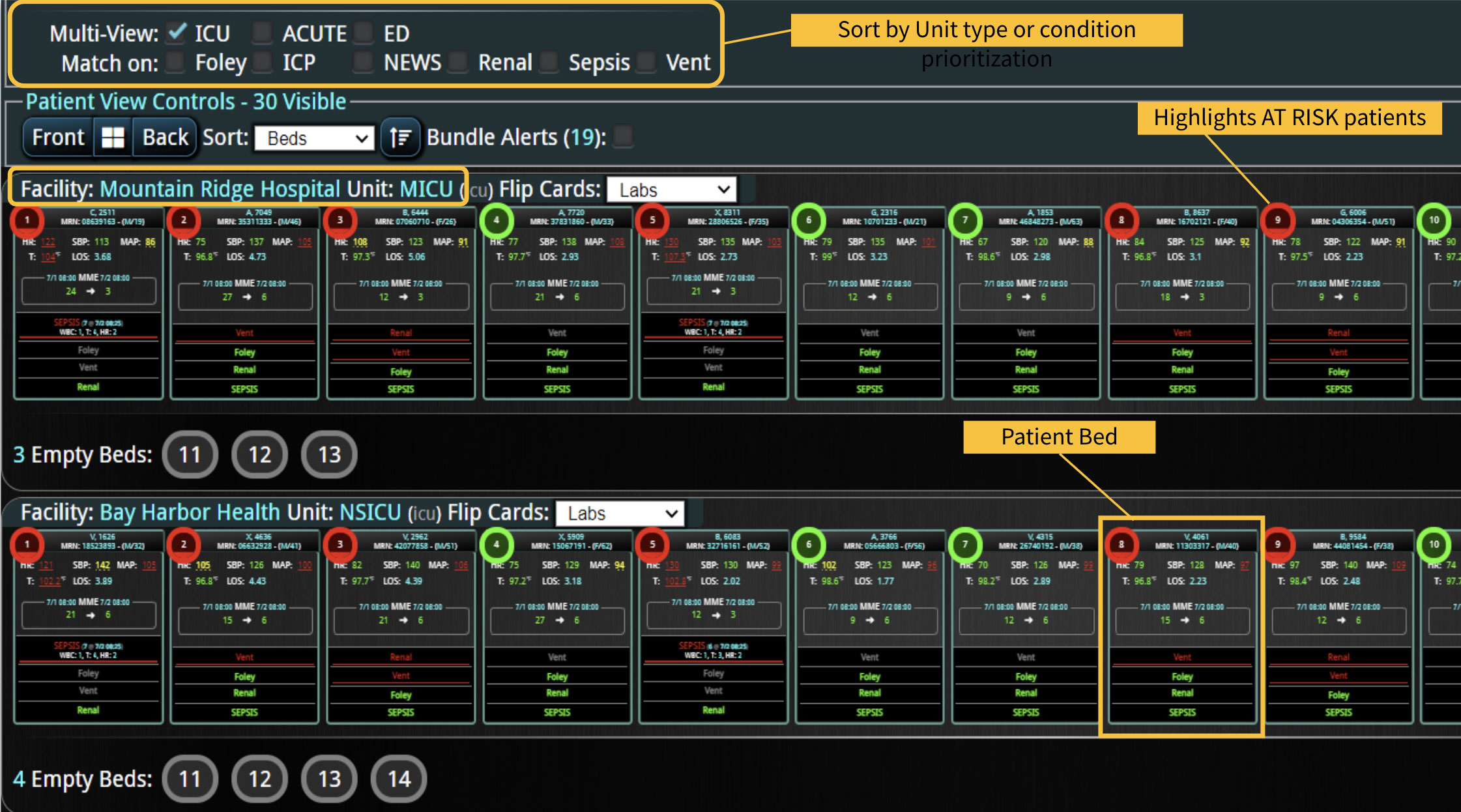
Historically at our institution (Baylor St. Luke’s Medical Center; Houston, TX, USA), rapid response teams (RRTs) respond to patient emergencies on the wards. Recently, in order to identify decompensating patients earlier, an innovative decision support software system was installed to alert RRTs to patient decompensation. In real-time, this software system continuously calculated a vital sign-based early warning score; once the score reached an abnormal threshold, the system alerted the RRTs to conduct a bedside evaluation. We analyzed data from patients who were transferred to an ICU within 24 hours of hospital ward admission from the ED. We compared data for four months before and after installing of the early warning, decision support software system.
Results
During the study period, 2.1% of ward admissions from the ED (n=46) in the pre-intervention period versus 2.8% (n=78) in the post-intervention period required transfer to the ICU within 24 hours (P=0.141). Hospital mortality rates for these patients decreased from 21.7% (n=10) in the pre-intervention period to 6.4% (n=5) in the post-intervention period (p=0.012).
Conclusions
These results demonstrate that utilization of this on time surveillance and decision support system resulted in a significant reduction in mortality rates for this specific high-risk group of ICU transfers.
Sources
1. Goldhill DR, Sumner A. Outcome of intensive care patients in a group of British intensive care units. Crit Care Med. 1998 Aug;26(8):1337-45.
2. Lundberg JS, Perl TM, Wiblin T, et al. Septic shock: an analysis of outcomes for patients with onset on hospital wards versus intensive care units. Crit Care Med. 1998 Jun; 26(6):1020-4.
3. Simchen E, Sprung CL, Galai N, Zitser-Gurevich Y, et al. Survival of critically ill patients hospitalized in and out of intensive care. Crit Care Med. 2007 Feb; 35(2):449-57.
4. Kennedy M, Joyce N, Howell MD, et al. Identifying Infected Emergency Department Patients Admitted to the Hospital Ward at Risk of Clinical Deterioration and Intensive Care Unit Transfer. Acad Emerg Med. 2010 October ; 17(10): 1080–1085
5. DeVita, et al. “Findings of the First Consensus Conference on Medical Emergency Teams”. Critical Care Medicine. Volume 34. Sept 2006.
6. McQuillan et al. “Confidential inquiry into quality of care before admission to intensive care”. BMJ 1998.
7. Solomon et al. “Effectiveness of rapid response teams on rates of in-hospital cardiopulmonary arrest and mortality: A systematic review and meta-analysis”. Journal of hospital medicine, 6/2016, issue 6.
8. Sprung CL, et al. Evaluation of triage decisions for intensive care admission. Critical Care Medicine 1999; 27:1073.
9. Hodgetts TJ, et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation 2002; 54:115.