23 Oct Improving compliance with low tidal volume/lung protective ventilation with utilization of on-time, bedside surveillance and early warning decision support systemA2

Improving compliance with low tidal volume/lung protective ventilation with utilization of on-time, bedside surveillance and early warning decision support systemA2
Background
For mechanically ventilated (MV) patients with and without acute respiratory distress syndrome (ARDS), outcomes such as subsequent lung injury, length of stay, infections, and duration of MV are improved with timely utilization of low tidal volume (LTV)/lung protective ventilation. Despite this widely acknowledged benefit, adherence rates to LTV remain low, ranging from 7-41%. The purpose of this investigation was to determine if a decision support software system providing real-time, bedside alerts can improve adherence to LTV for patients on MV.
Methods
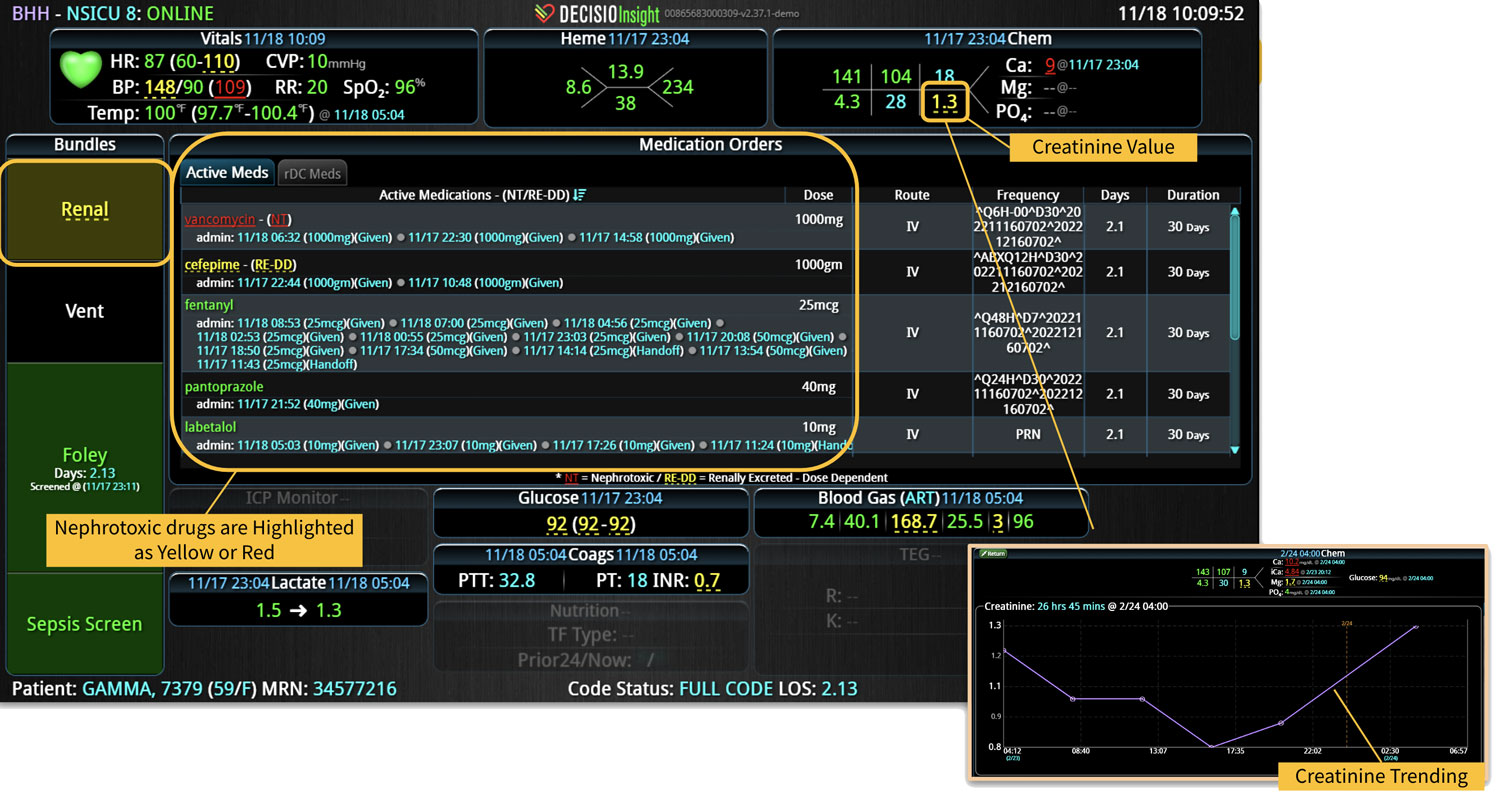
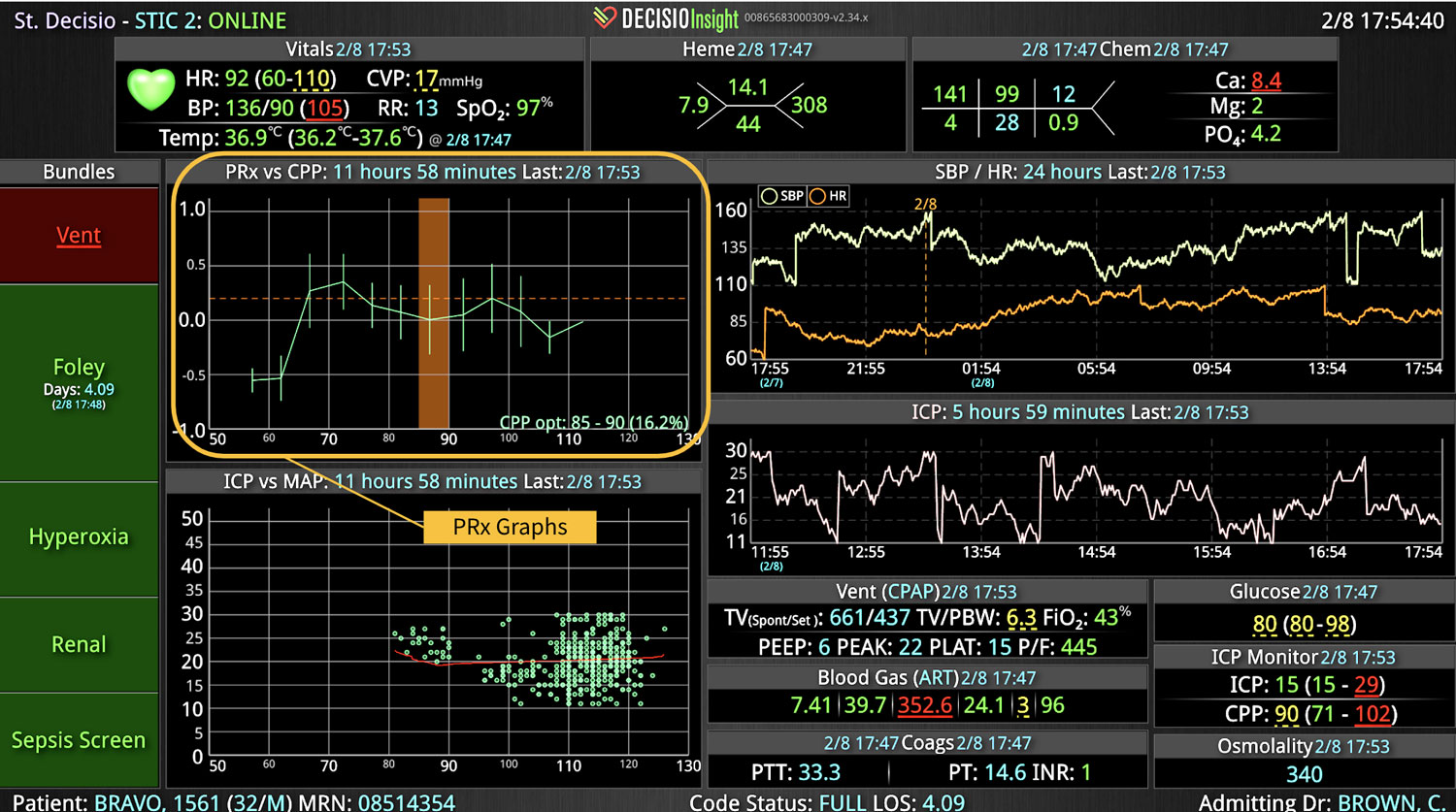
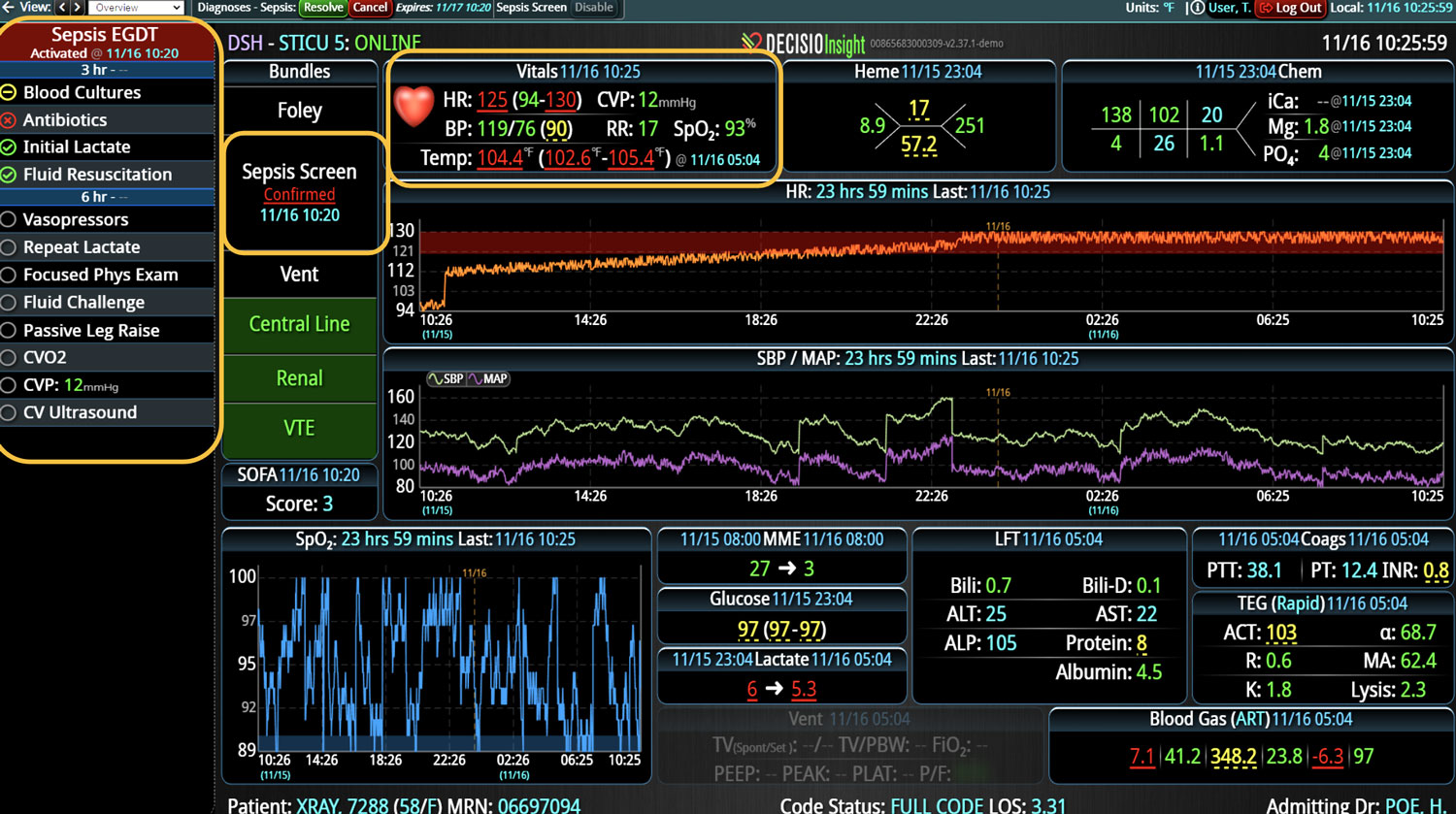
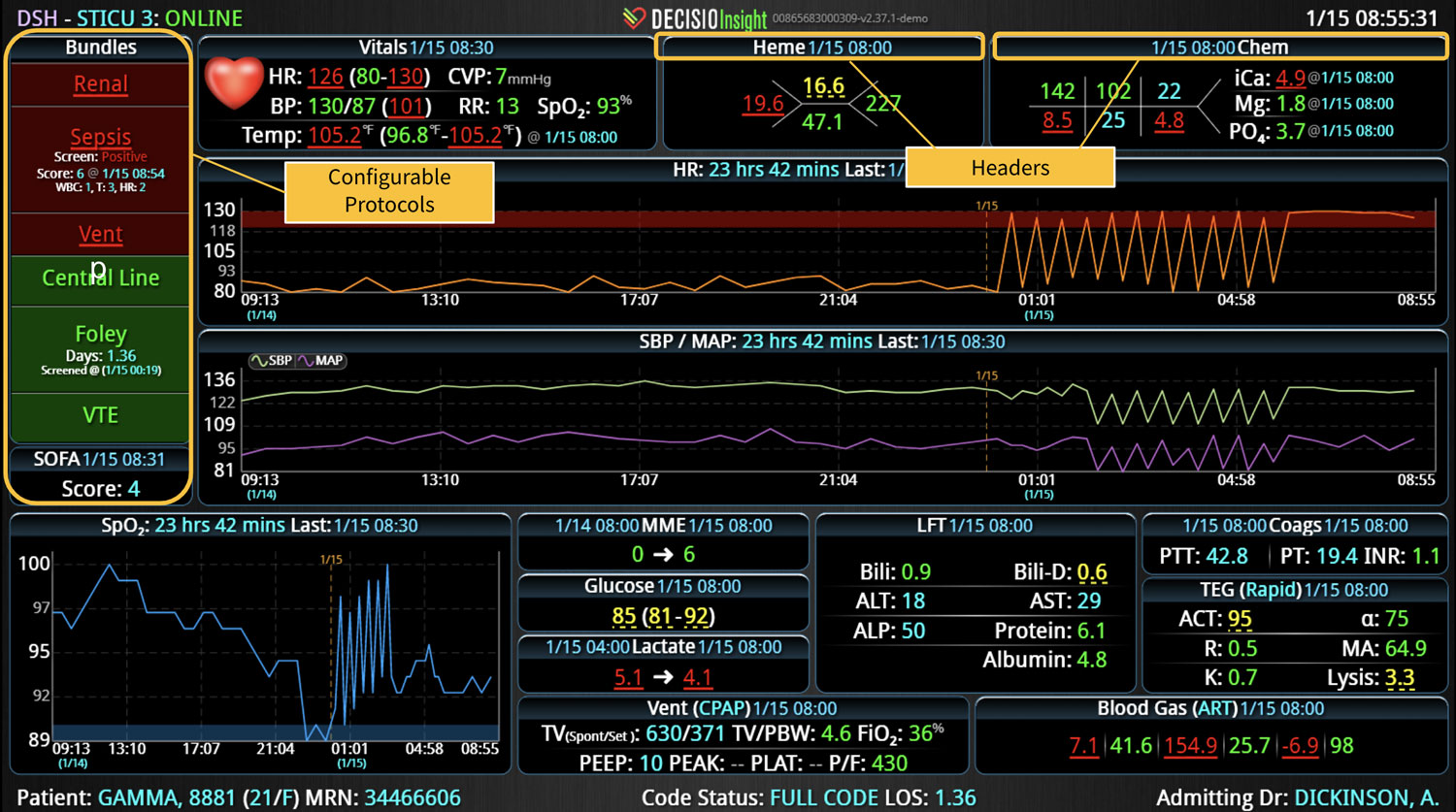
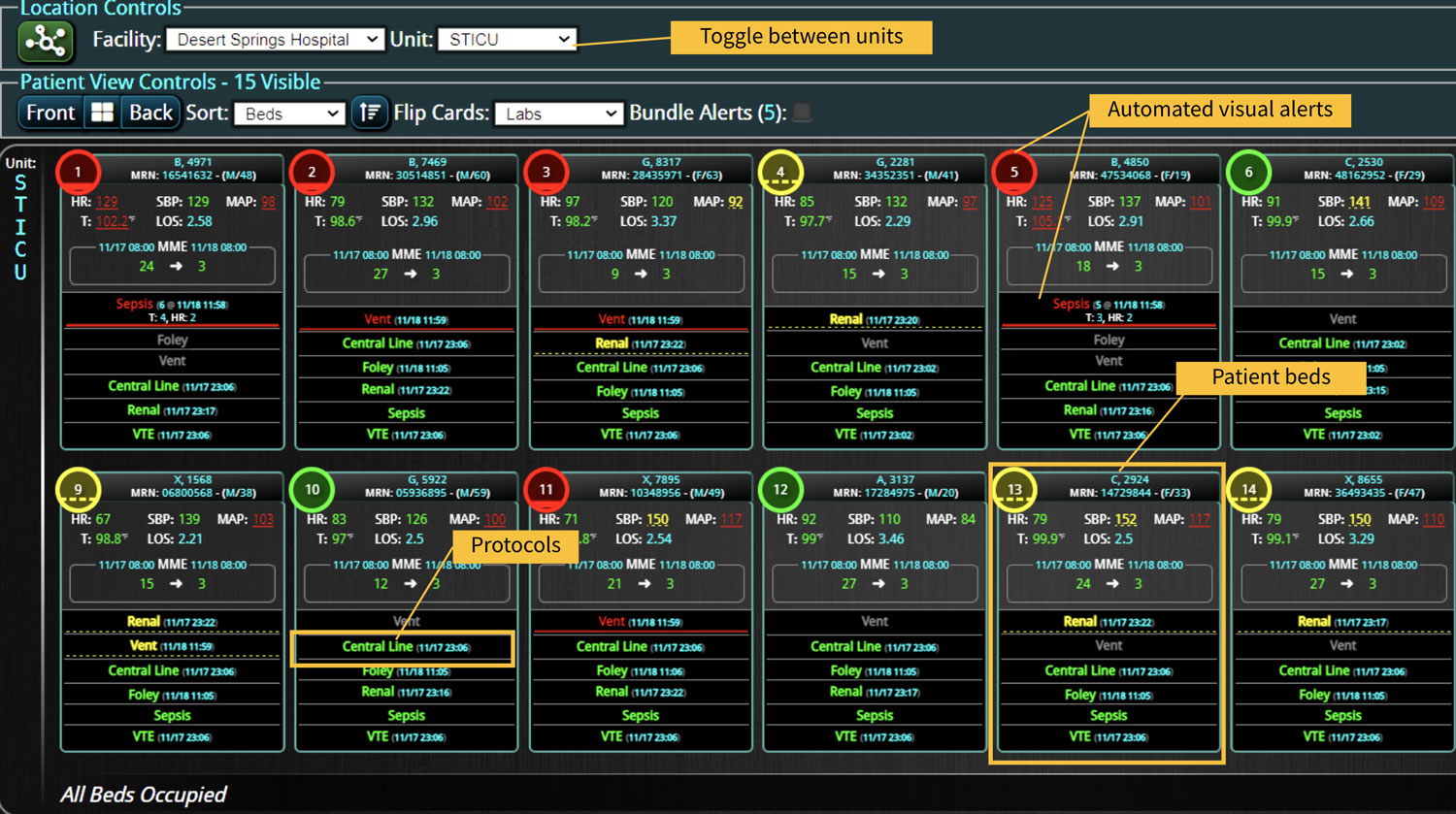
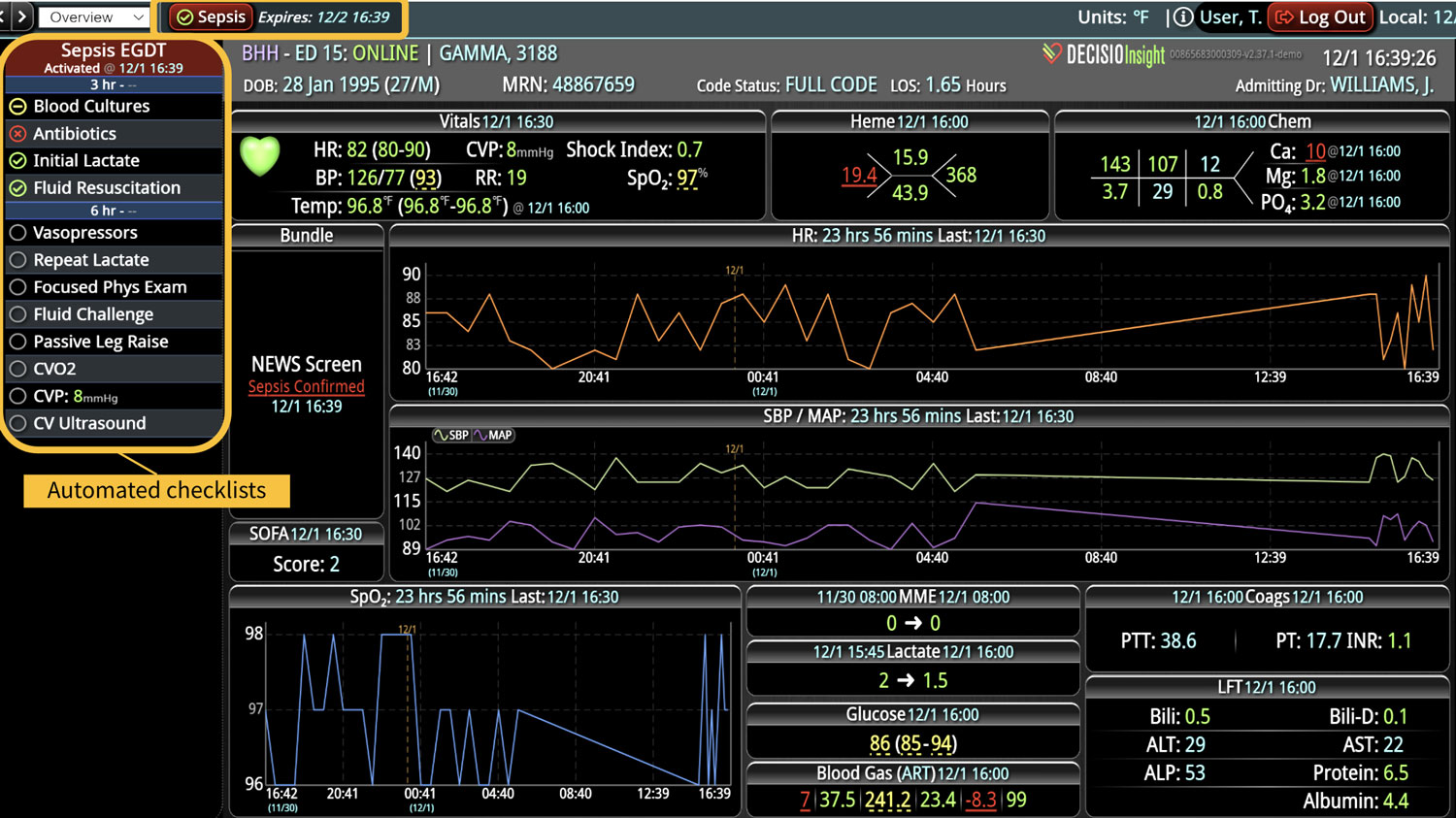
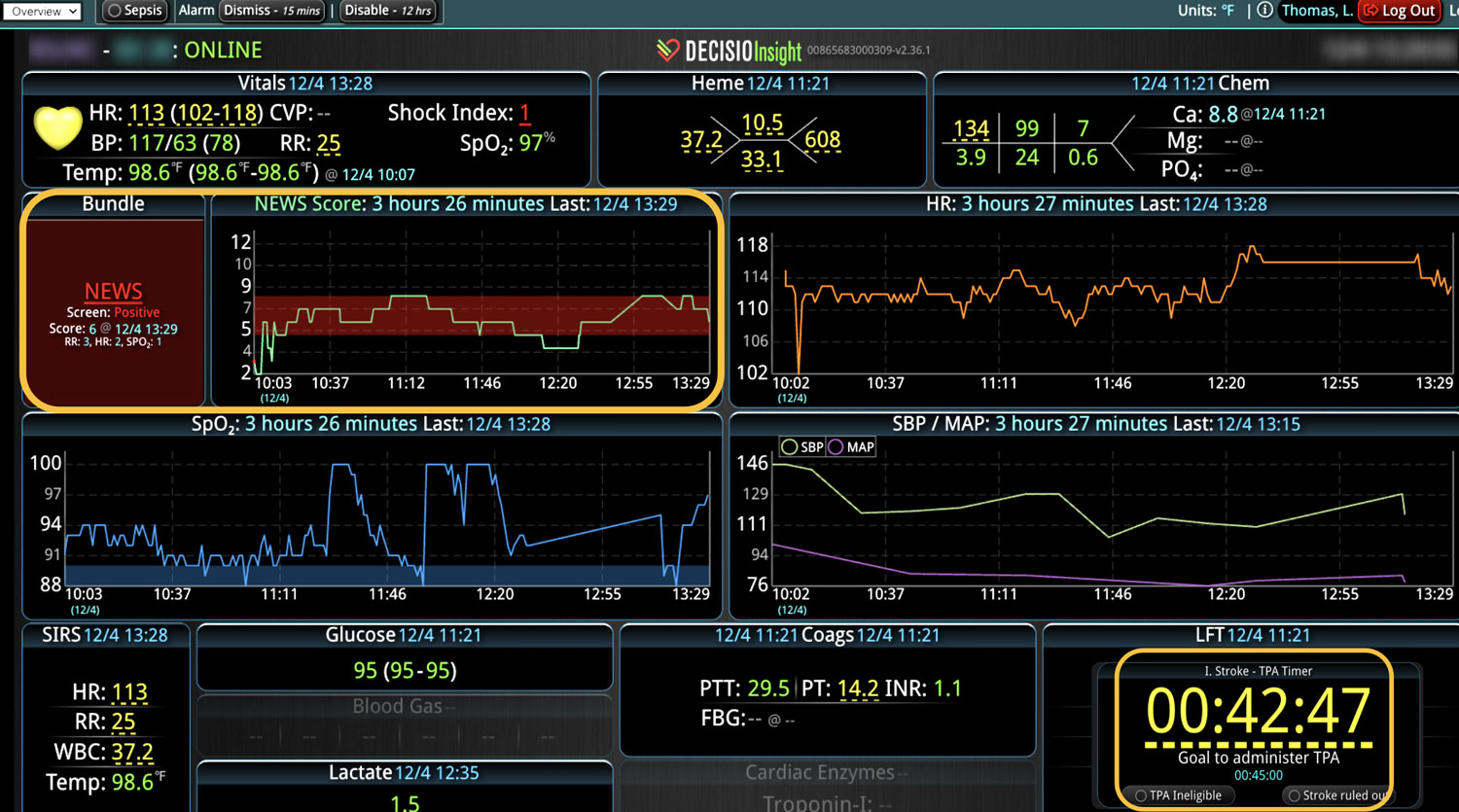
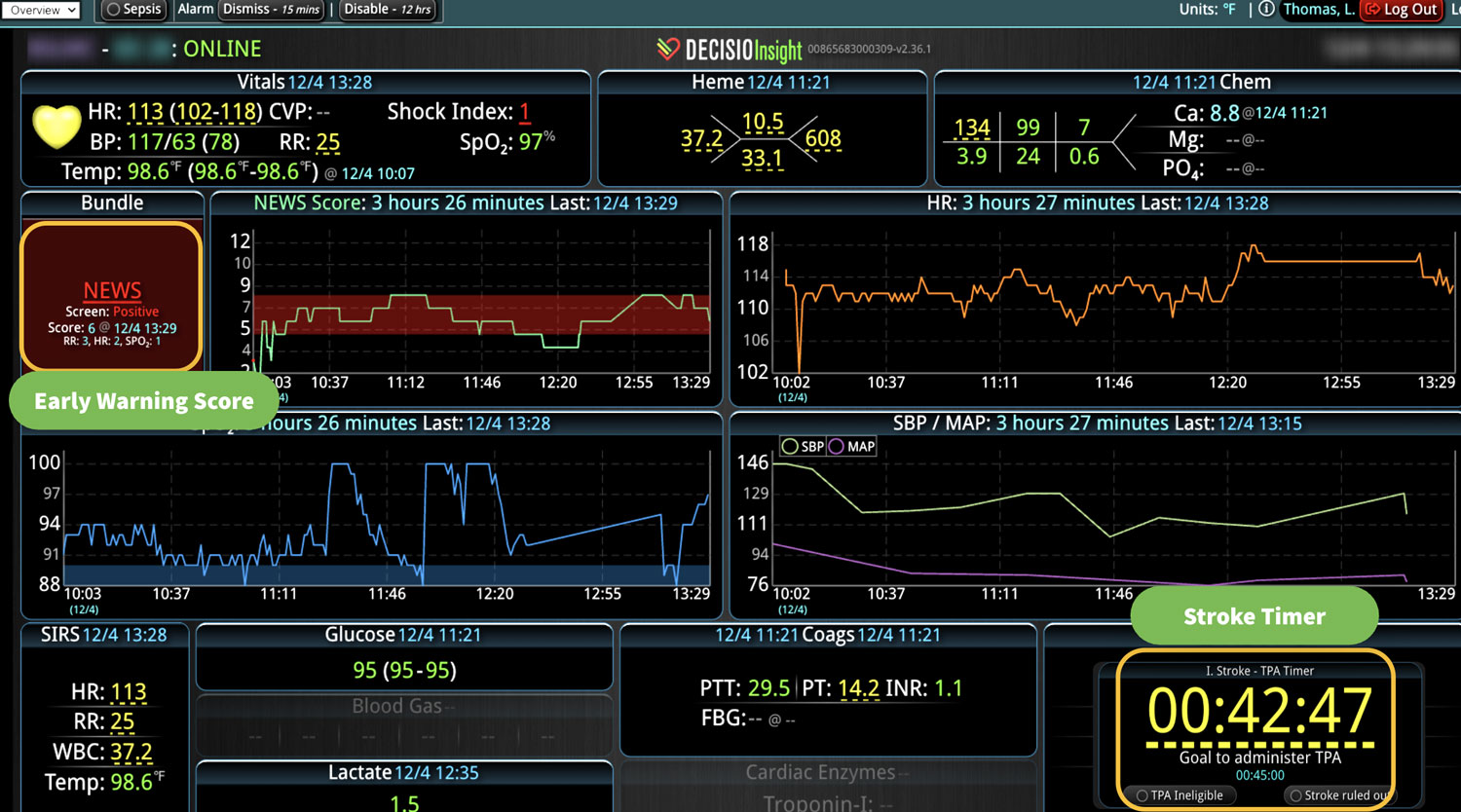
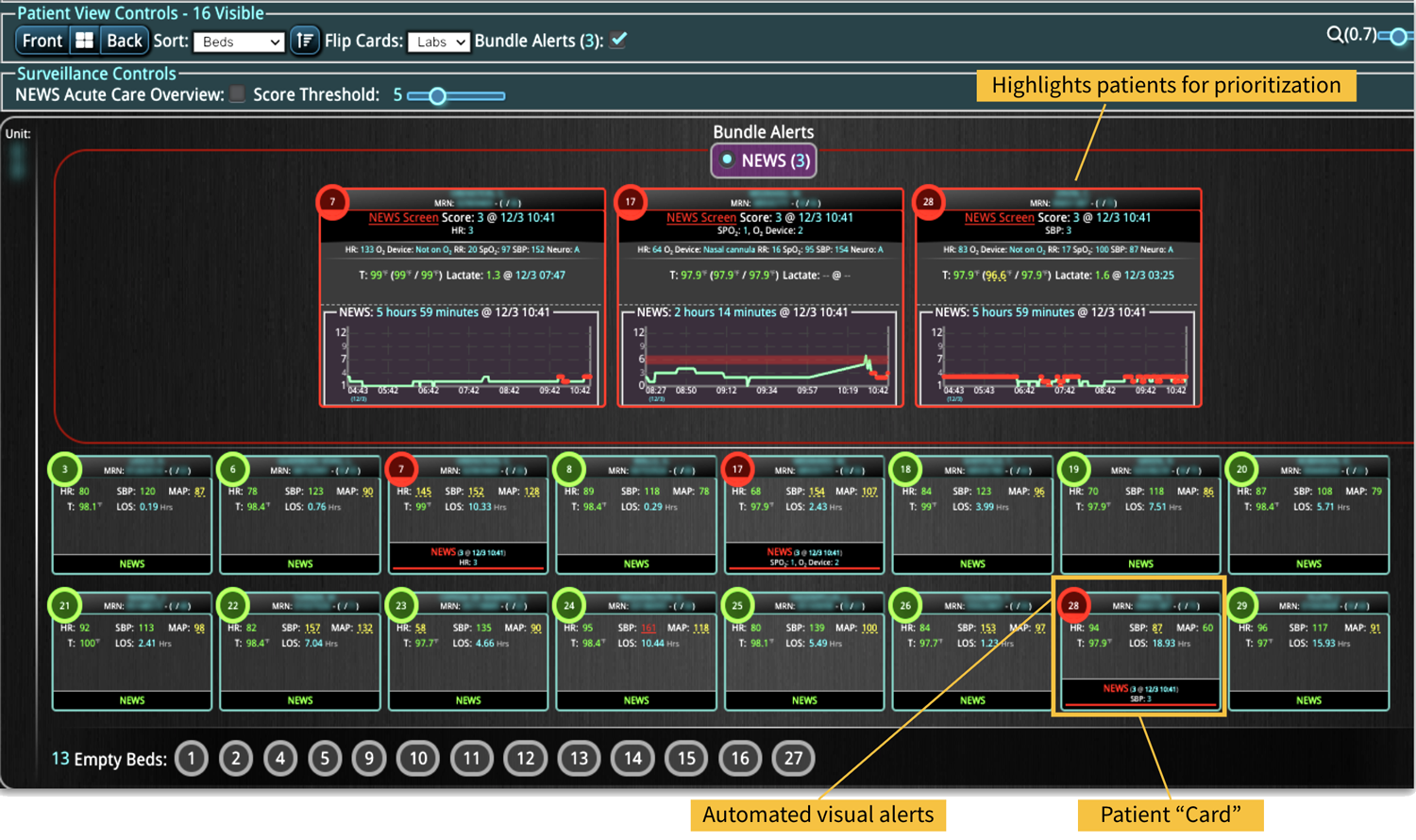
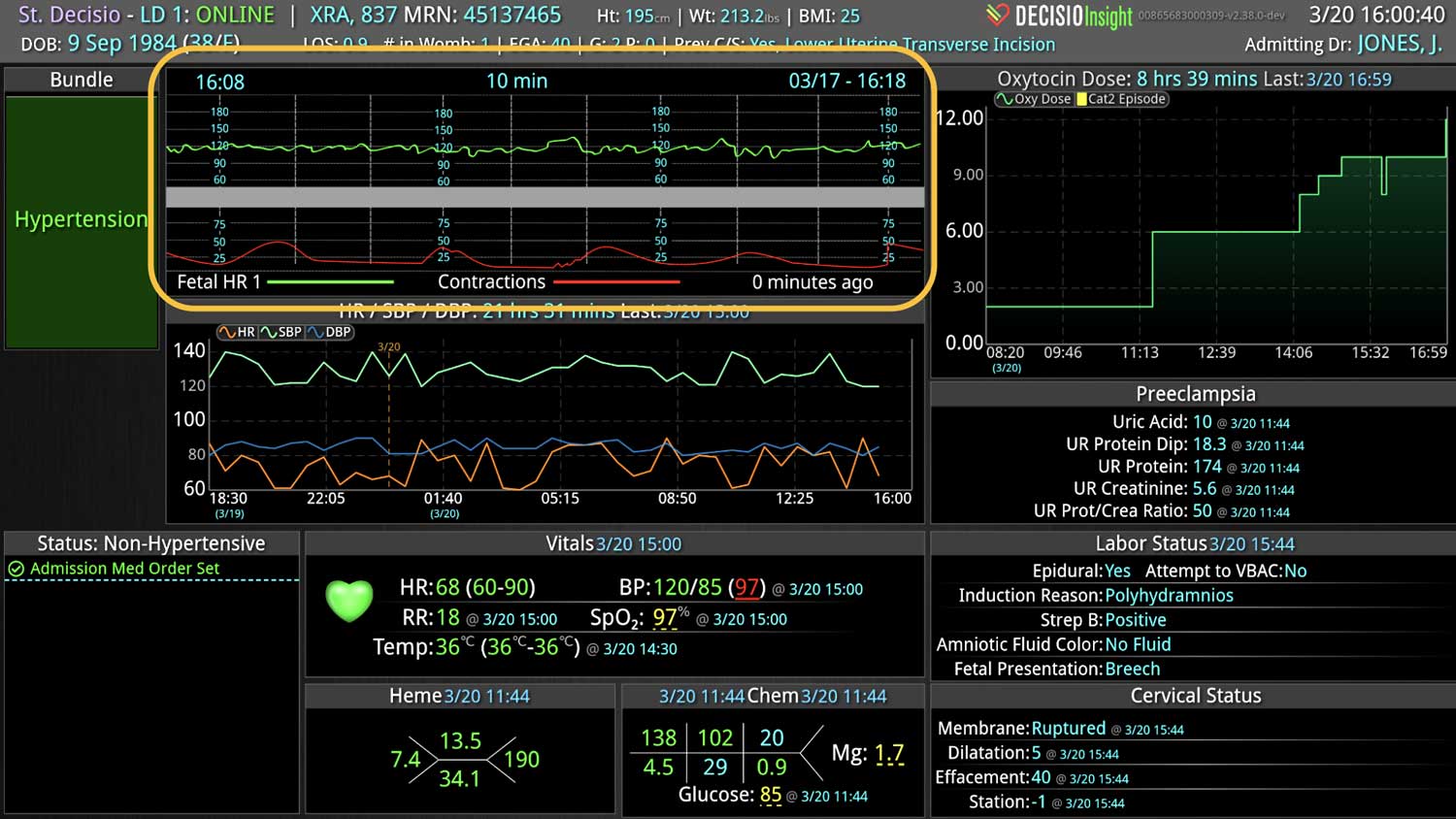
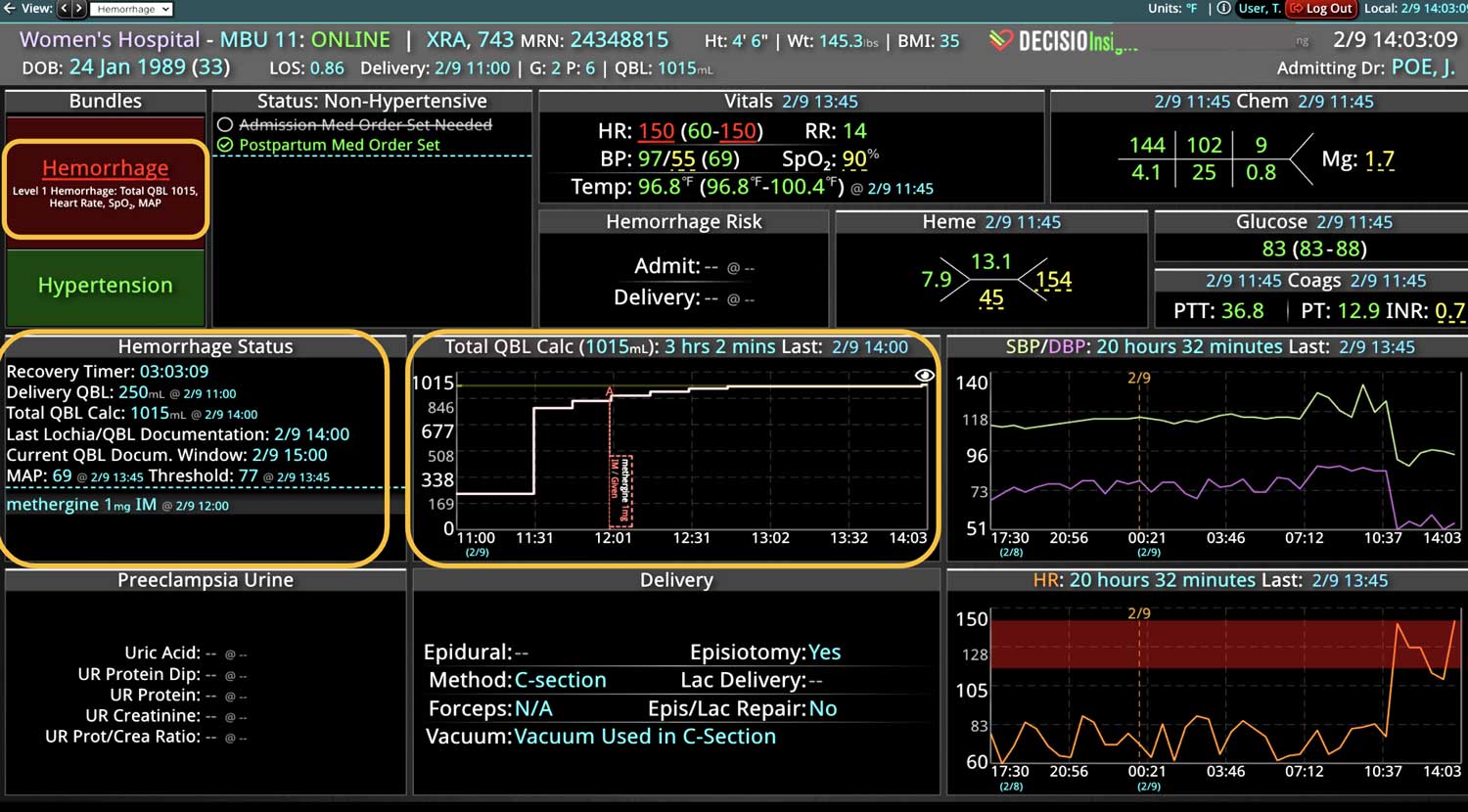
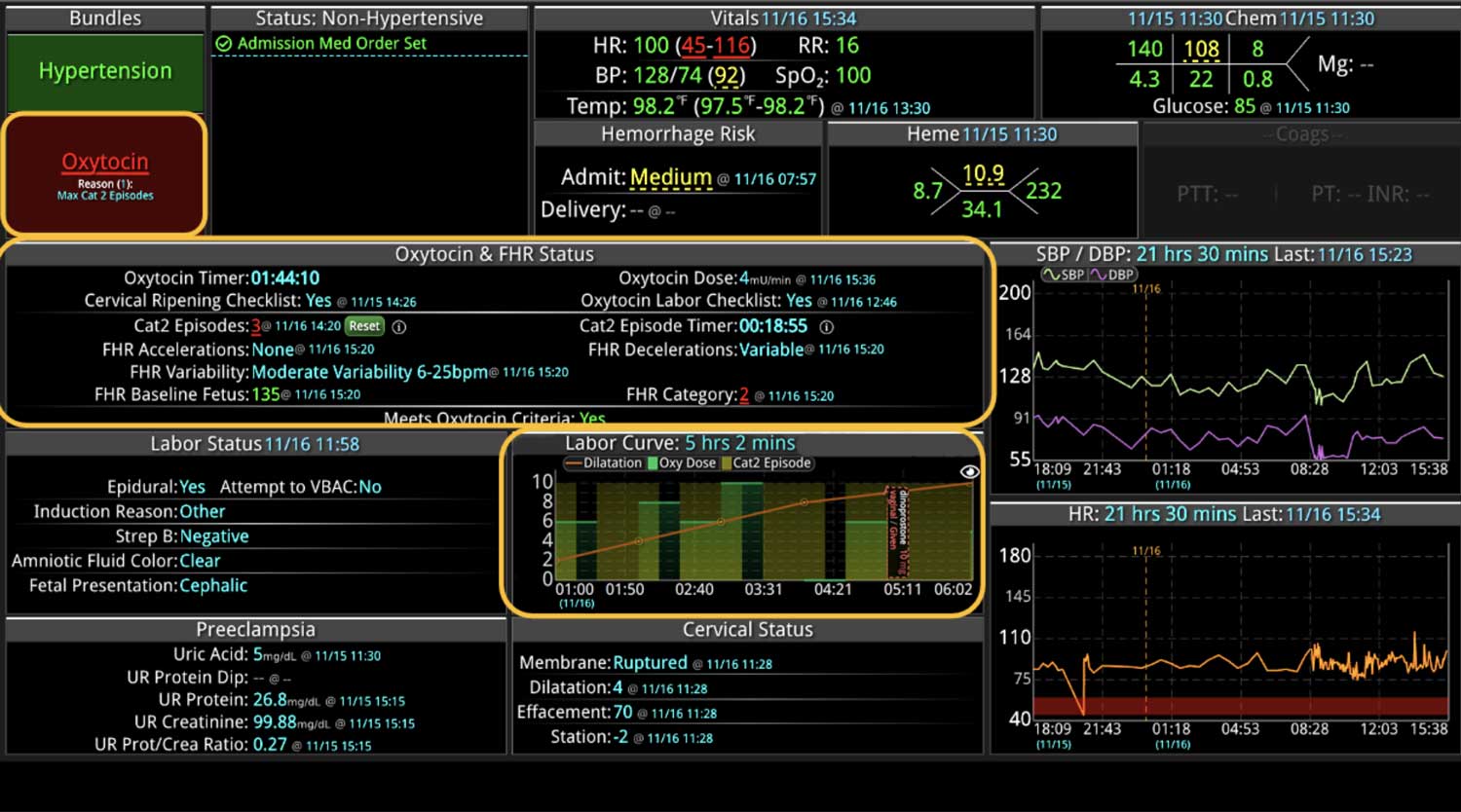
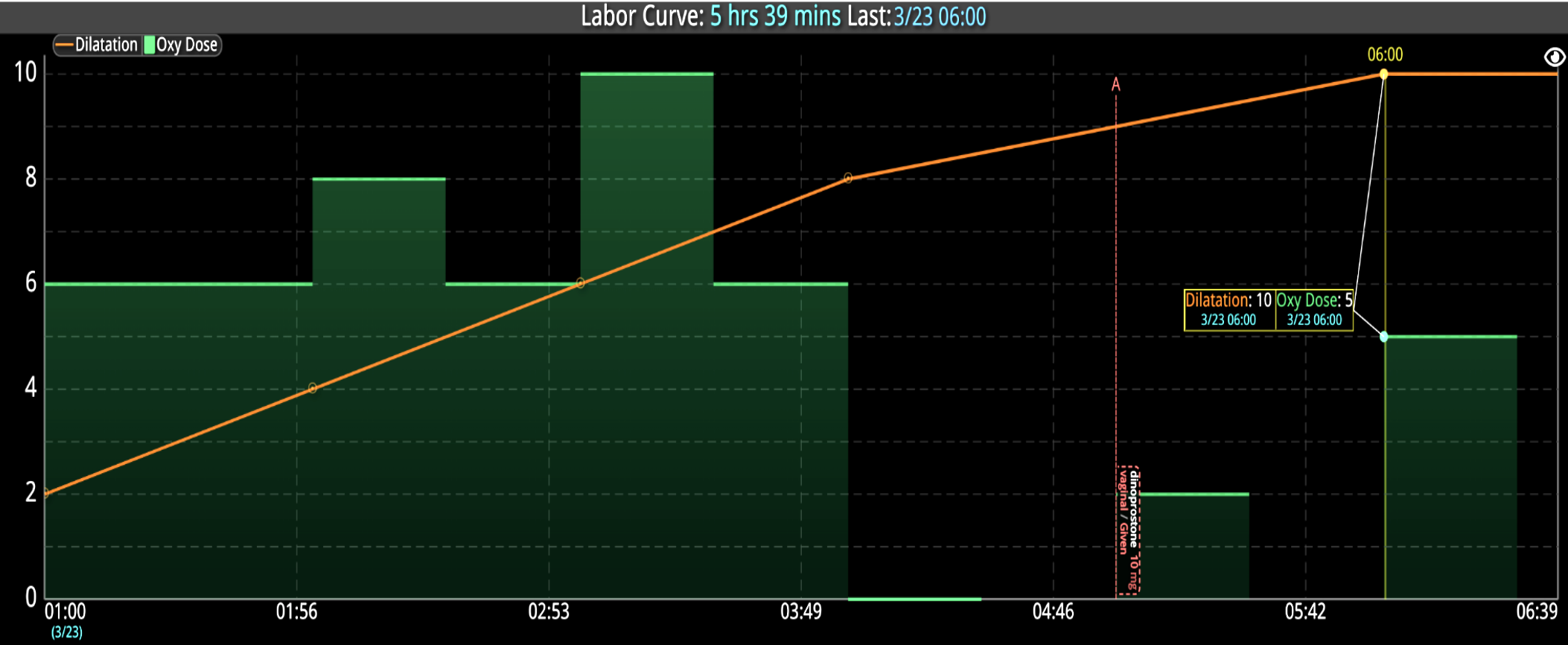
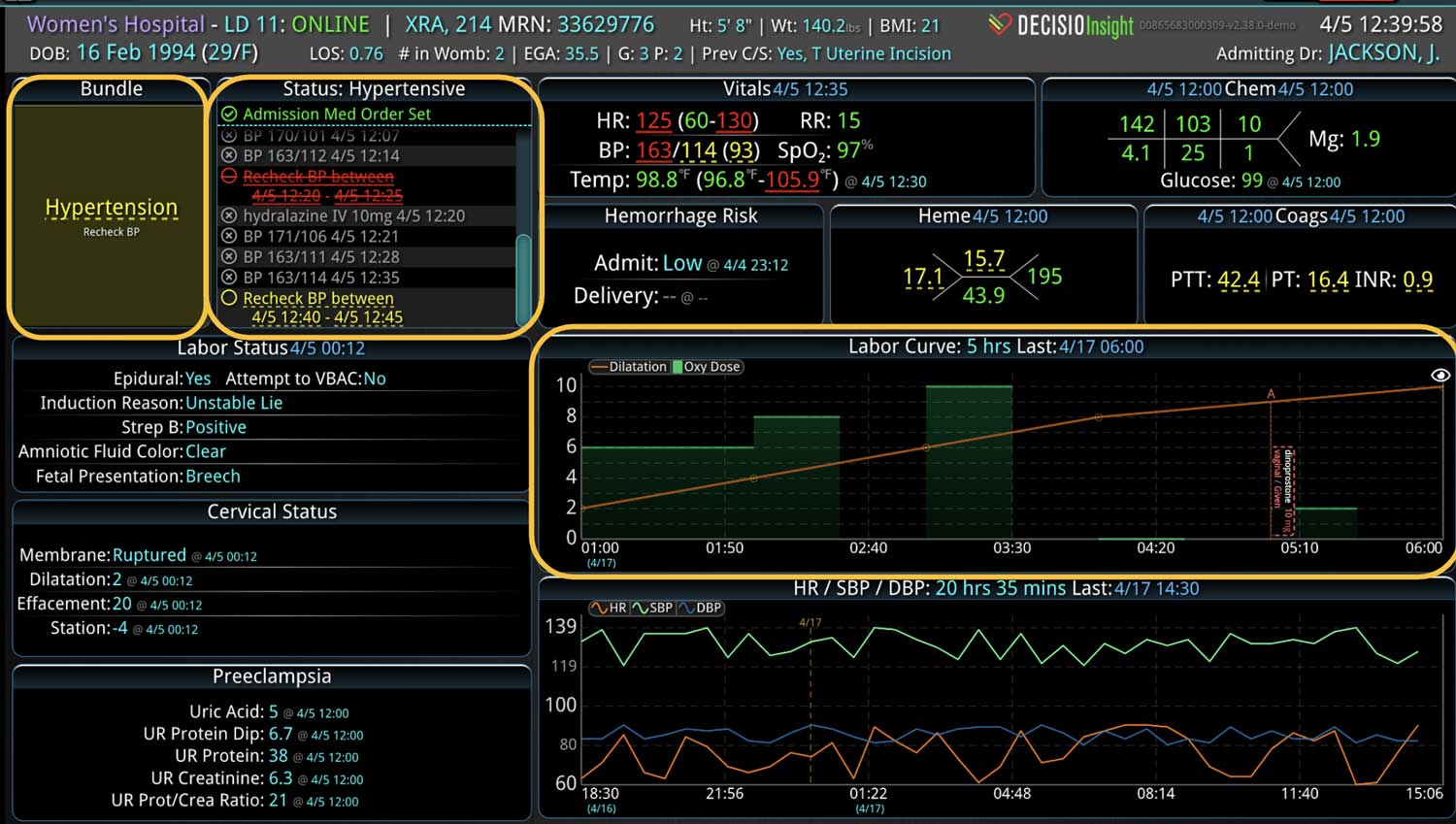
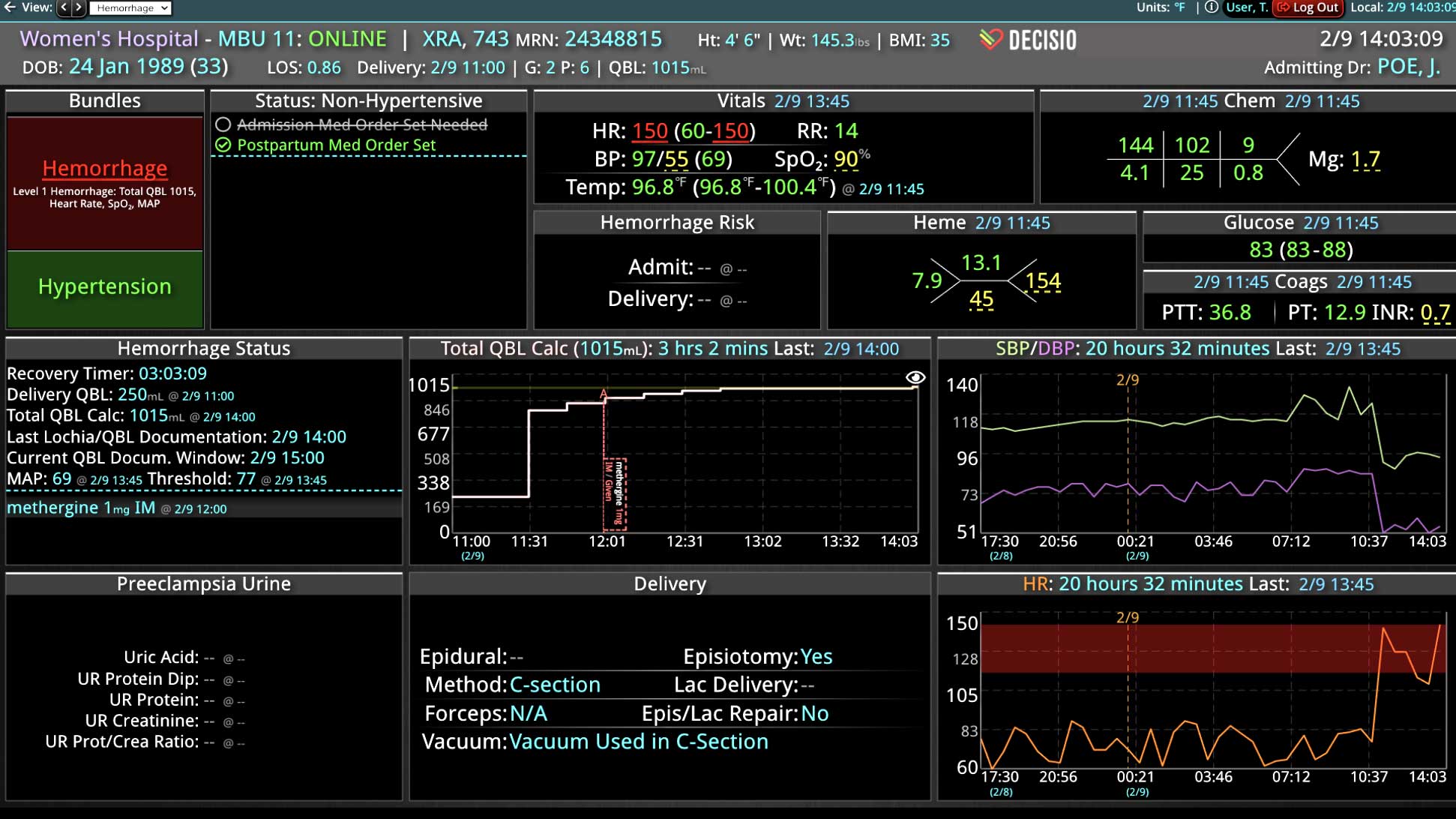
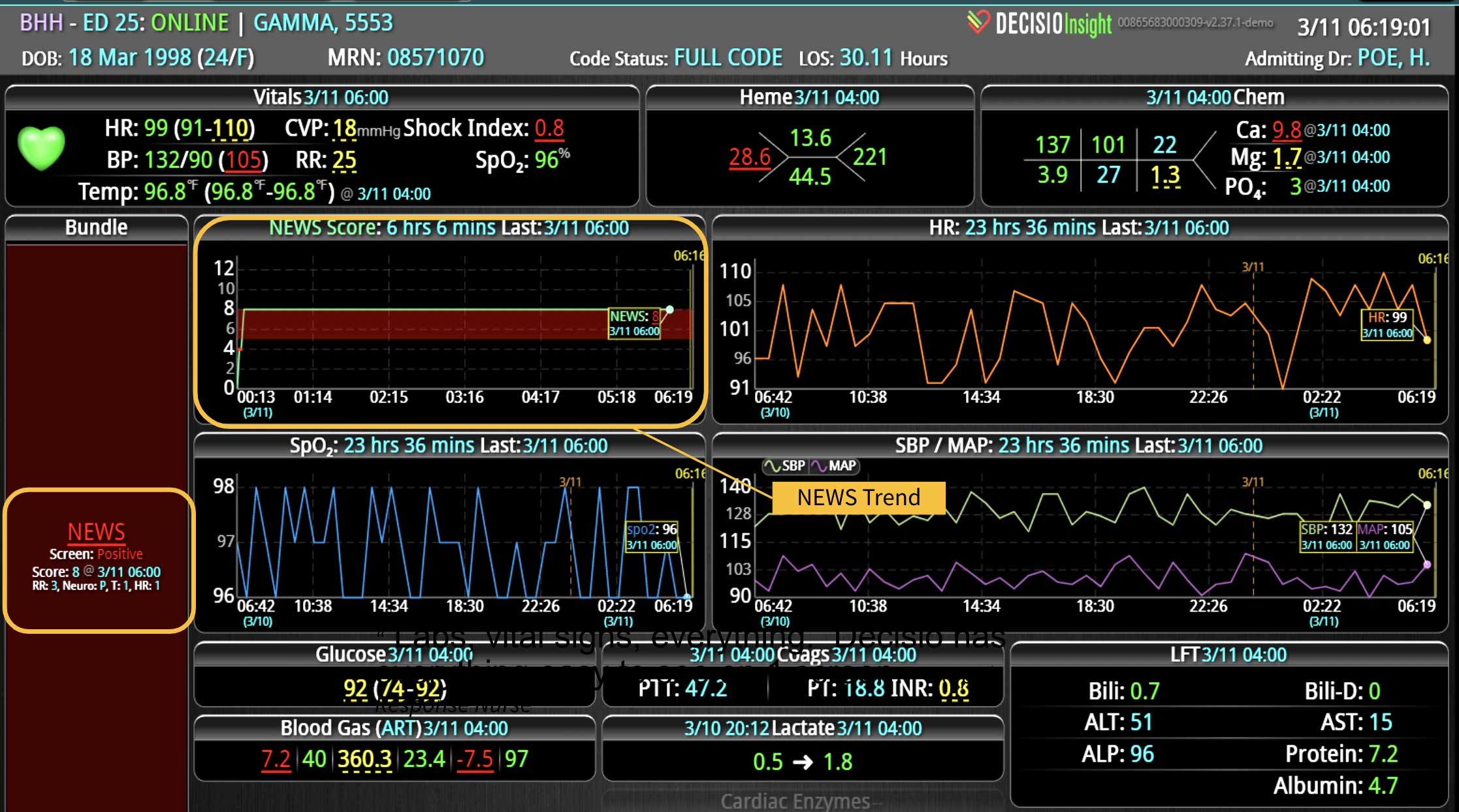
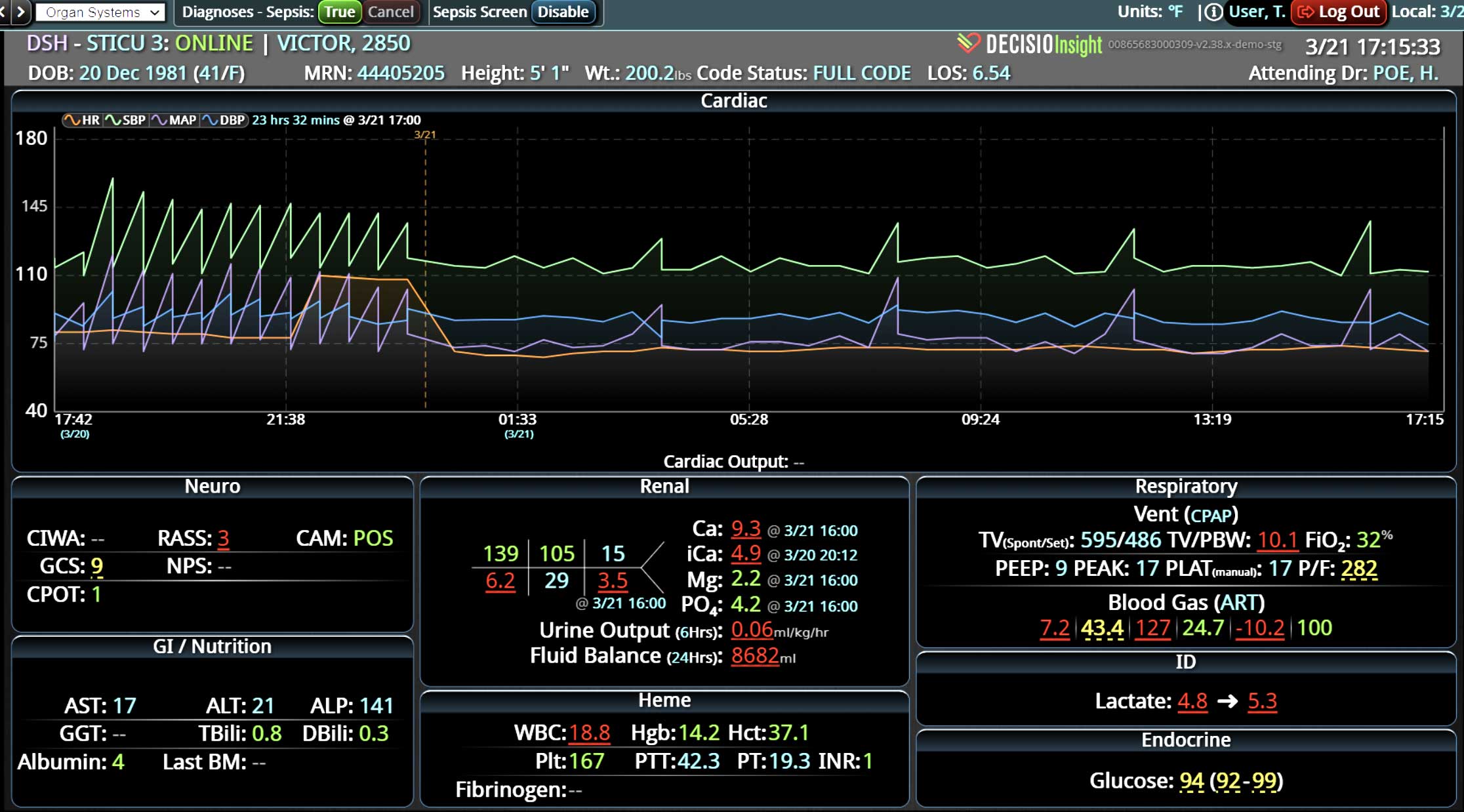
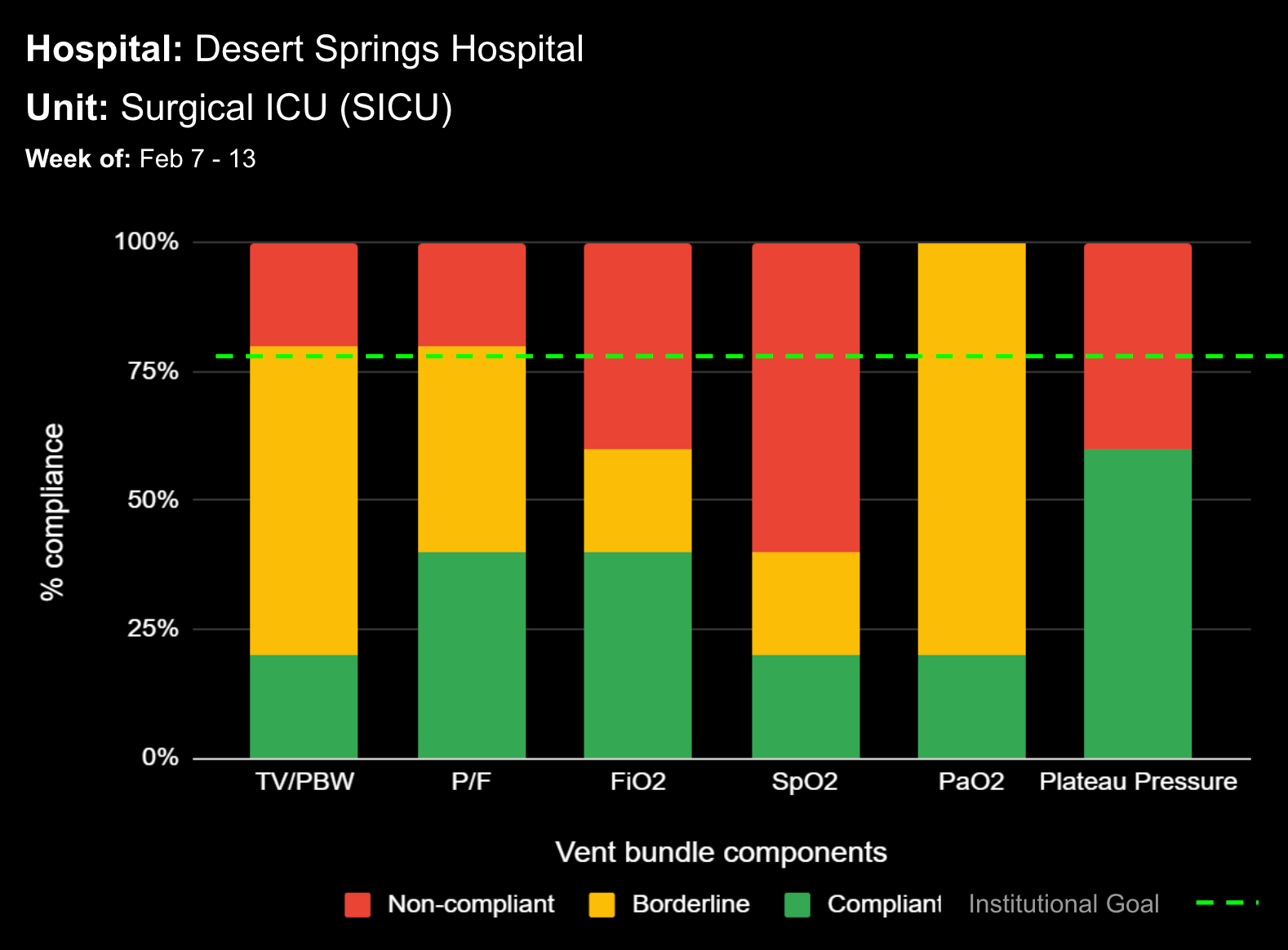
Two medical intensive care units (ICU) were equipped with a decision support software system that displayed real-time surveillance data and warnings on a large video screen above each patient’s bed. For all patients on MV, the screen displayed real-time tidal volume per probable body weight (TV PBW) – this value was displayed in green, yellow, or red for values <6, 6.1-8, and >8 ml/kg PBW, respectively. The PaO2/Fio2 (P/F) was also displayed in red, yellow, and green for values <150, 151-300, and >300, respectively. Also, a dedicated “ventilator bundle” window flashed yellow or red if either the TV PBW or the P/F value were within their warning ranges. With each arterial blood gas result, a TV PBW value was categorized as <6, 6-1-8, or >8 ml/kg, and a P/F value was categorized as >300, 201-300, 101-200, or <100. Control group and intervention group data were obtained from the same ICU’s during four months prior to and two months after the intervention – providing a “before and after” comparison from the same unit. The primary outcome was to compare pre- and post-intervention percent adherence to LTV, defined as <6 ml/kg PBW.
Results
For patients with suspected severe ARDS (P/F <100), the percent adherence to LTV was 40.3% in the pre-intervention group, and 65.6% in the post-intervention group (p=0.021). For patients without suspected ARDS (P/F >300), the percent of patients ventilated at >8 ml/kg PBW was 14.5% in the pre-intervention group, and 7.8% in the post-intervention group (p=0.032). For all patients on MV, the percent of patients ventilated at >8 ml/kg PBW was 13.5% in the pre-intervention group, and 7.8% in the post-intervention group (p=0.004).
Conclusions
This report demonstrates that a bedside decision support system significantly improves early recognition of suspected ARDS and adherence to LTV for mechanically ventilated patients.
Clinical Implications
It has been estimated that for intensivists to adhere to evidence-based practices for a complex critically ill patient, it would require up to 200 interventions daily, clearly stretching human capabilities. This study indicates that a decision support software system, with real-time surveillance and early warning alerts, can provide a critical “backstop” for clinicians and hospitals attempting to adhere to best practices, improve outcomes, and reduce medical errors.
Abstract Title:
Improving compliance with low tidal volume/lung protective ventilation with utilization of on-time, bedside surveillance and early warning decision support system
Authors:
Christopher Howard, MD, FCCP, Anand Naik, James Herlihy, Christopher Morgan, Babith Mankidy, Muhammed Siddique, Ali Omranian, Kalpalatha Guntupalli
Presented By:
BAYLOR ST. LUKE’S MEDICAL CENTER AT THE 47TH ANNUAL CRITICAL CARE CONGRESS (SCCM)