08 Apr Clinical Outcomes in Septic Patients after Implementing a Visual Clinical Decision Support System

Clinical Outcomes in Septic Patients after Implementing a Visual Clinical Decision Support System
Background
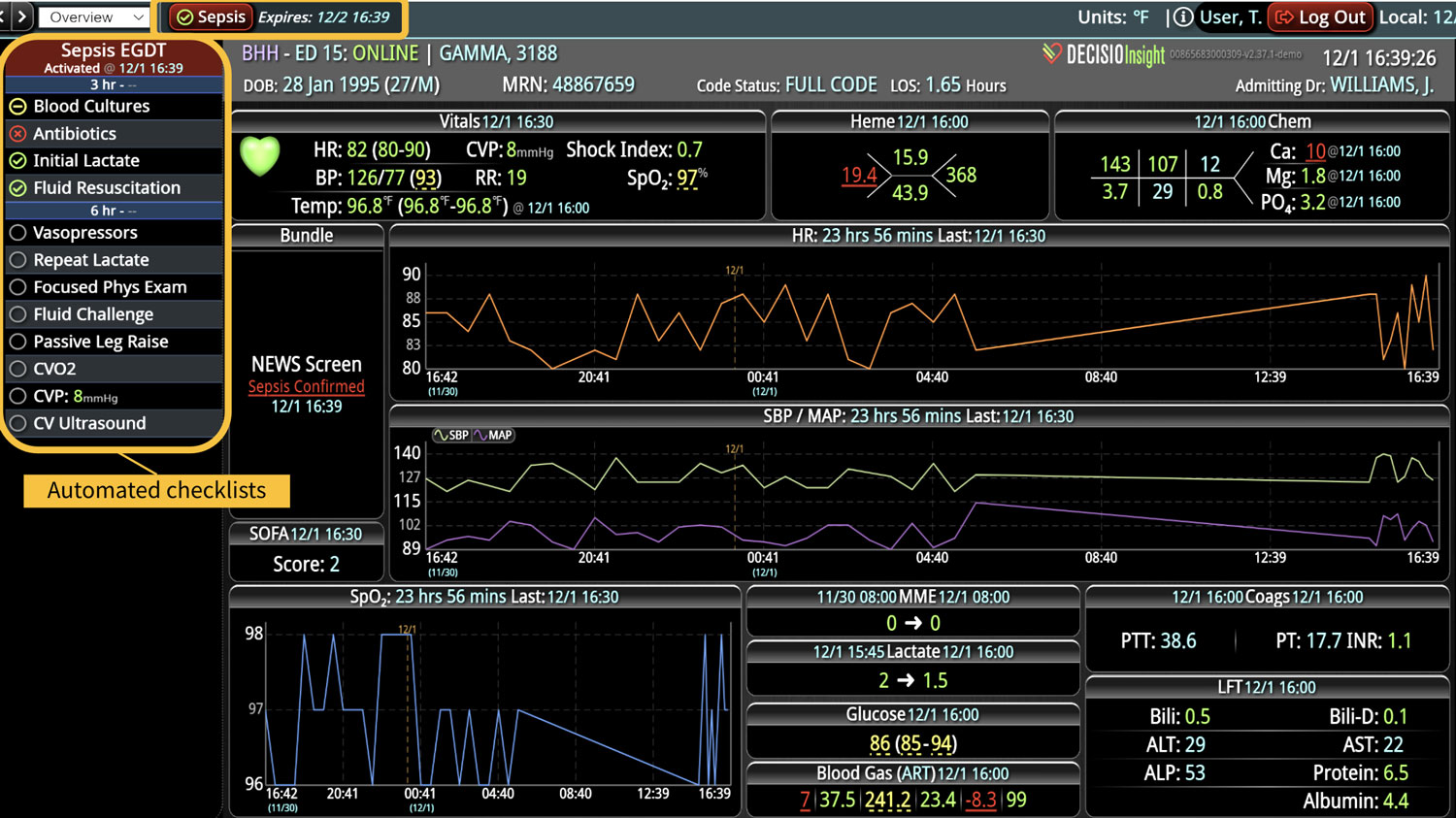
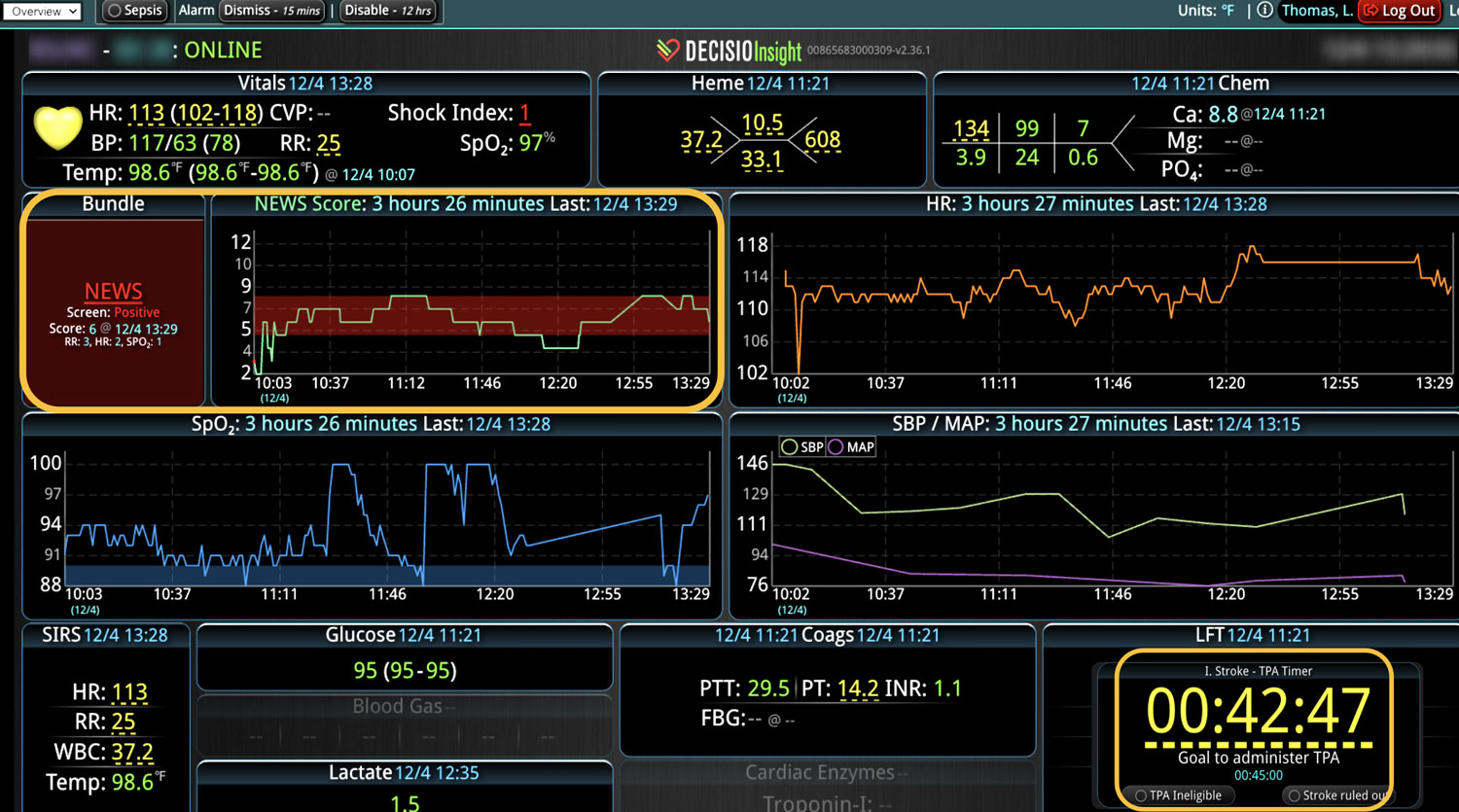
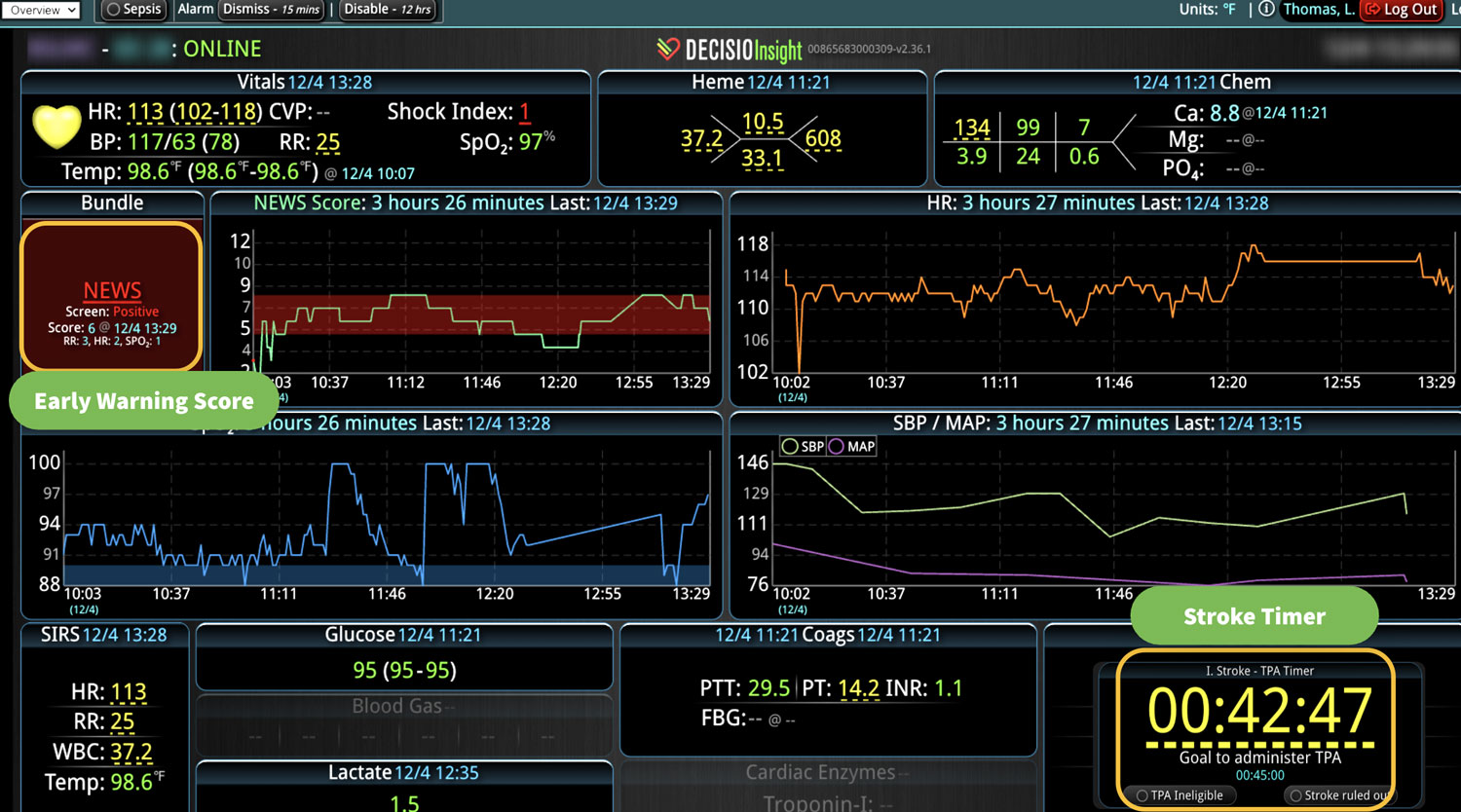
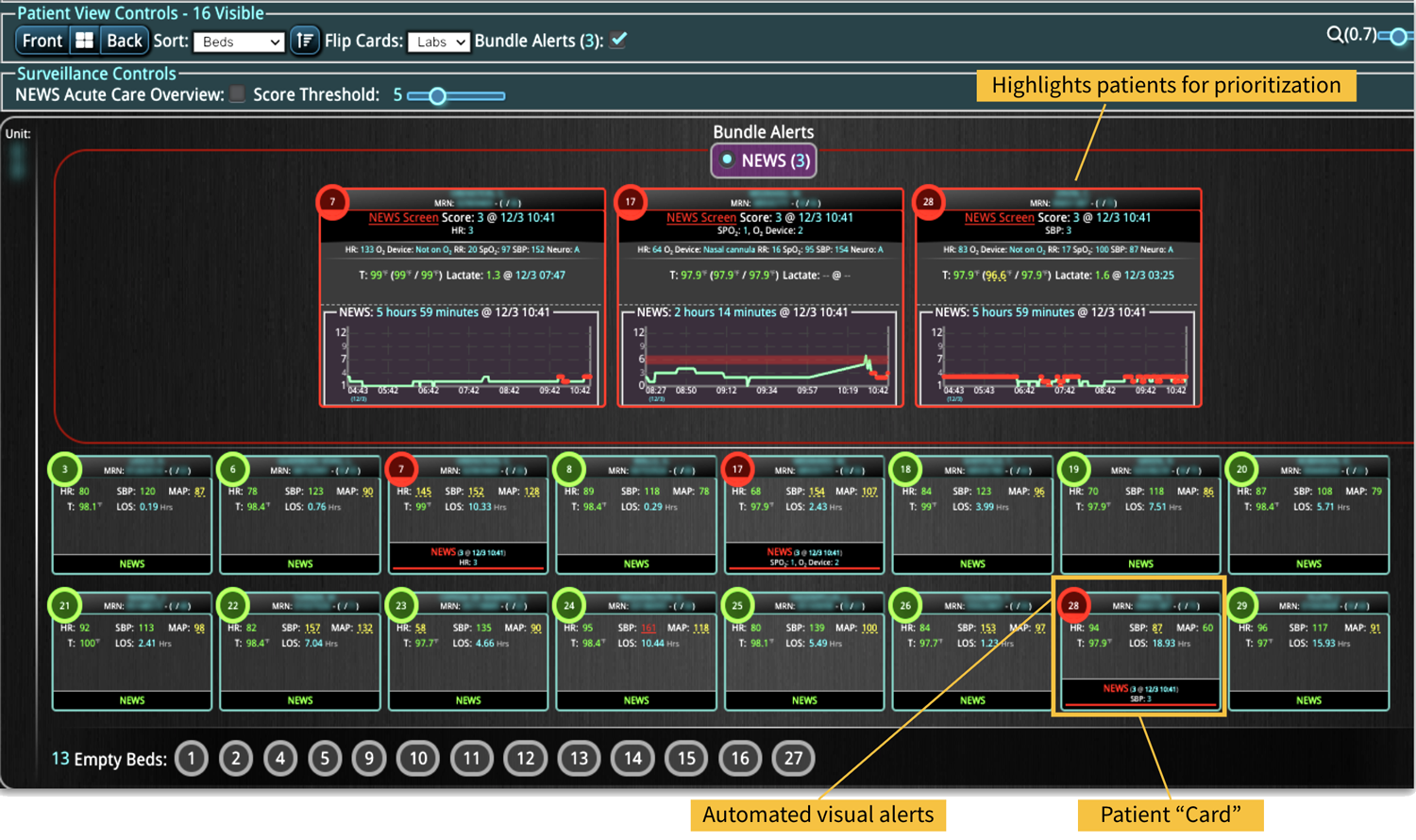
Sepsis is a leading cause of death in hospitalized patients. Frequent sepsis screening coupled with early diagnosis and intervention is key to improving outcomes. Electronic health records (EHRs) store vast amounts of data, but accessing and visualizing clinically relevant data can be cumbersome. New clinical decision support tools can automatically screen patients and display visual alerts using data already contained within the EHR, enabling earlier diagnosis and treatment of patients. We hypothesized that implementing of a bedside clinical surveillance visualization system in the intensive care environment would be associated with a decreased mortality of septic patients.
Methods
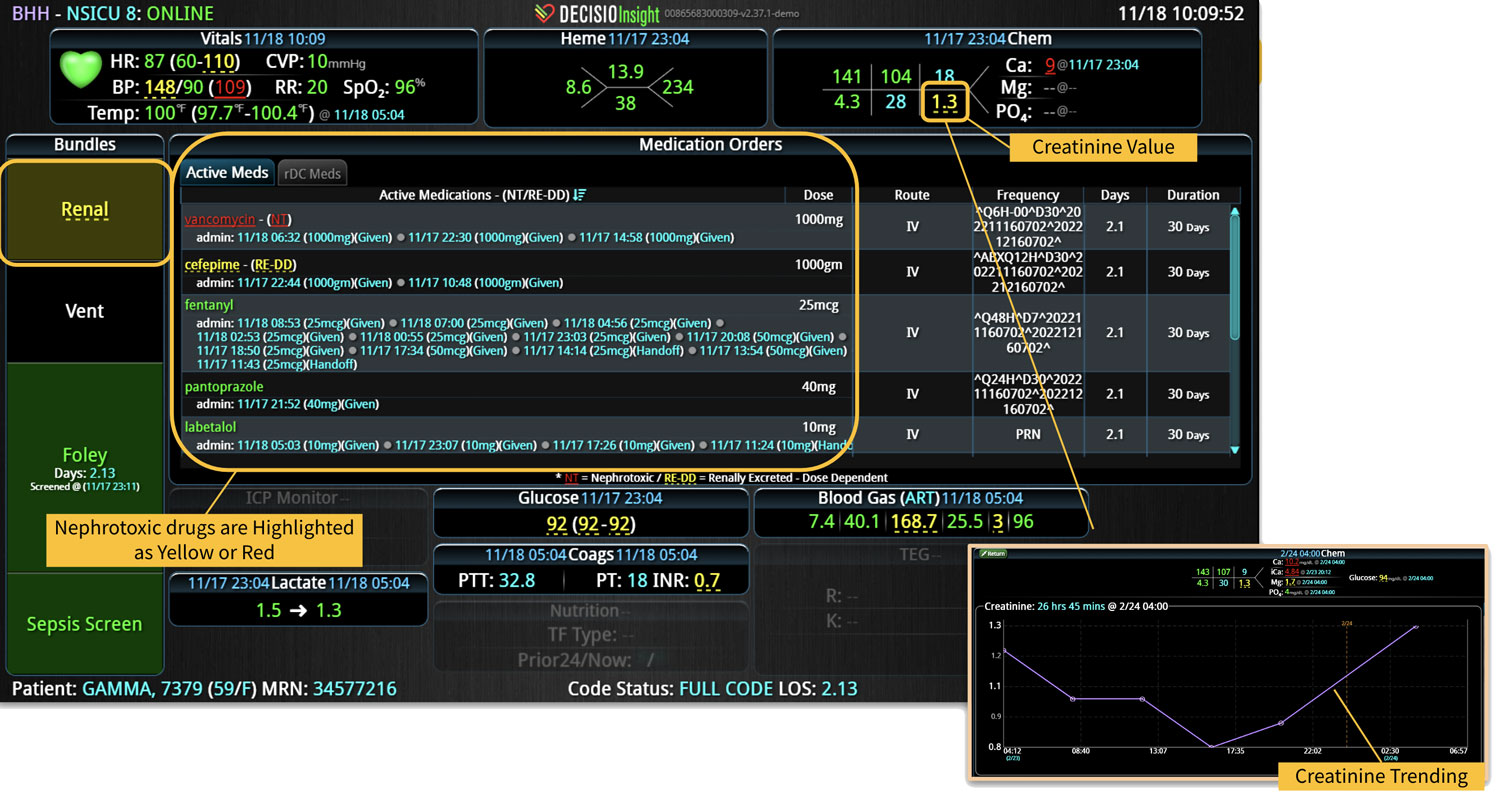
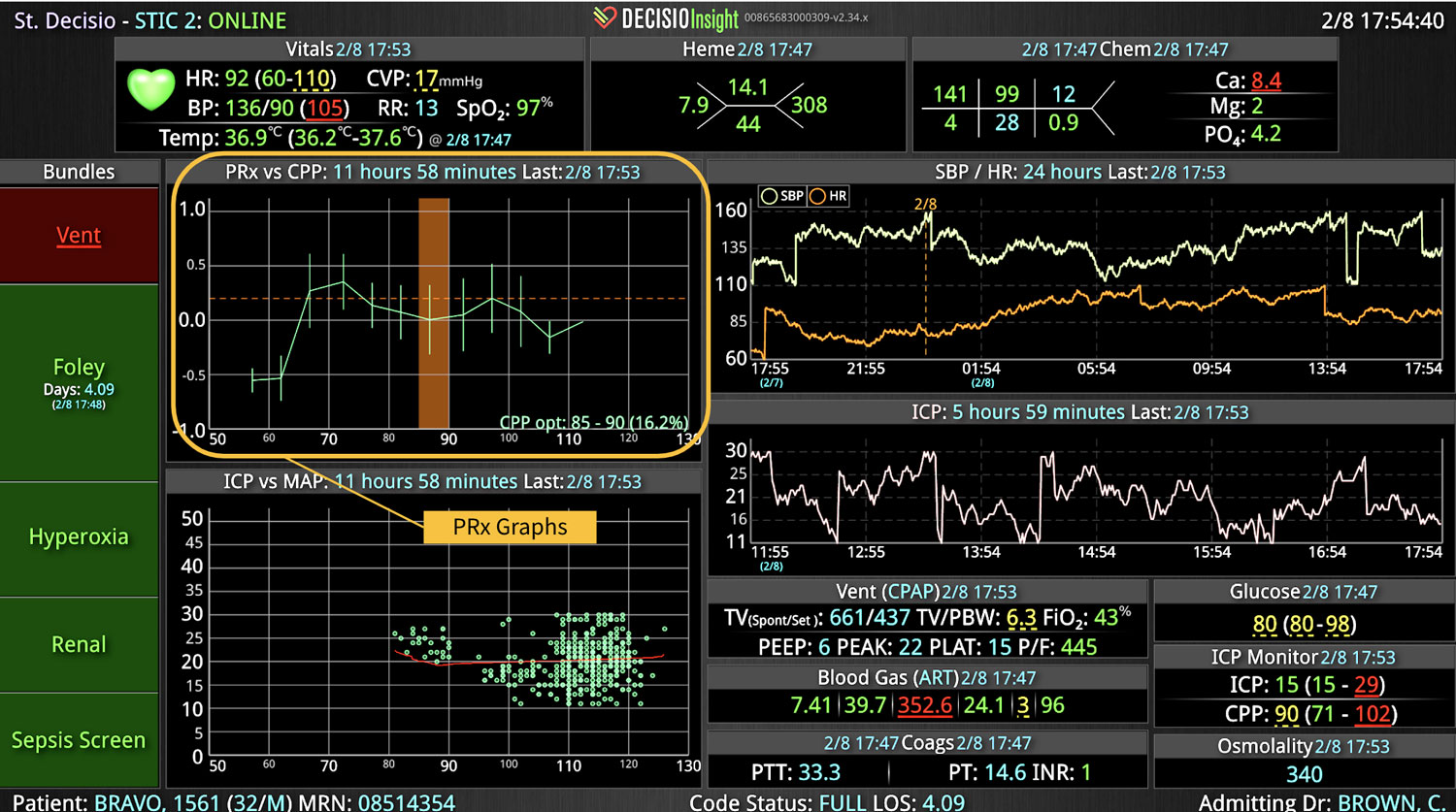
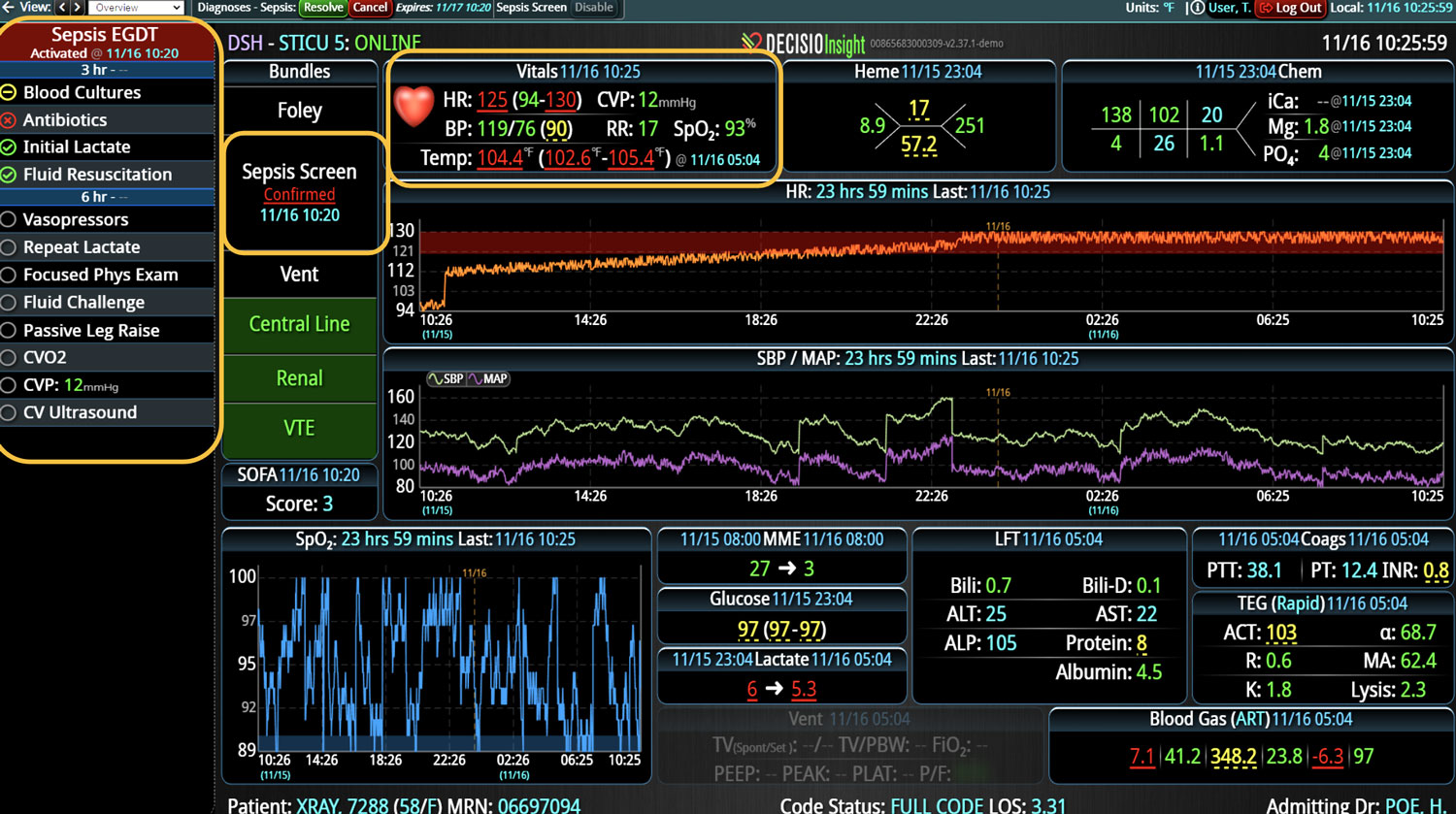
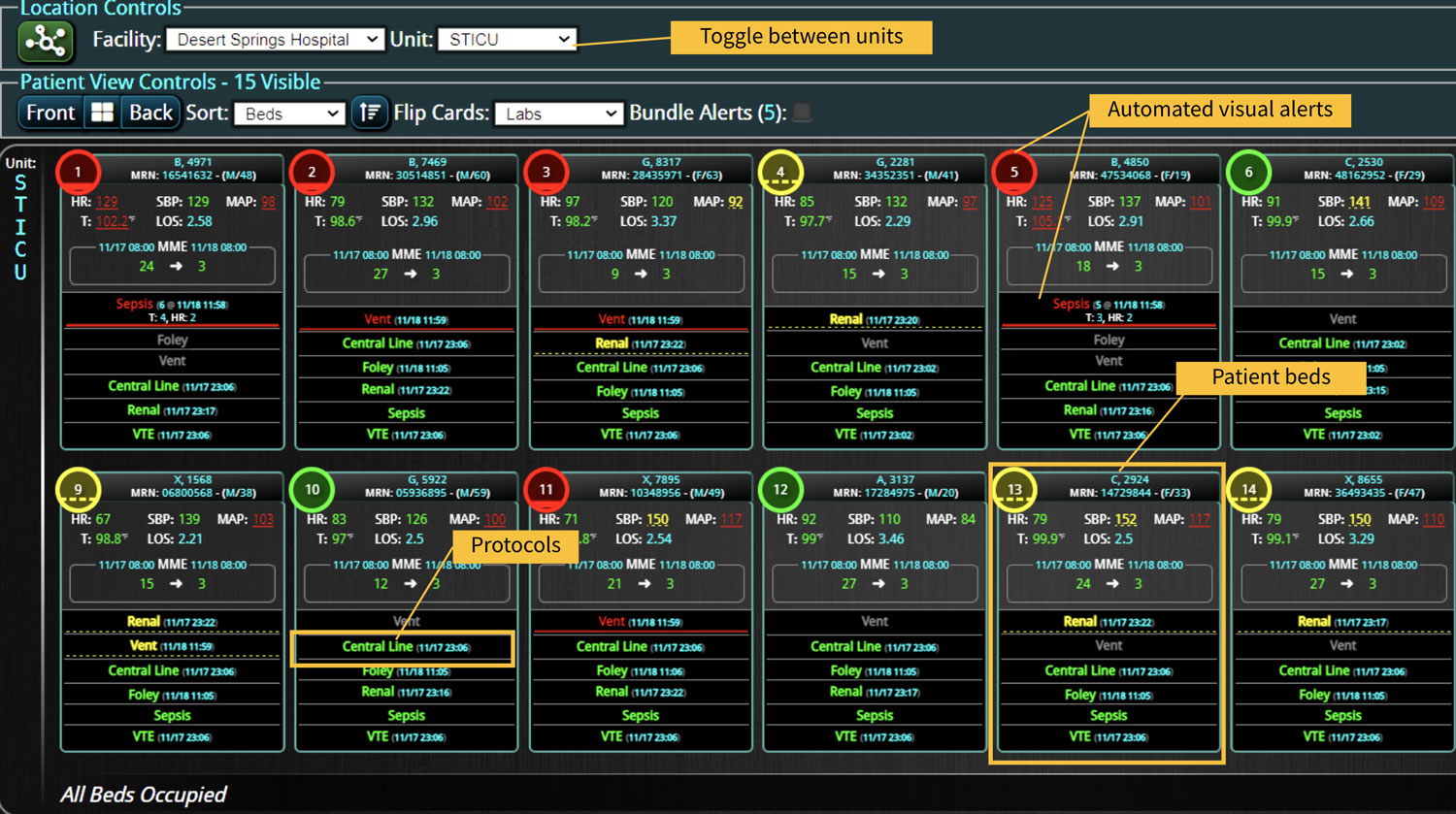
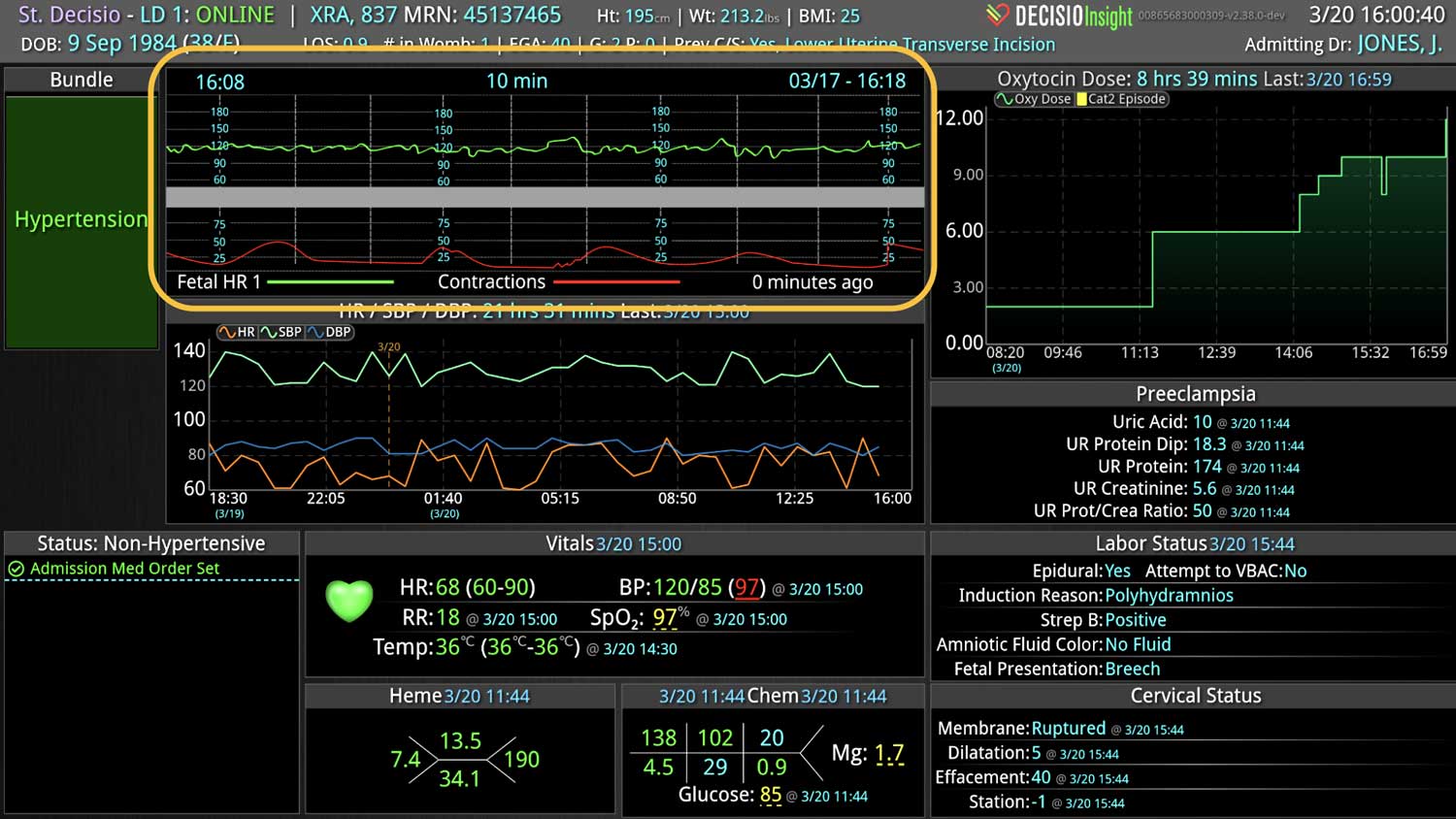
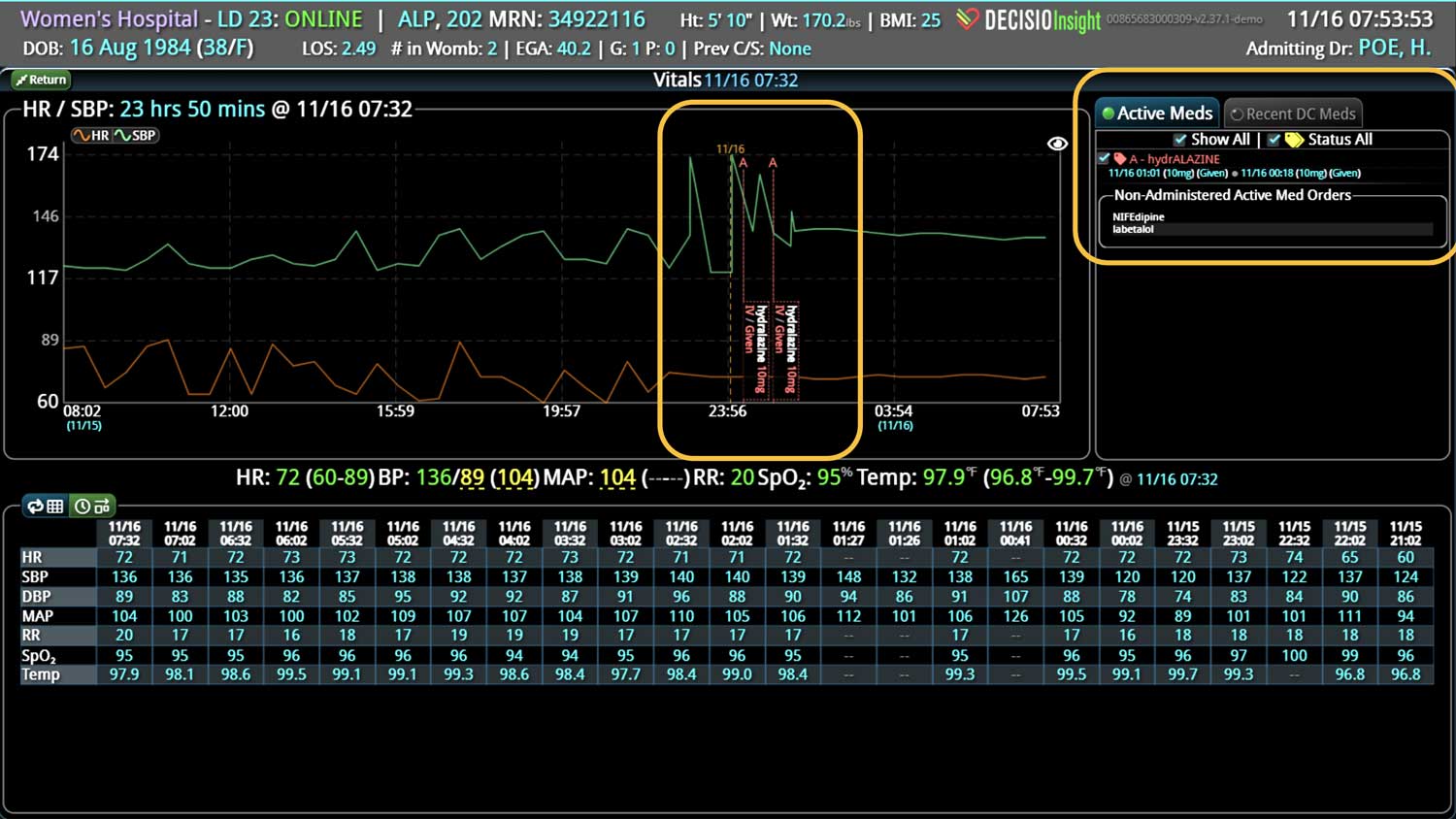
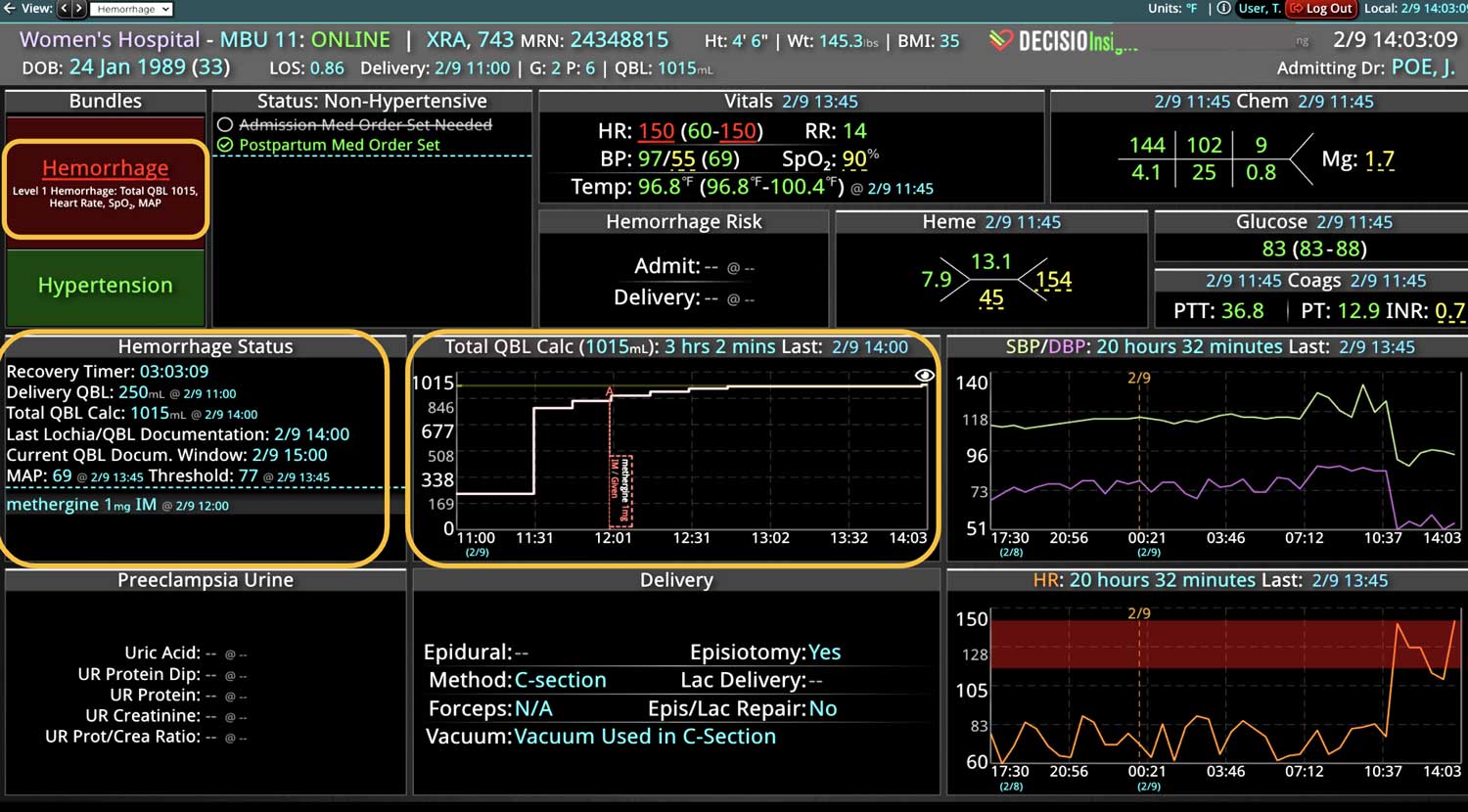
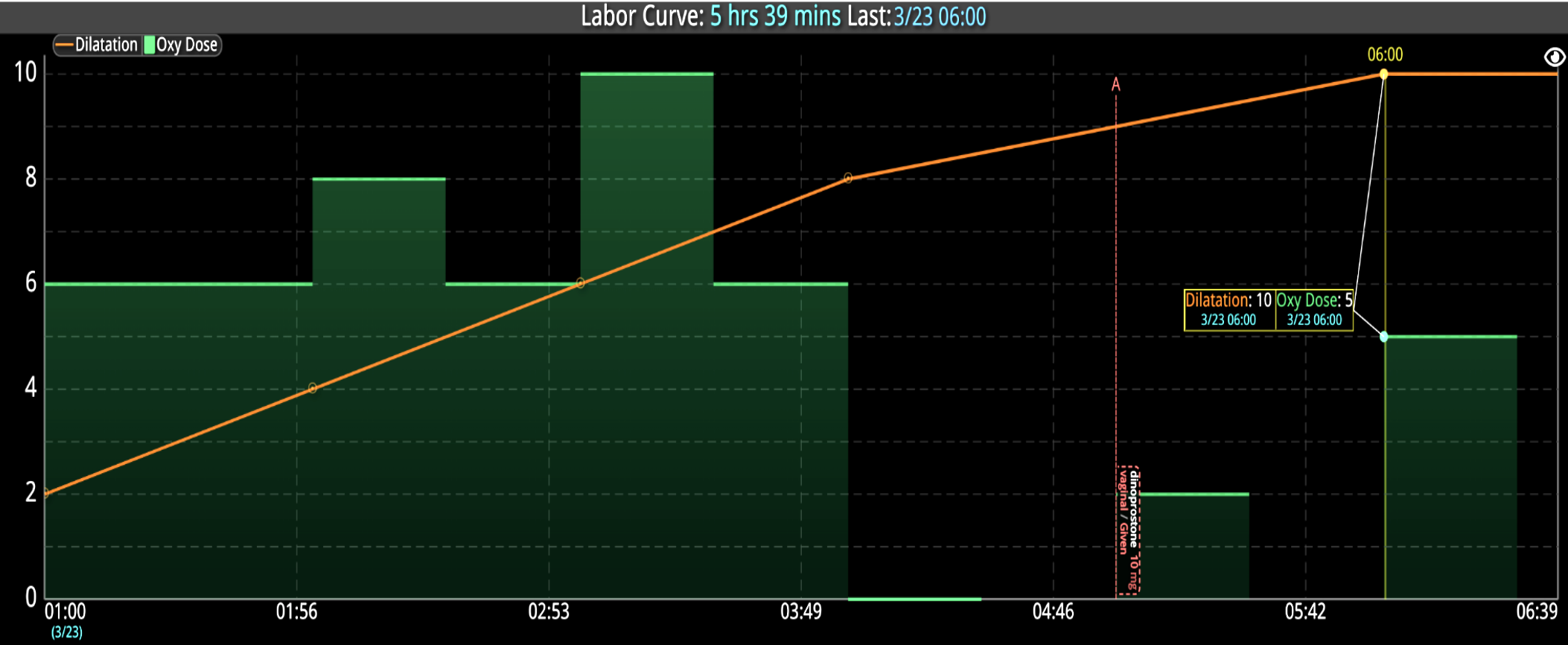
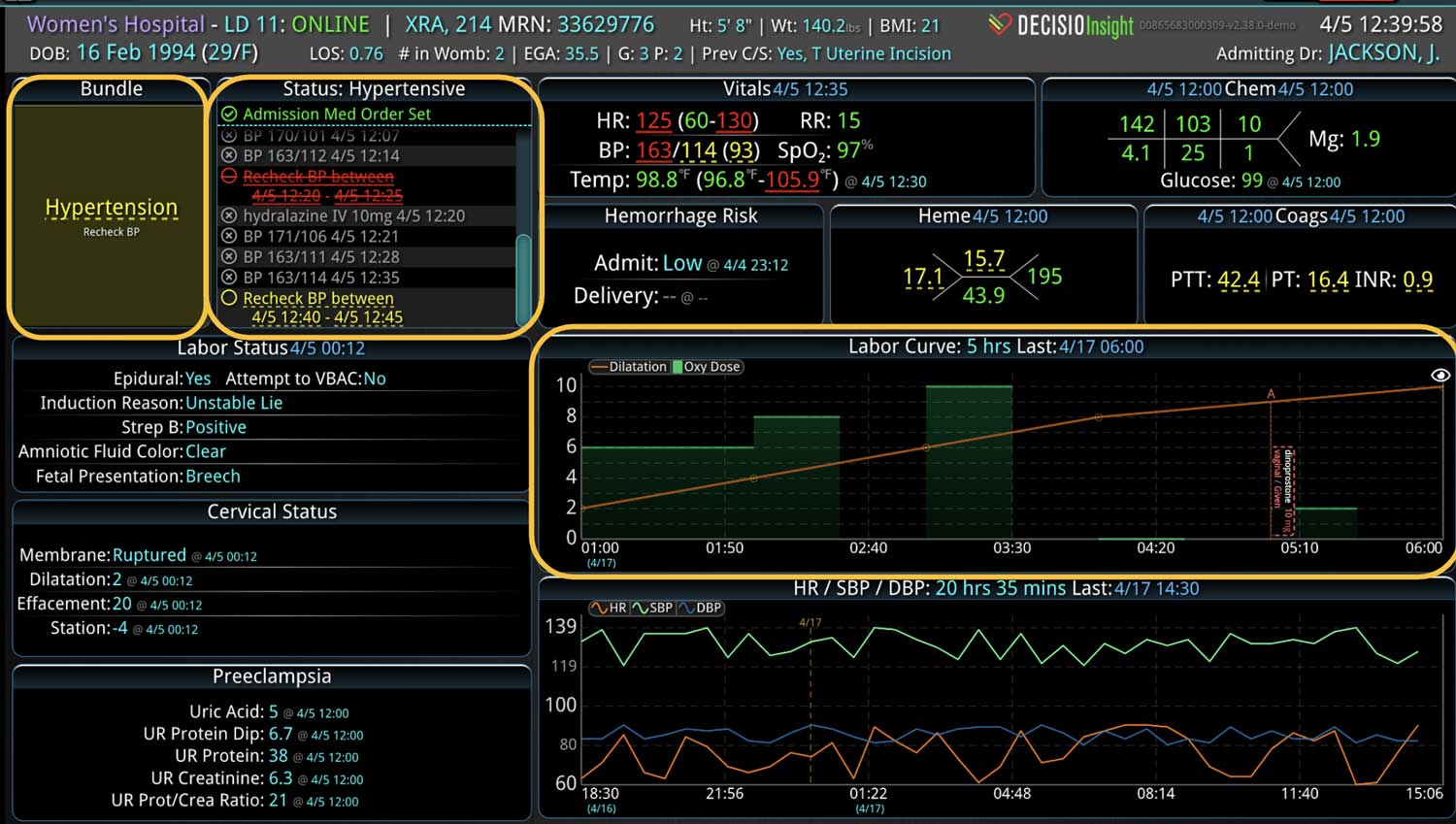
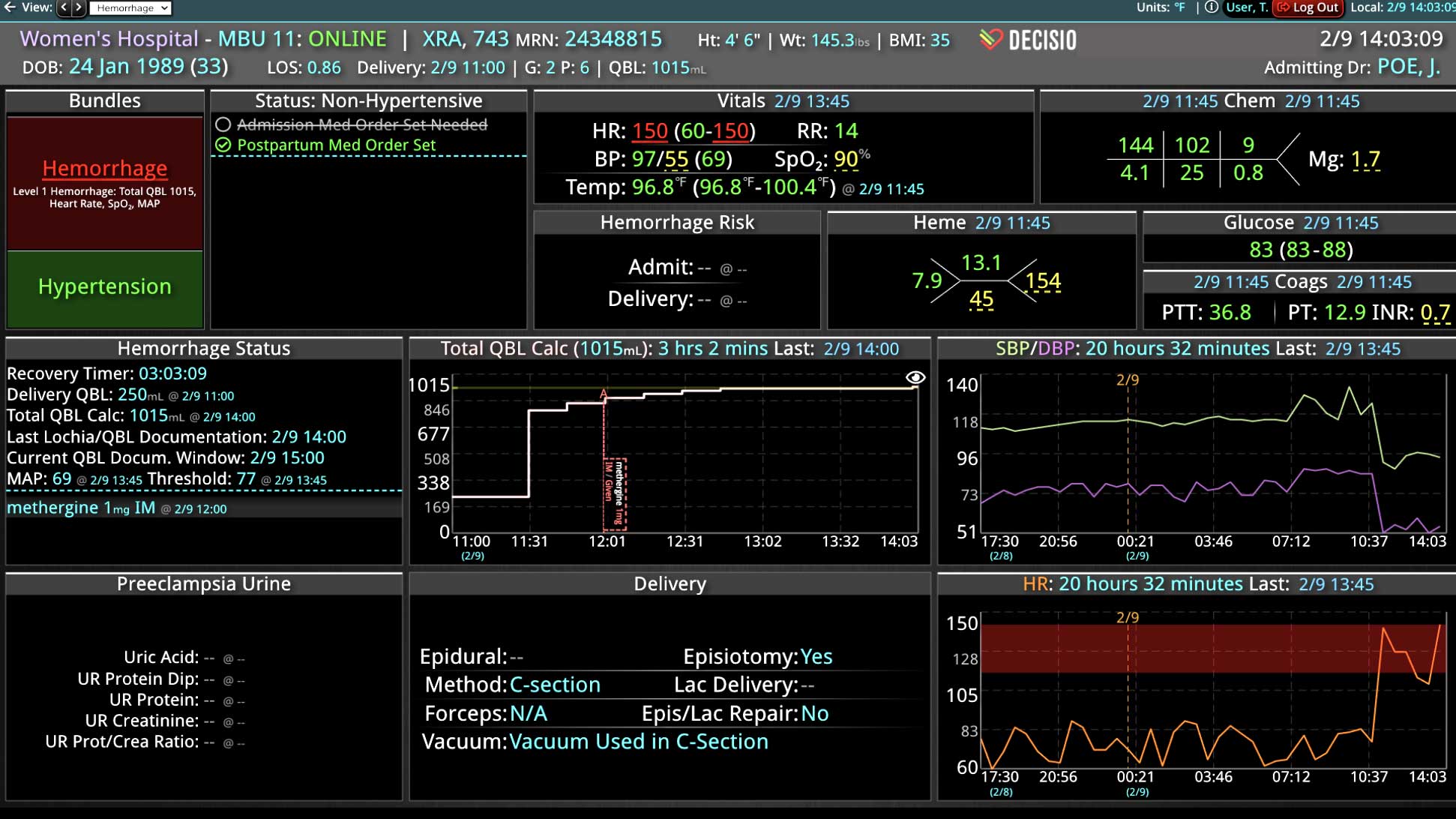
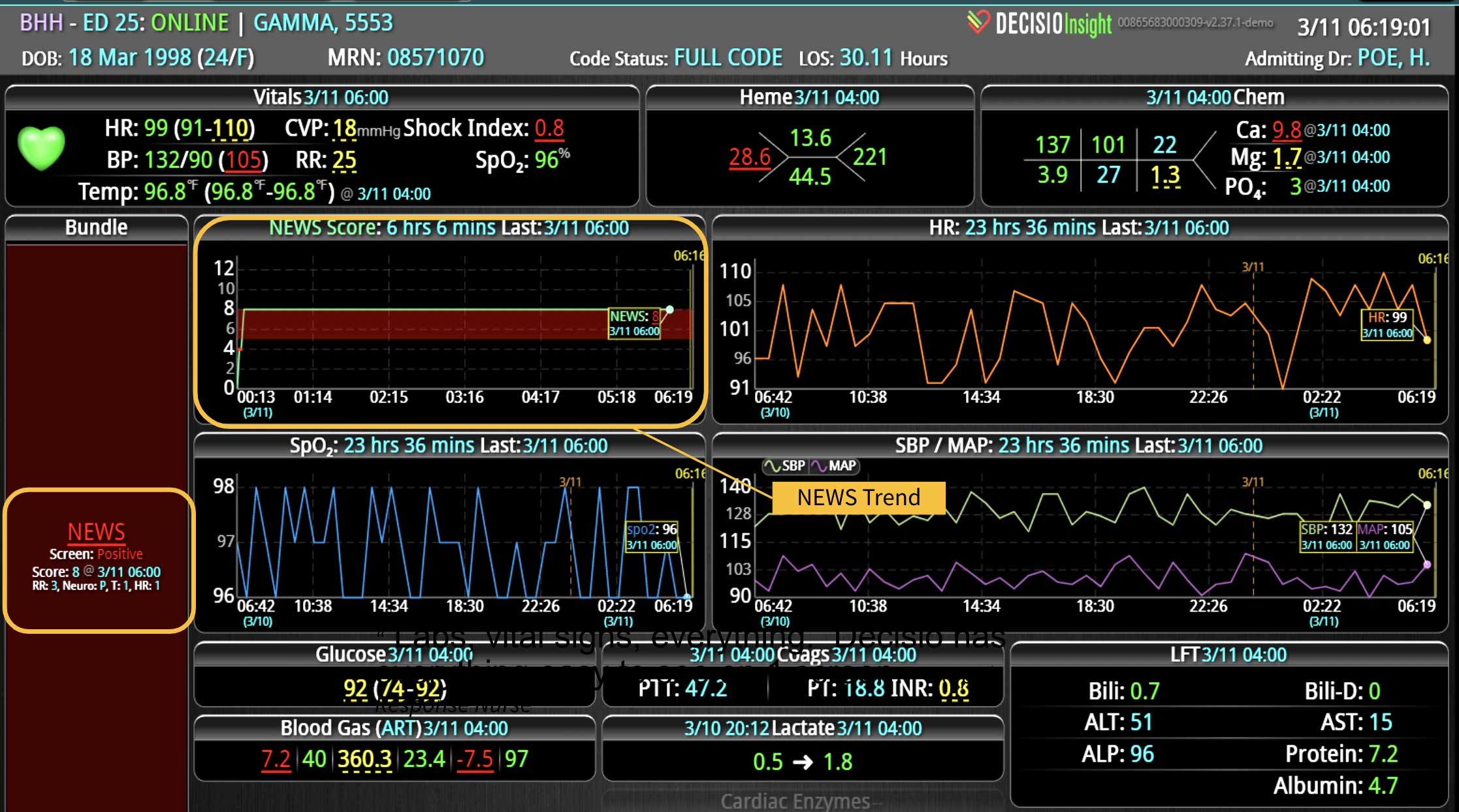
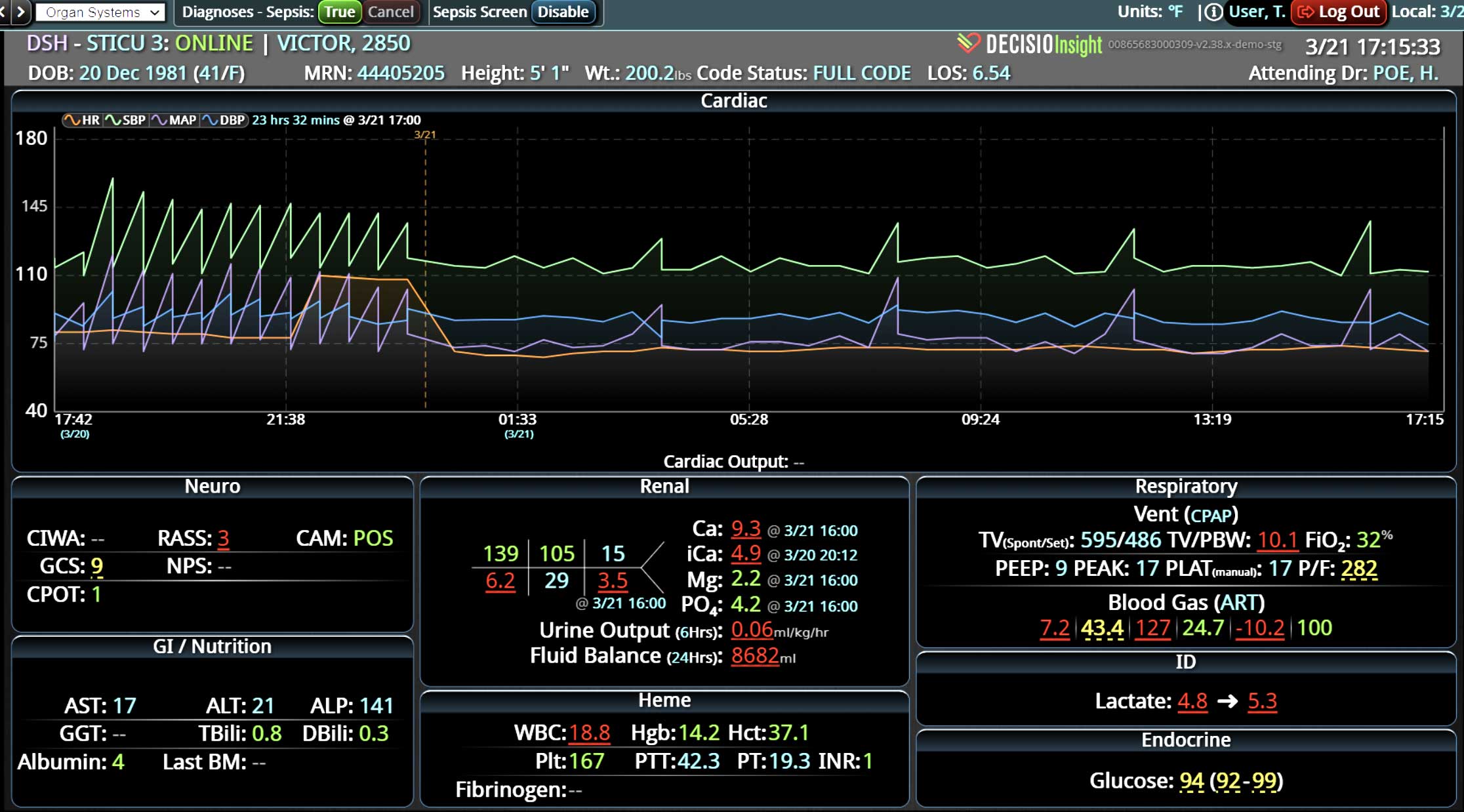
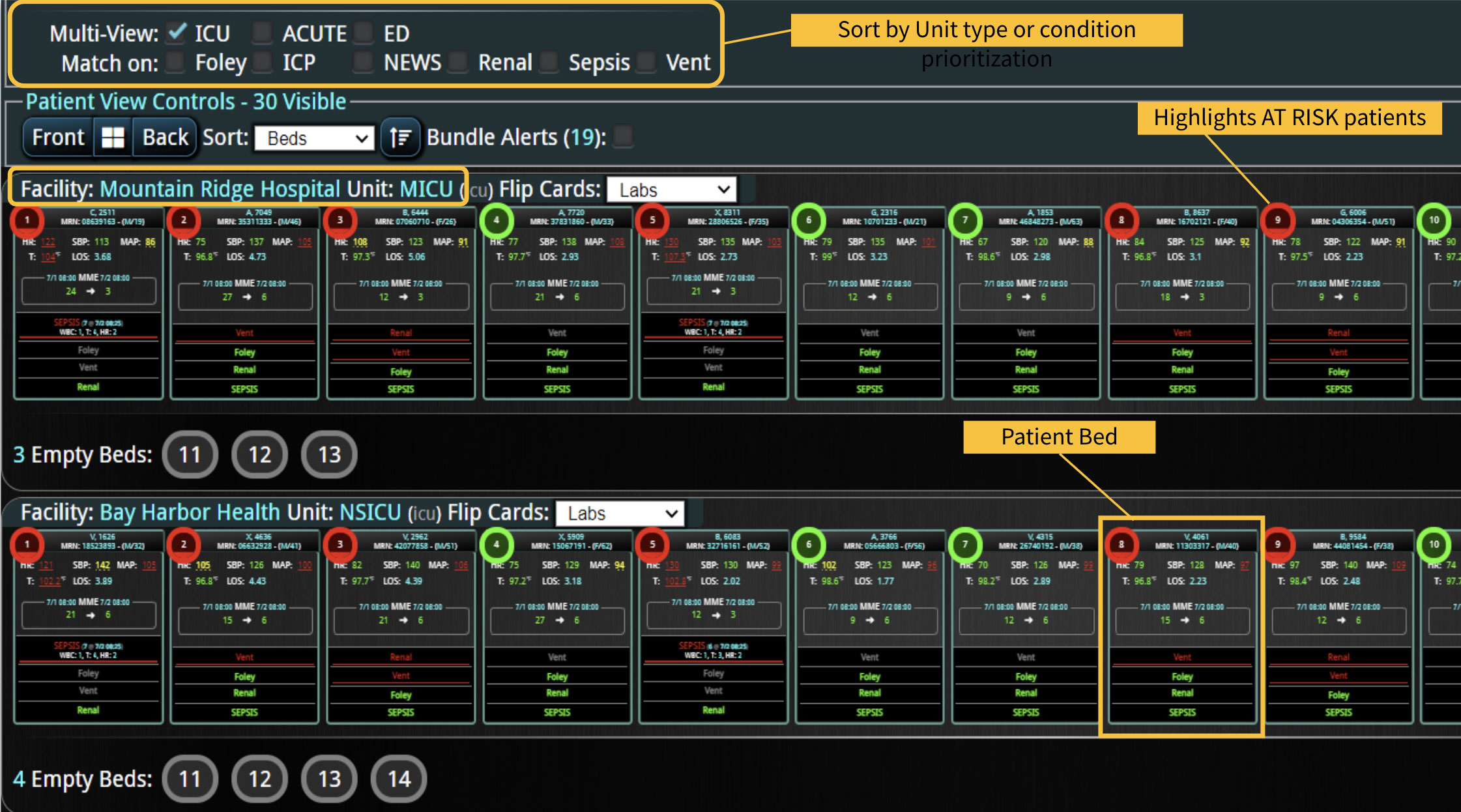
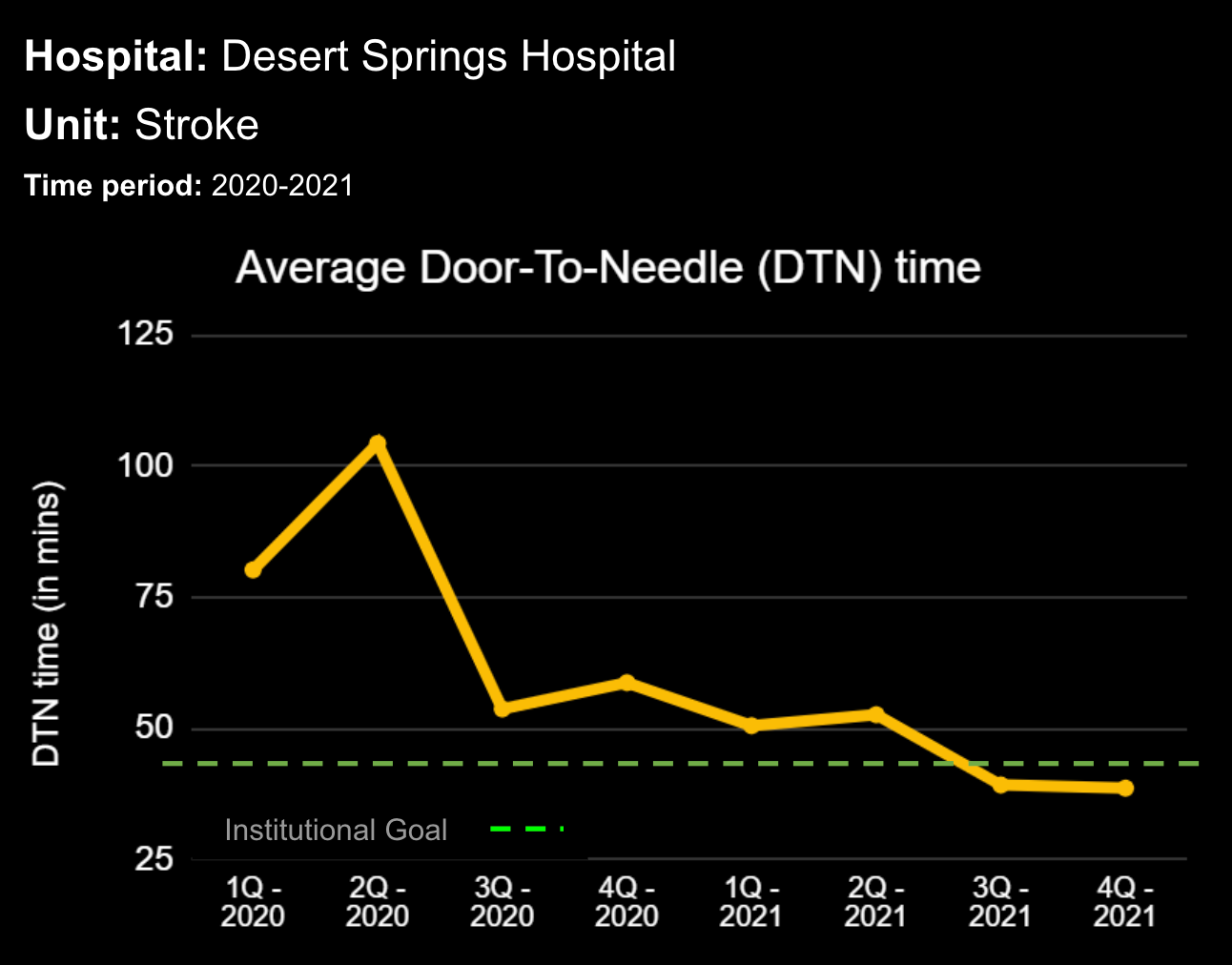
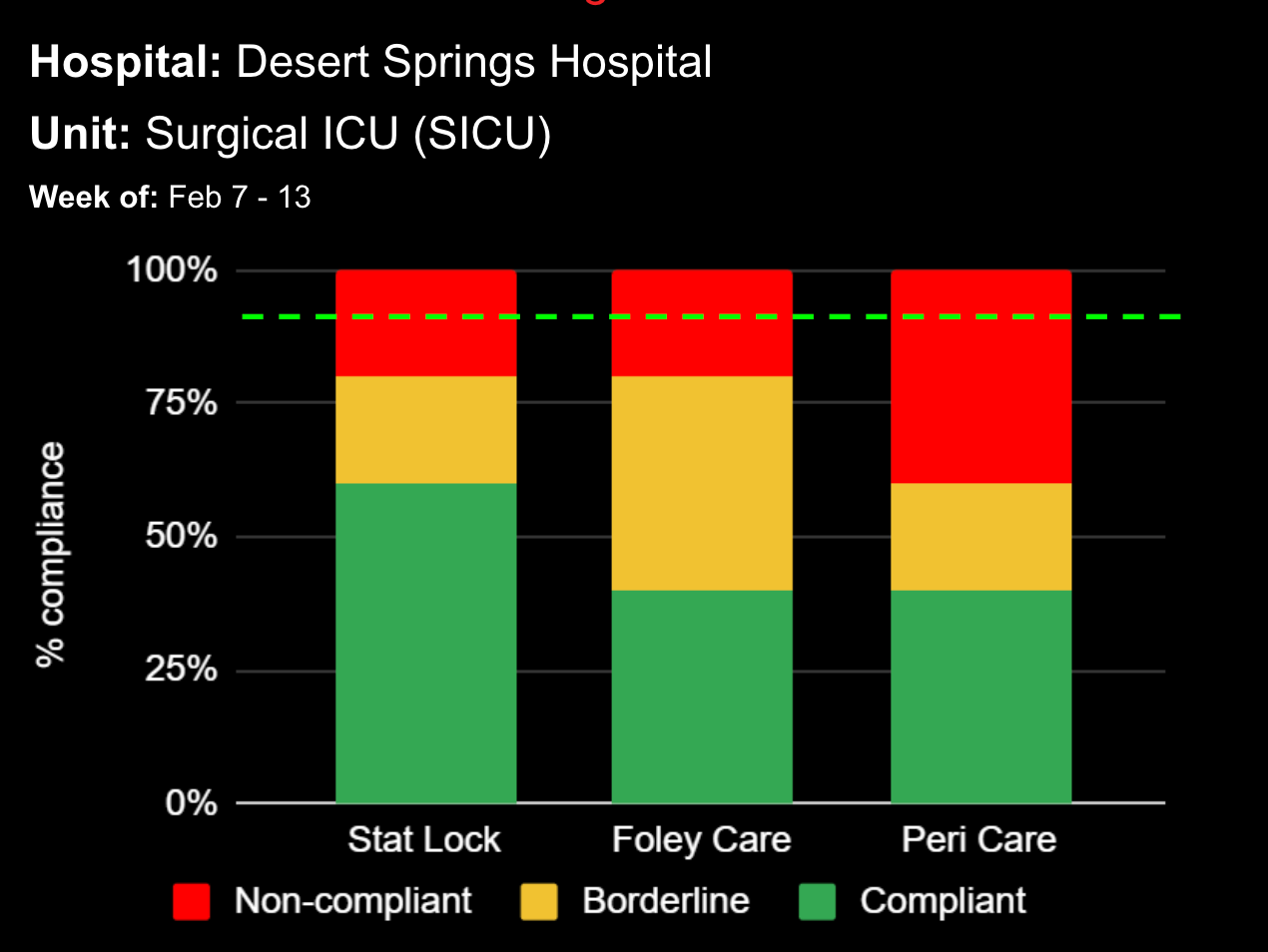
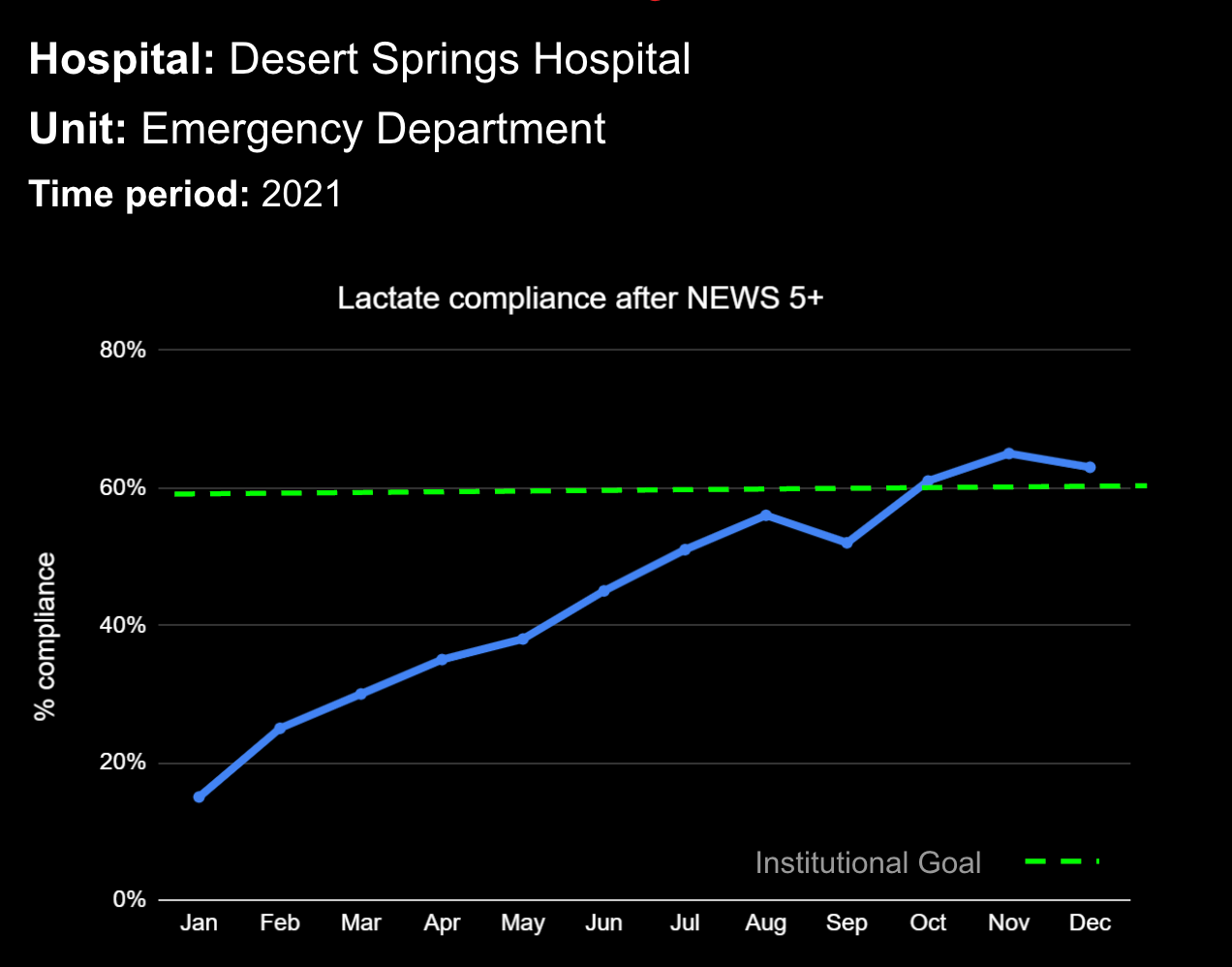
A commercially available web-based clinical surveillance and decision support dashboard system was implemented in our neuroscience and surgical intensive care units (ICU) in December 2016. The system continuously displays the most recent vital signs and laboratory data on a dedicated clinical dashboard visible to all members of the care team at the bedside. Medication administration data were available for the decision support system after April 2017. An automated sepsis screen based on heart rate, body temperature, respiratory rate, and white blood cell count was also initiated in April 2017 and became visible to clinicians on the dashboard starting in June 2017. We measured sepsis incidence and mortality among septic patients before (group 1, April – June 2017) and after (group 2, June – October 2017) implementing the sepsis screen. Patients were retrospectively diagnosed as septic utilizing clinical, laboratory and medication administration data available in the EHR utilizing a validated method, (JAMA, 2017;318(13):1241-1249).
Results
There were 657 patients in group 1 and 1171 in group 2. Age (56 years) and gender (58% male) were the same for both groups. Both groups had a median of 2 positive sepsis screens during their ICU stay. Group 1 patients had a 6.5% rate of sepsis while in group 2 sepsis was 4.8% (p = 0.11). The mortality among septic patients in group 1 was 27.9% while in group 2 it was 16.1% (p = 0.05).
Conclusions
Implementing automated bedside clinical surveillance and visual decision support system was associated with trend towards a decreased rate of sepsis. Integration of a continuously available decision support system in the ICU setting may help all providers identify sepsis in real time and rapidly initiate treatment to improve quality of care.
Abstract Title:
Clinical Outcomes in Septic Patients after Implementing a Visual Clinical Decision Support System
Authors:
J Baker MD, B Jang BS, C Droege PharmD, E Quinones MD, H Radhakrishnan MD, T Pritts MD PhD, JB Holcomb MD, M Goodman MD, V Nomellini MD PhD
Presented By:
PRESENTED BY UNIVERSITY OF CINCINNATI AT THE 70TH SOUTHWESTERN SURGICAL CONGRESS ANNUAL MEETING