10 Jun The Impact of CLABSI on Hospitals and Strategies for Prevention

The Impact of CLABSI on Hospitals and Strategies for Prevention
Central Line-Associated Bloodstream Infections (CLABSIs) pose a significant financial burden on hospitals, leading to increased hospital stays, additional medical treatments, and higher use of healthcare resources. Each CLABSI case can cost hospitals between $22,000 to $100,000, depending on the severity and interventions required. Additionally, hospitals may face penalties from insurance companies and reduced reimbursements from Medicare and Medicaid due to high infection rates. These financial strains emphasize the importance of investing in preventive measures and staff training to reduce CLABSI incidence.
The Finanical Impact of CLABSI
A detailed study conducted at a tertiary-care academic medical center found that CLABSI significantly increased hospital costs and mortality risk. The study revealed that adjusted variable costs for CLABSI patients were approximately $32,000 higher than for those without CLABSI (in 2010 US dollars). Moreover, CLABSI was associated with a 2.27-fold increased risk of in-hospital mortality after adjusting for illness severity and other healthcare-associated infections. These findings highlight the substantial financial burden and elevated mortality risk linked to CLABSI in both ICU and non-ICU settings.
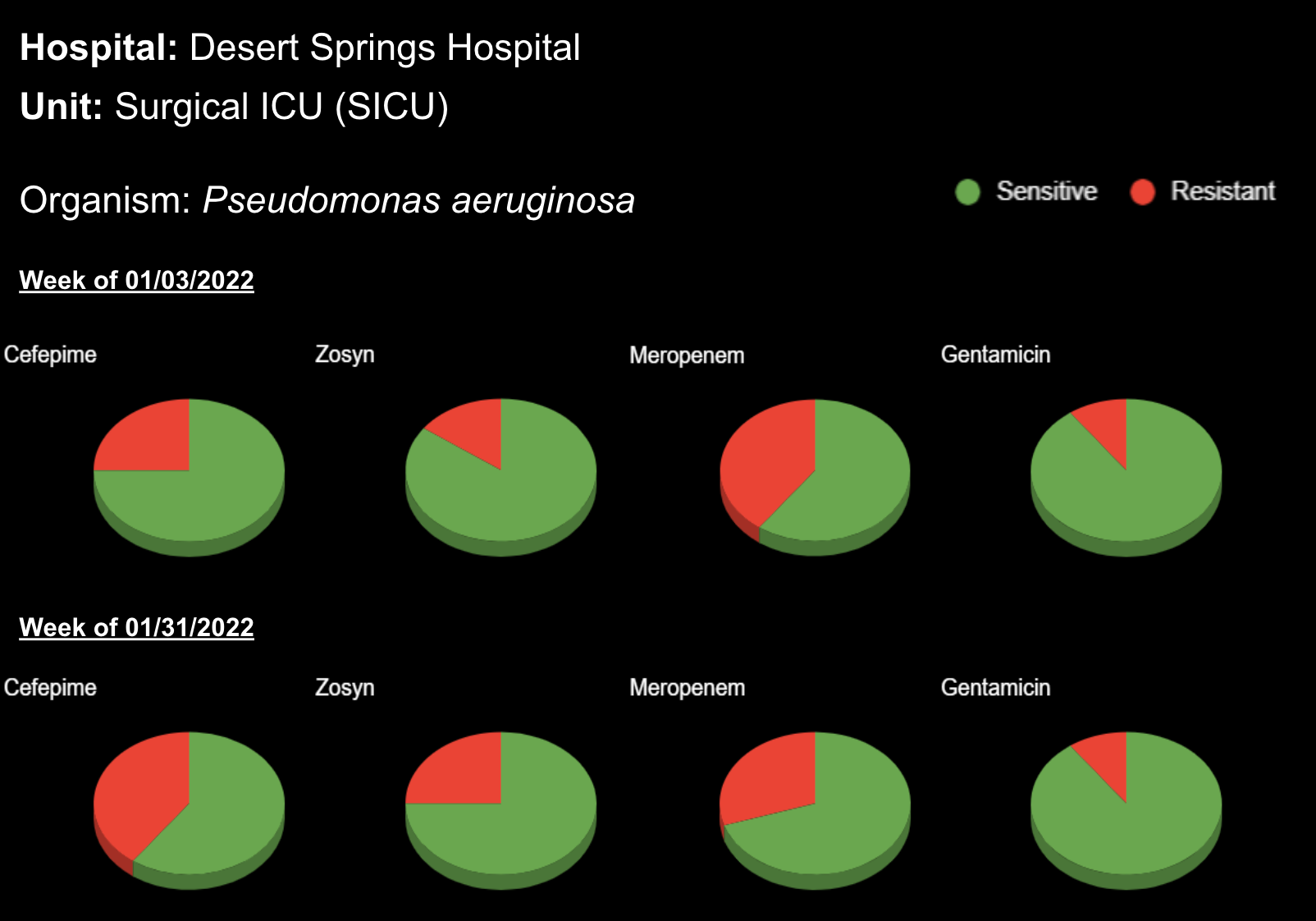
Antibiotic Resistance
The issue is further complicated by antibiotic resistance. Antibiotic-resistant pathogens in CLABSI cases complicate treatment, leading to longer hospital stays, increased healthcare costs, and higher mortality rates. These infections require more complex and expensive treatment regimens, as first-line antibiotics may no longer be effective. The overuse and misuse of antibiotics contribute to this resistance, making it imperative for healthcare facilities to implement stringent infection control practices and antibiotic stewardship programs to mitigate the spread and impact of resistant infections.
Extending Lengths of Stay
CLABSIs significantly extend hospital stays due to their complexity and severity. Patients with CLABSI often require prolonged antibiotic treatments, which not only increases medication use but also raises the risk of developing antibiotic-resistant infections. The extensive medical care and monitoring required add substantial costs to the treatment and management of CLABSI. Secondary complications, such as sepsis and organ dysfunction, can arise, necessitating additional medical interventions and resources. Overall, CLABSI leads to a considerable financial burden on healthcare systems due to extended hospitalization, increased antibiotic use, and the need to address secondary health issues.
Risk Factors
Several risk factors increase a patient’s vulnerability to CLABSI. Multilumen access catheters pose a higher risk due to multiple entry points for potential infection. The use of total parenteral nutrition (TPN) involves frequent and prolonged access to the central line, creating opportunities for microbial contamination. Patients undergoing chemotherapy and those who are immunosuppressed have compromised immune systems, making them less capable of fighting off infections. Prolonged catheterization duration also increases the likelihood of microbial colonization and subsequent infection. Effective prevention strategies, including stringent aseptic techniques, regular assessment of catheter necessity, and meticulous catheter care, are essential to mitigate these risk factors and reduce the incidence of CLABSI.
Reducing CLABSIs
The Agency for Healthcare Research and Quality (AHRQ) outlines several evidence-based steps to reduce Central Line-Associated Bloodstream Infections (CLABSIs) in hospitals. These steps include the following:
- Appropriate hand hygiene
- Chlorhexidine for skin preparation
- Full-barrier precautions during catheter insertion
- Avoiding the femoral vein for catheter placement in adult patients
- Prompt removal of unnecessary catheters
By implementing these guidelines, hospitals can effectively lower CLABSI rates and improve patient outcomes.
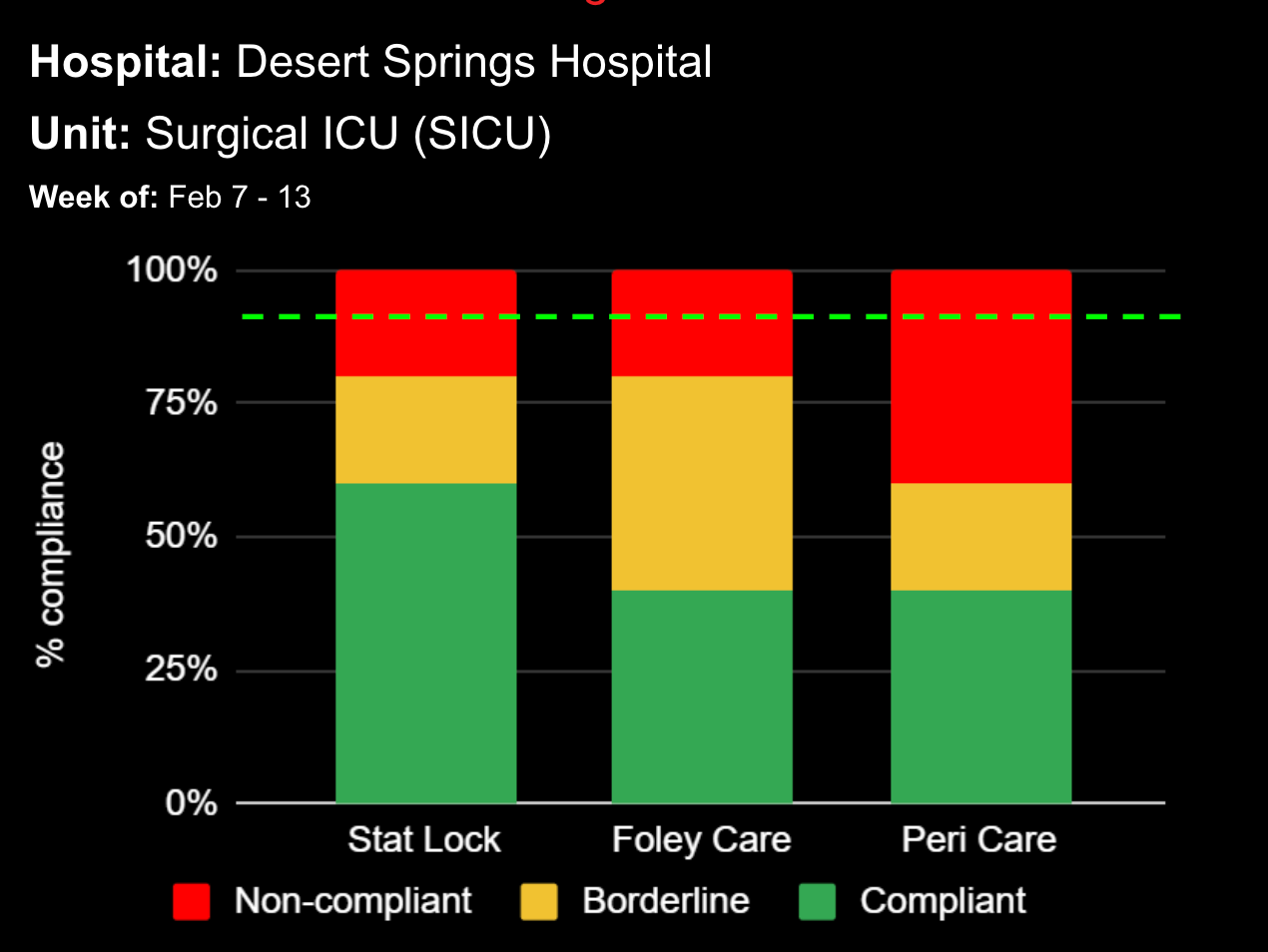
AHRQ also recommends several post-insertion steps to reduce CLABSIs. After inserting the central line, a sterile dressing should be applied immediately to the insertion site, with transparent dressings preferred for better site visualization unless the site is oozing. Dressings should be replaced if they become damp, loosened, or soiled, or after inspecting the site. Antimicrobial ointments are not recommended as they do not reduce CLABSI incidence. These steps, along with meticulous care and adherence to aseptic techniques, are vital in minimizing infection risk and ensuring patient safety.
Clinical Decision Support Systems
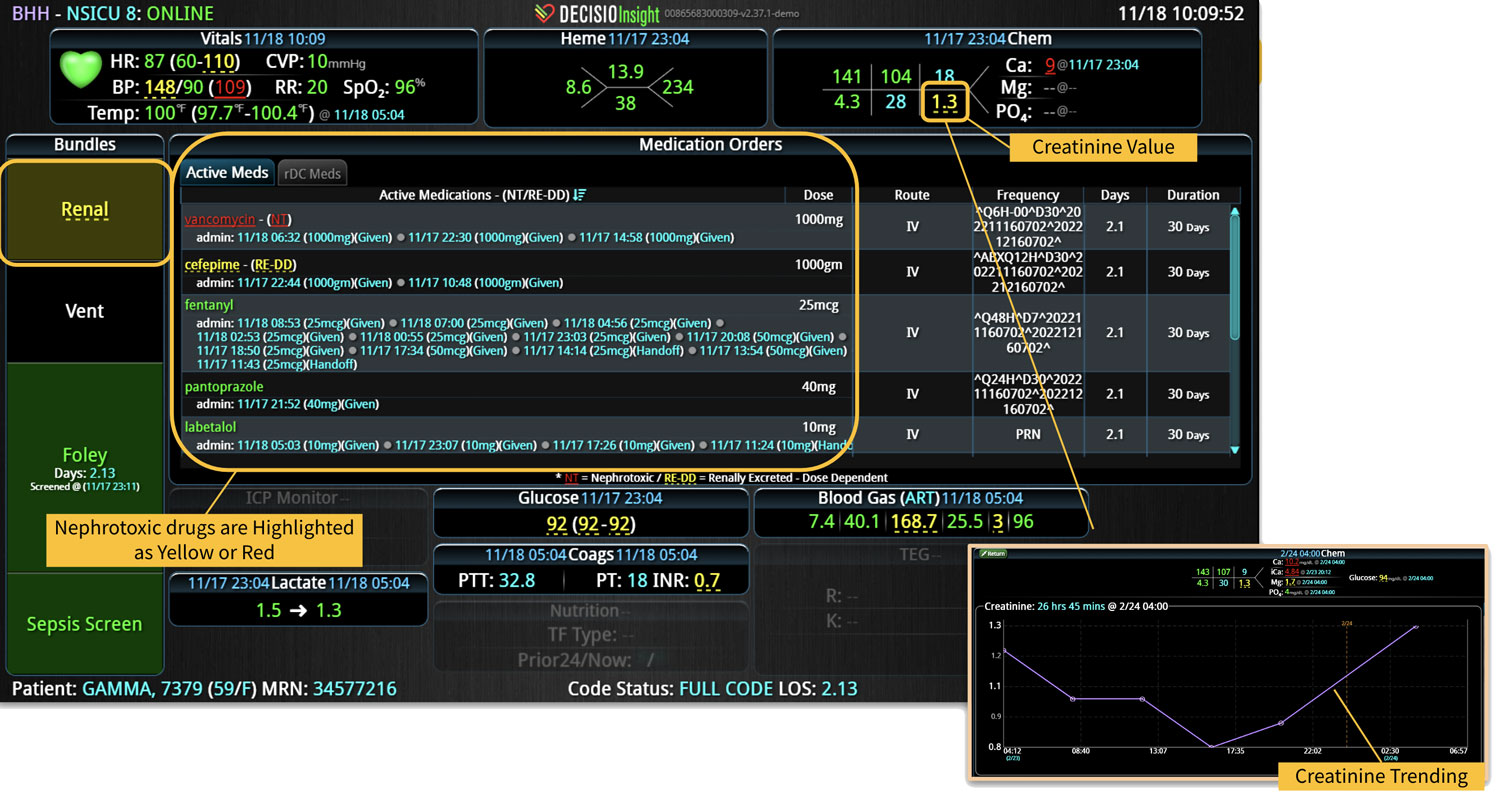
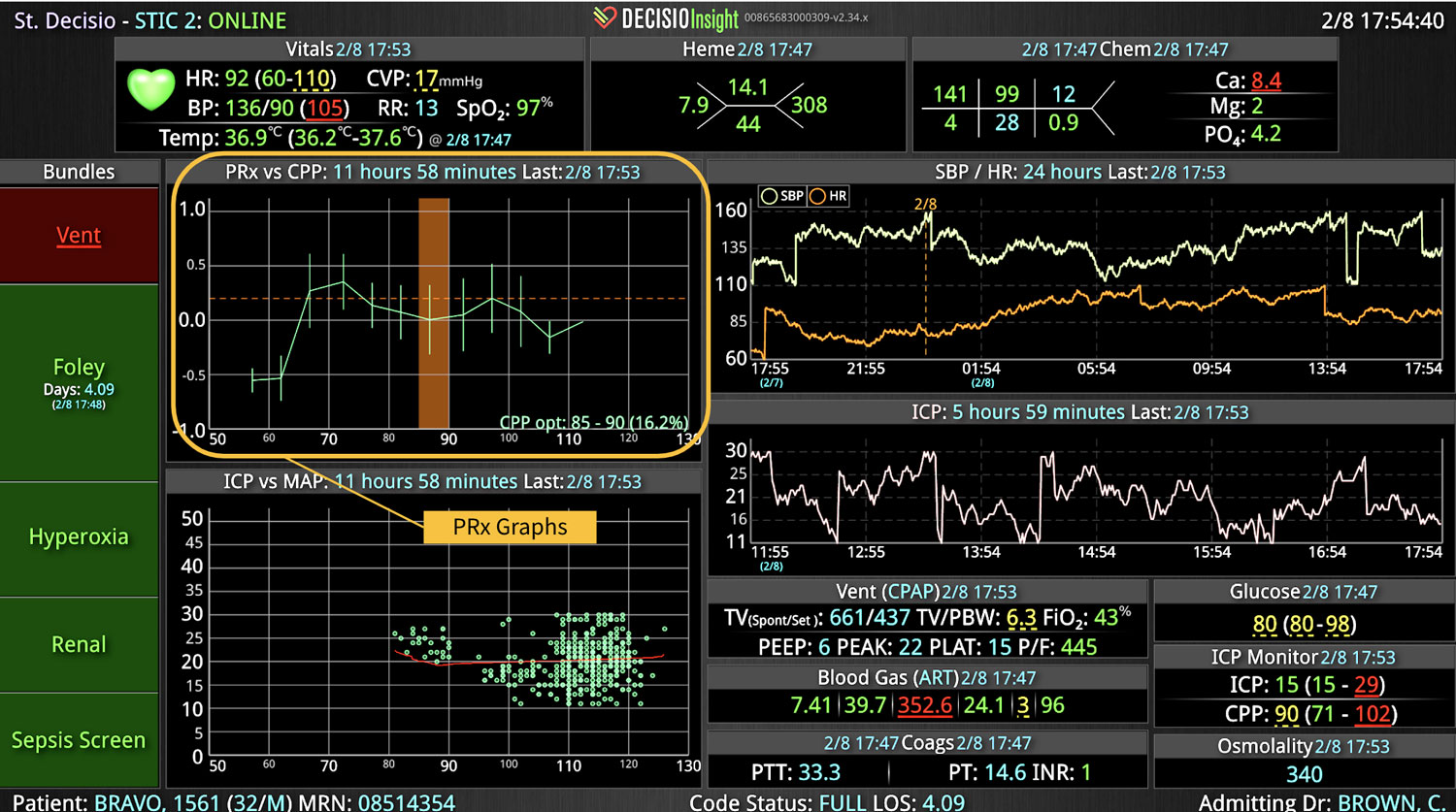
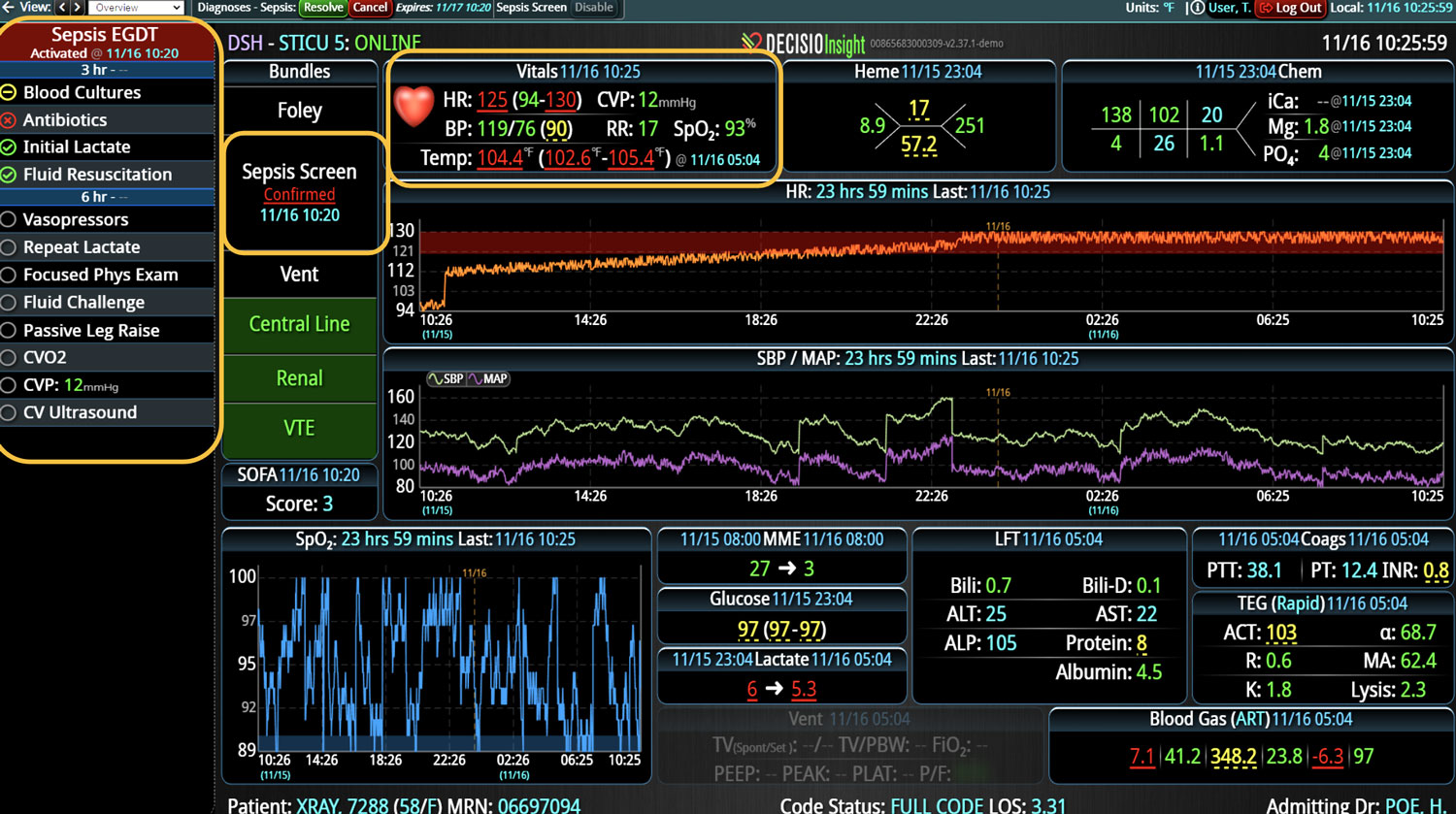
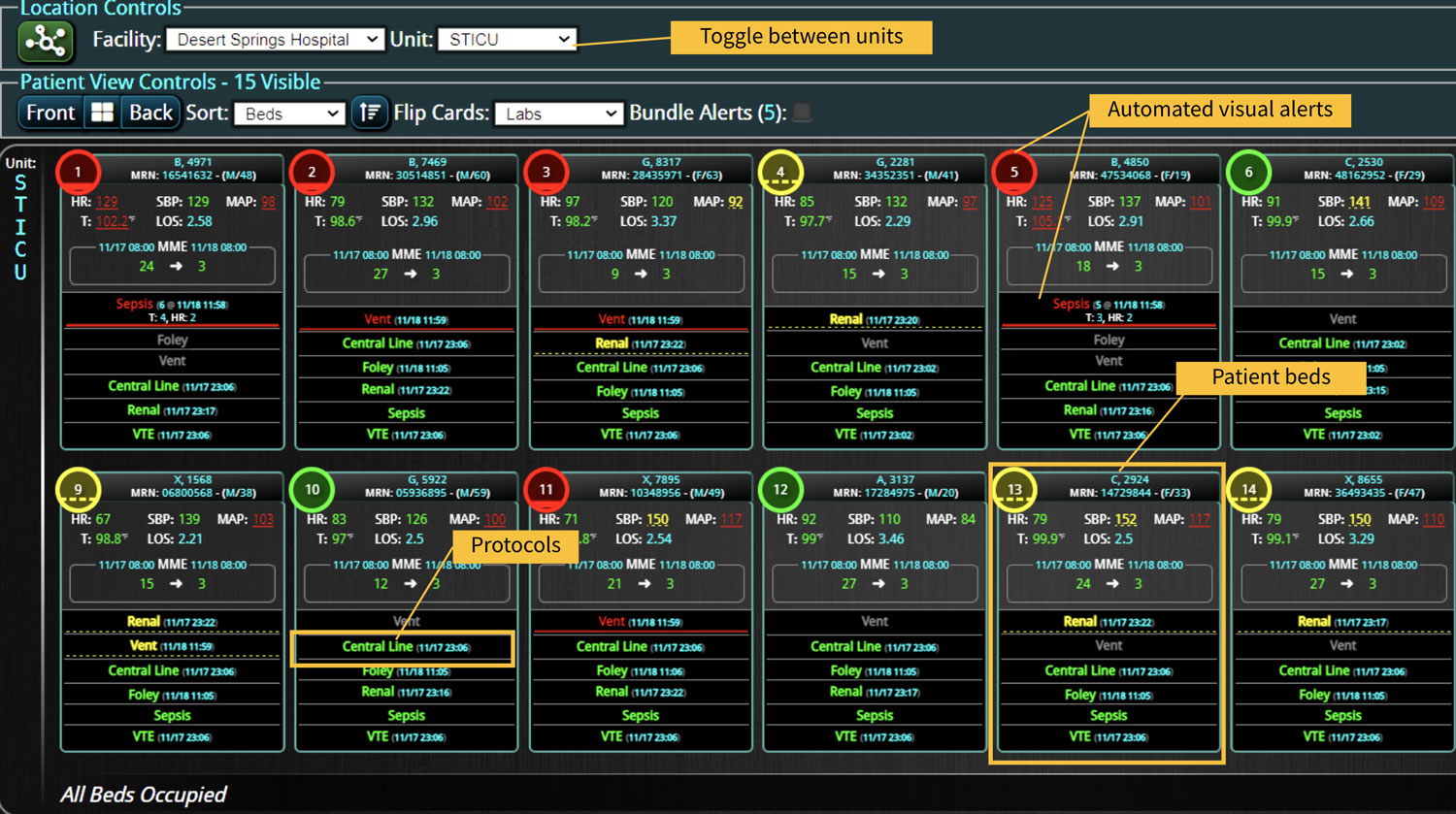
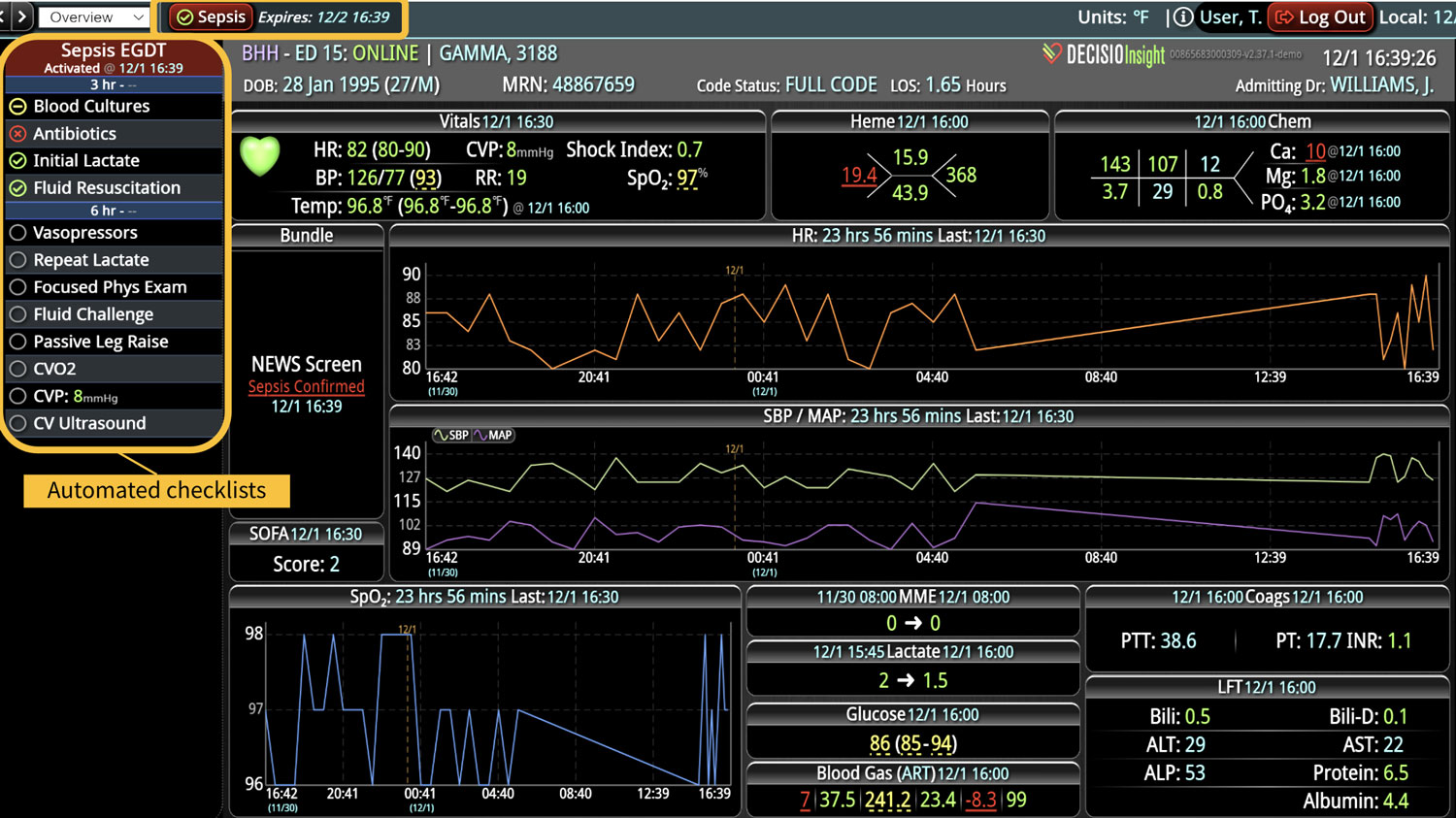
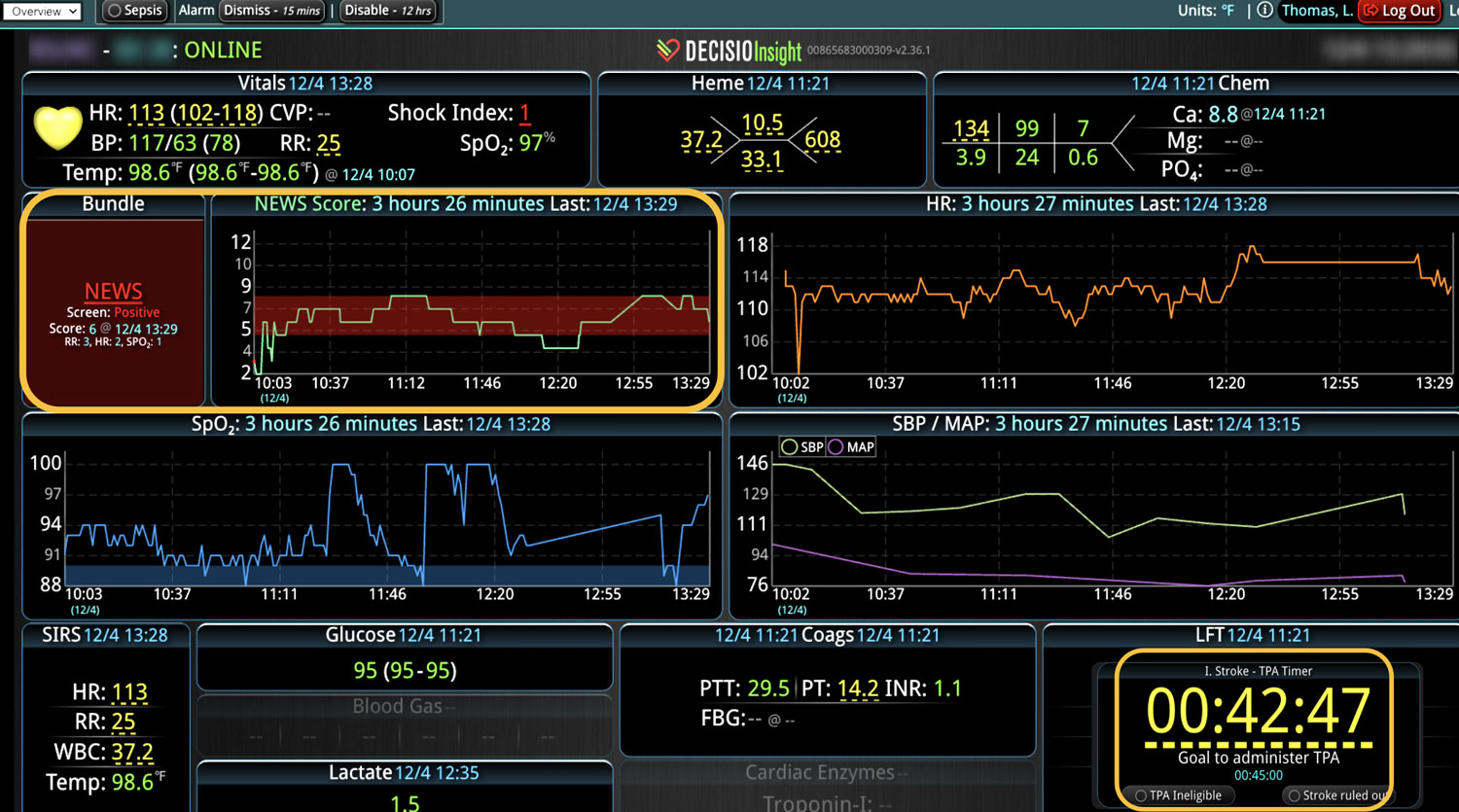
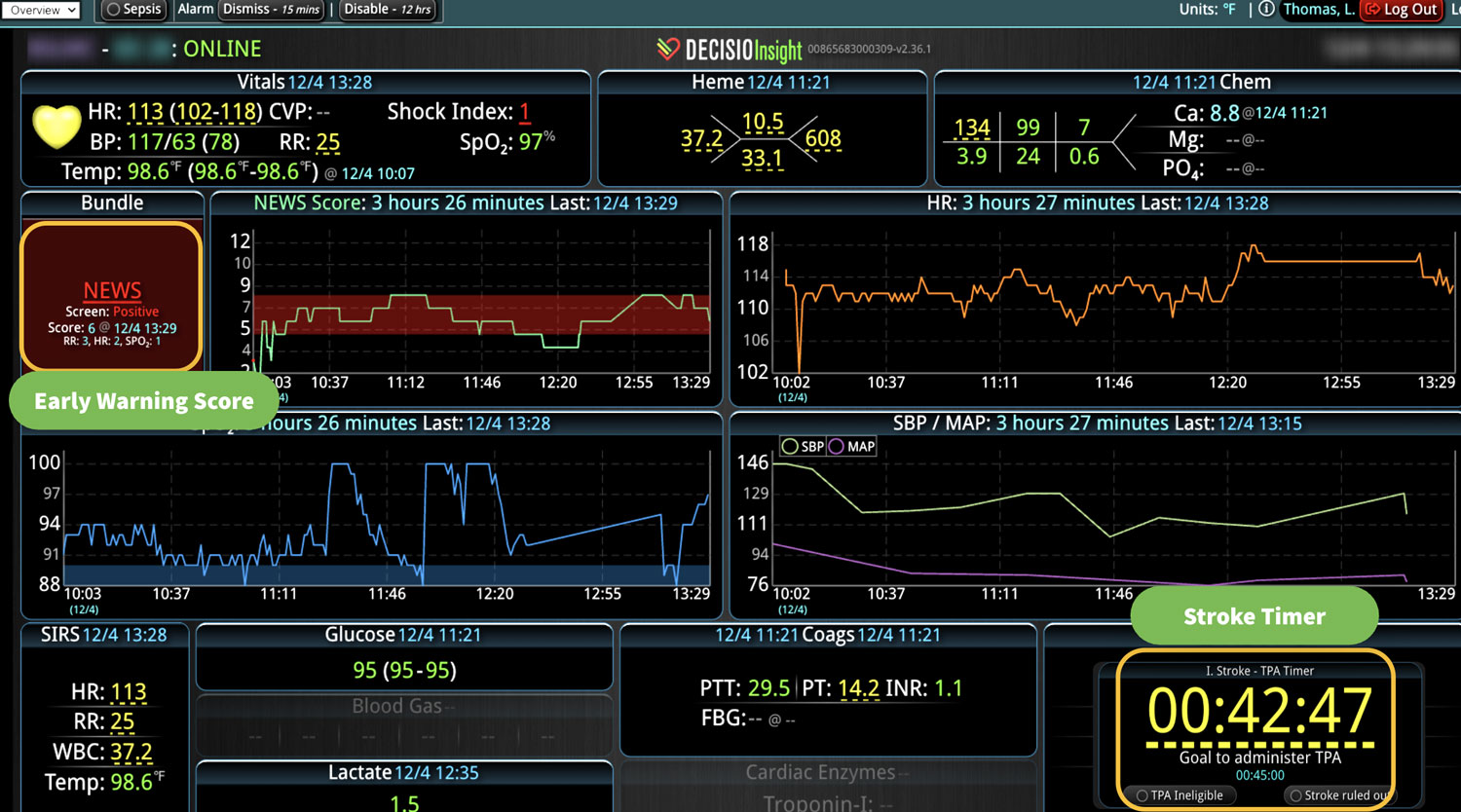
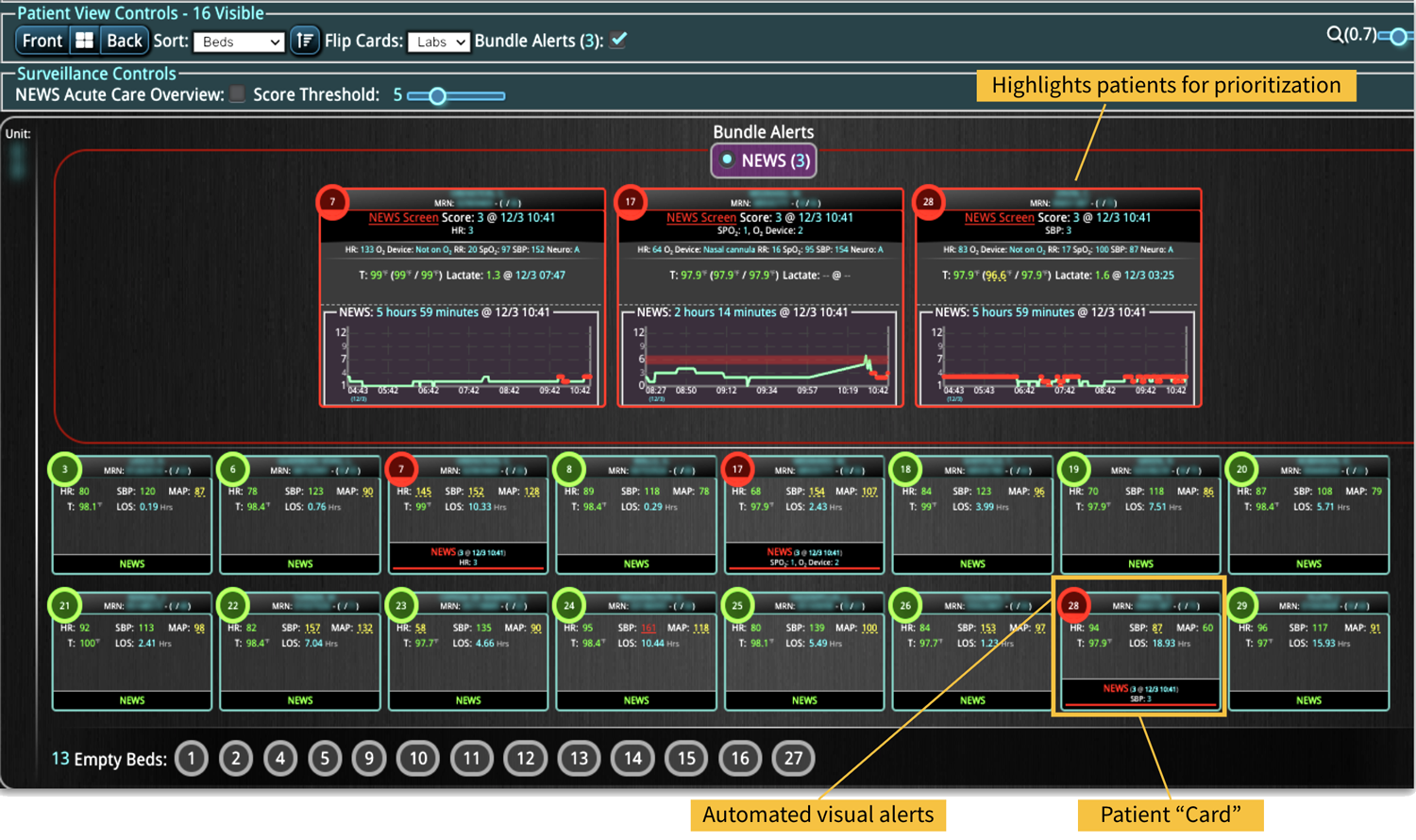
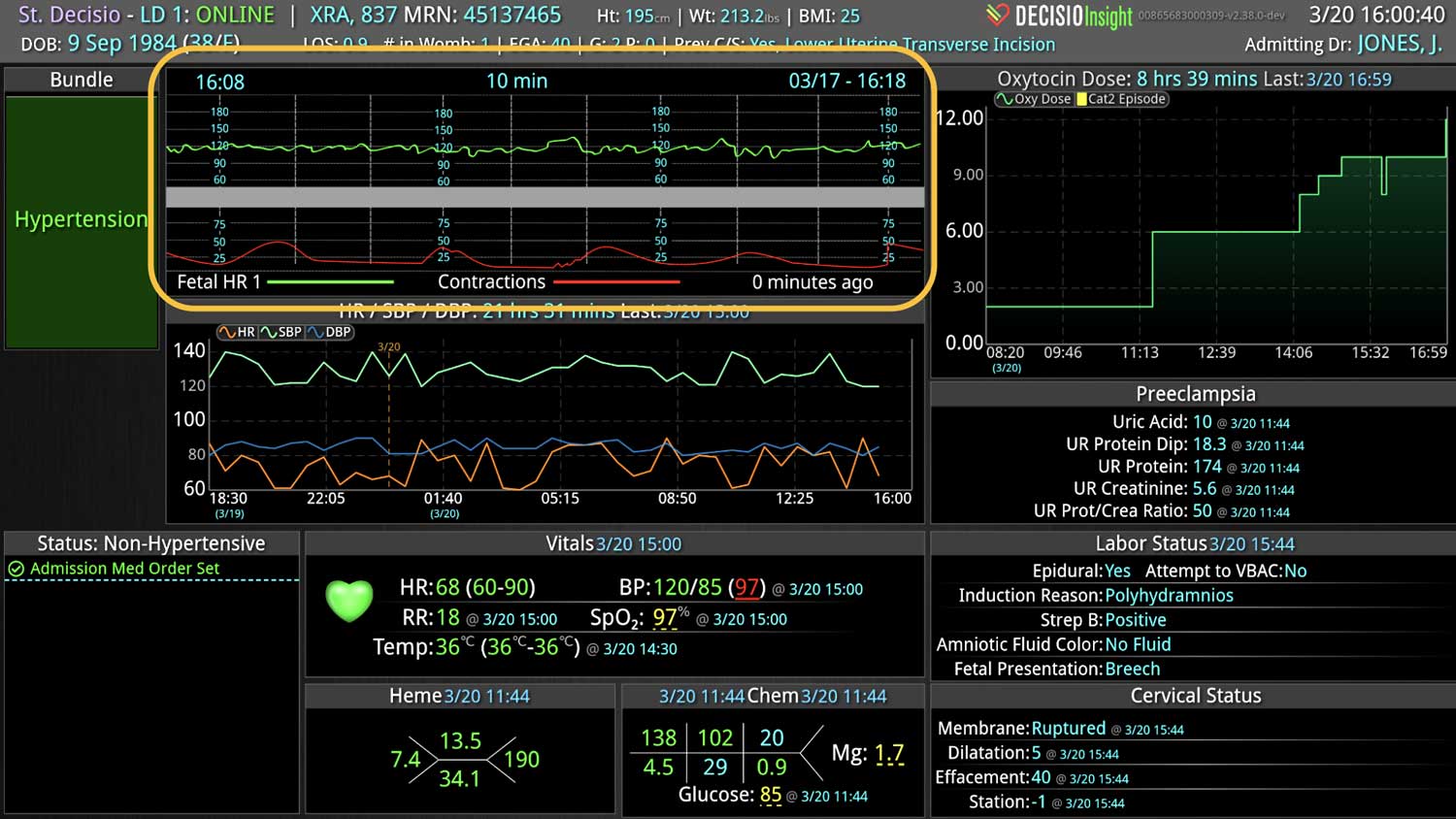
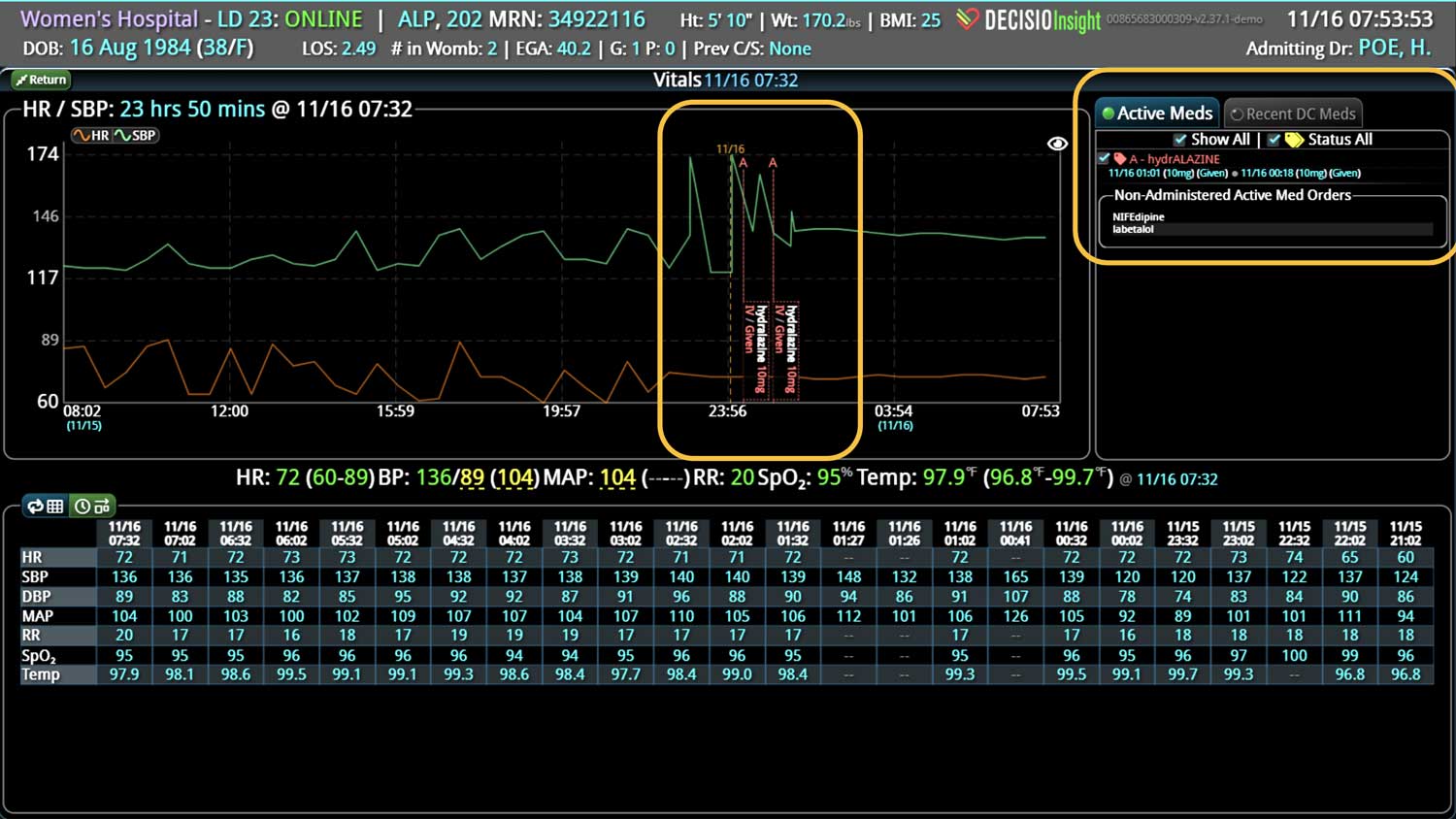
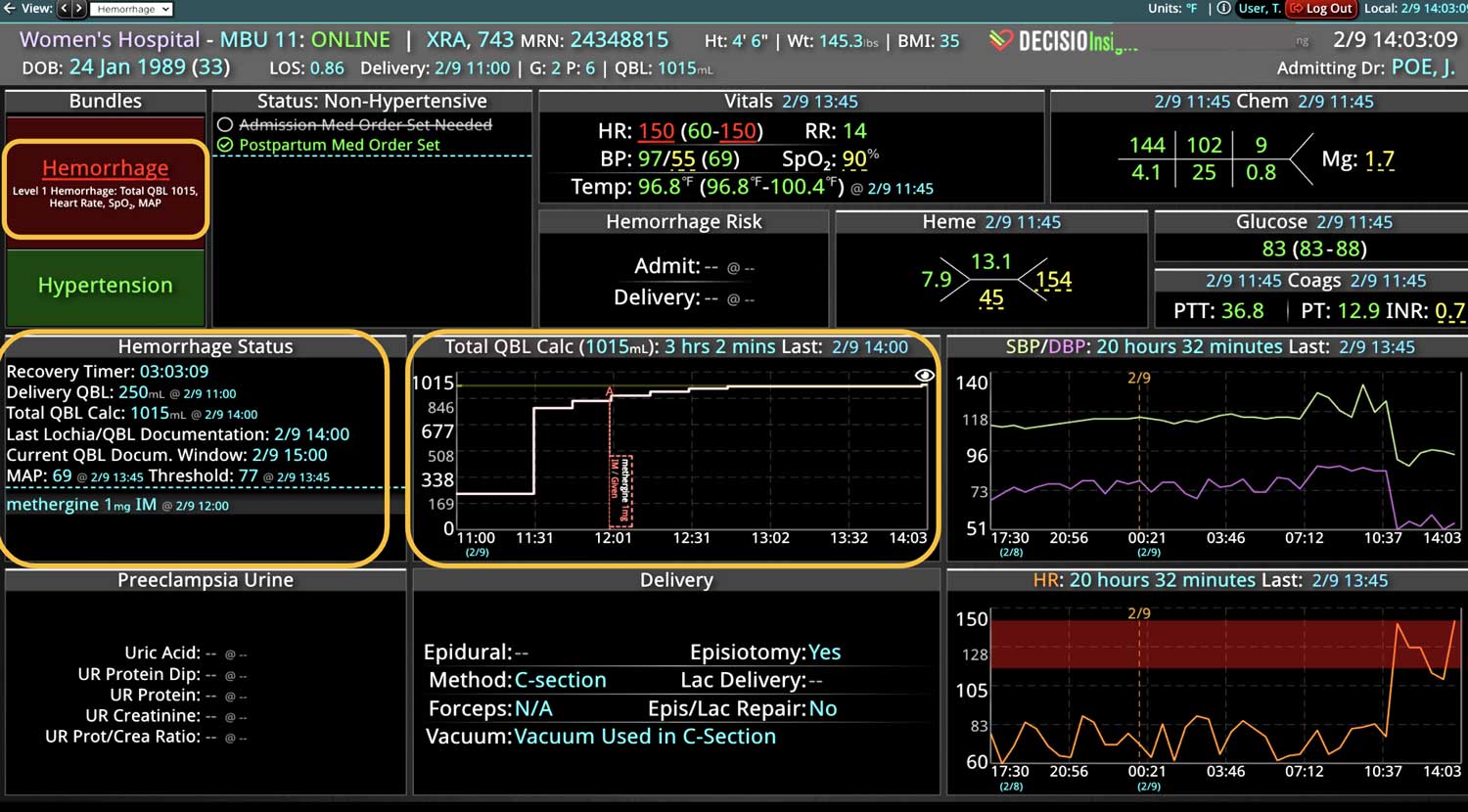
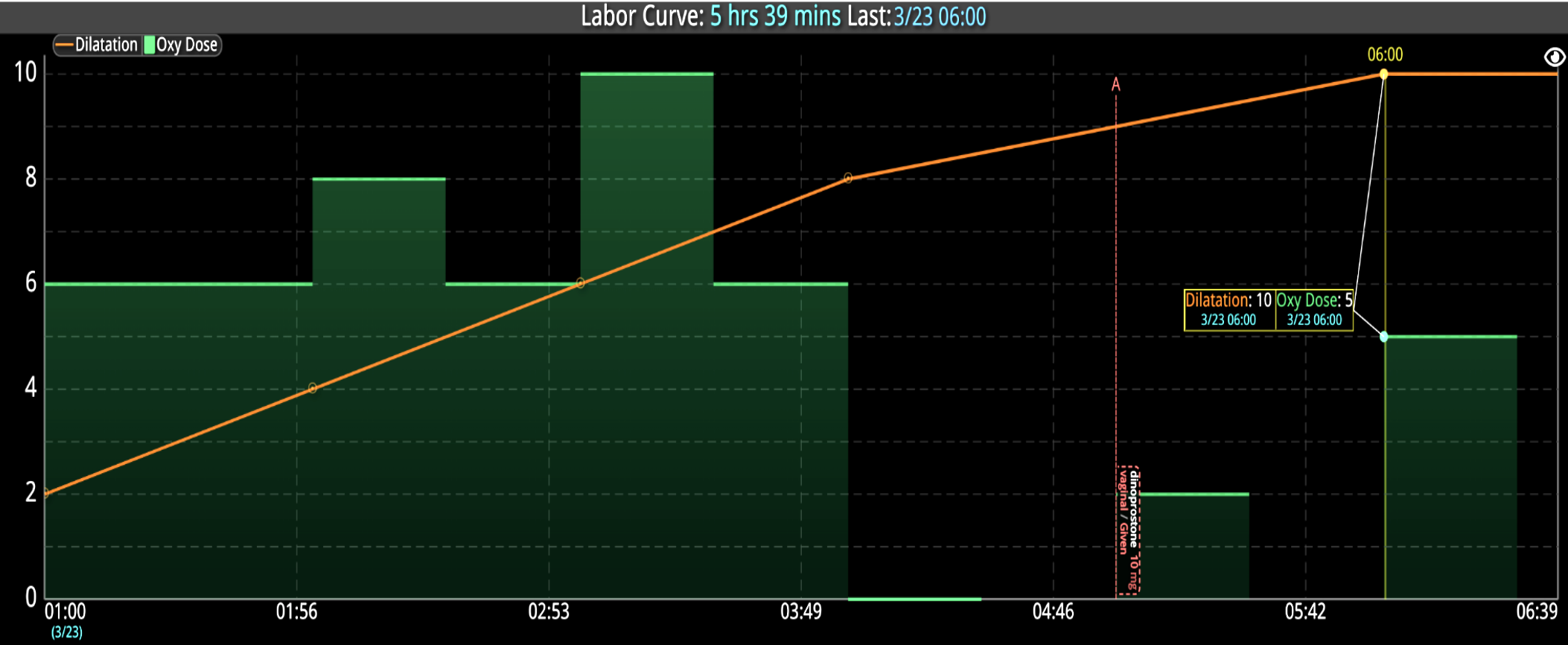
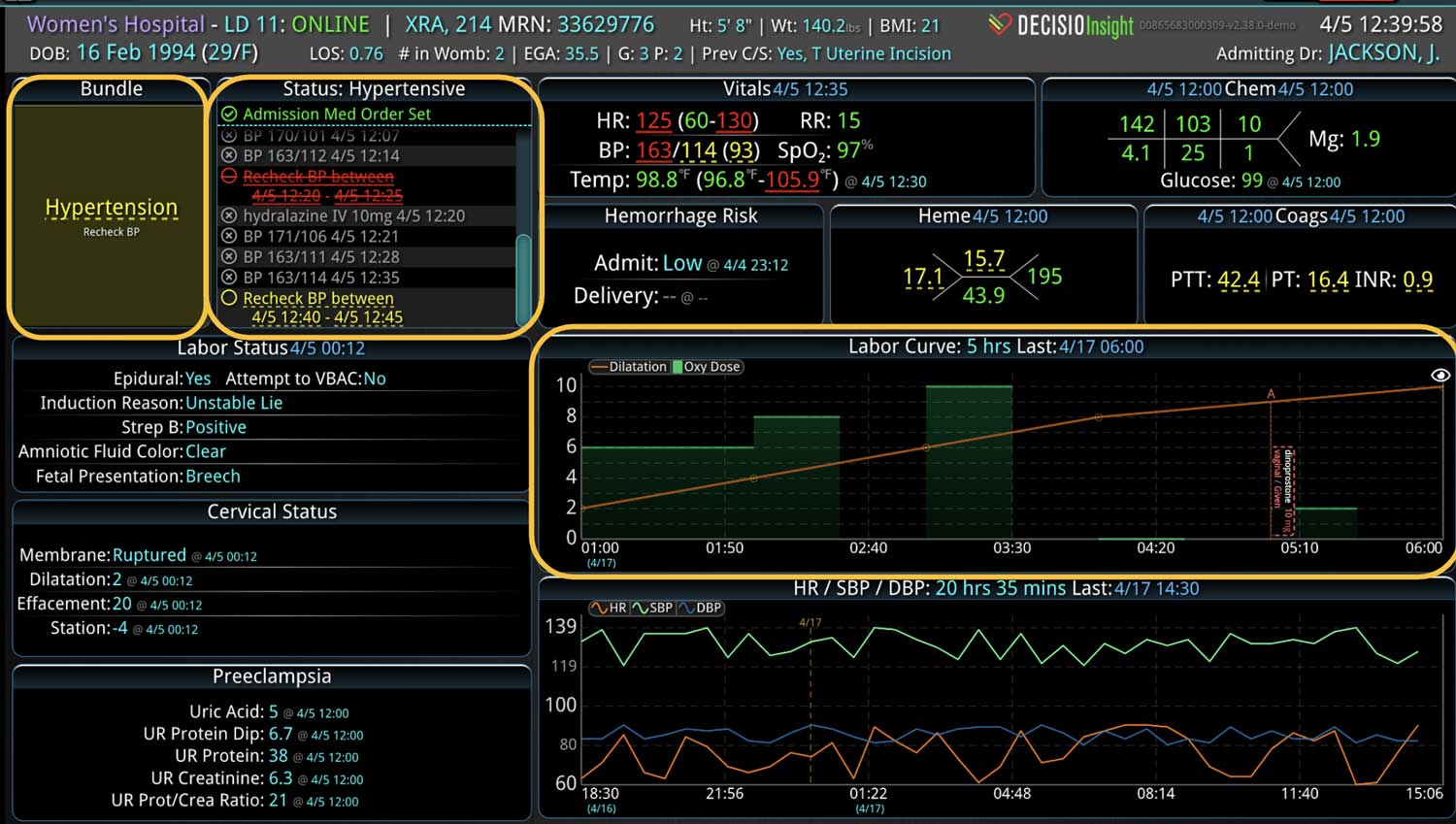
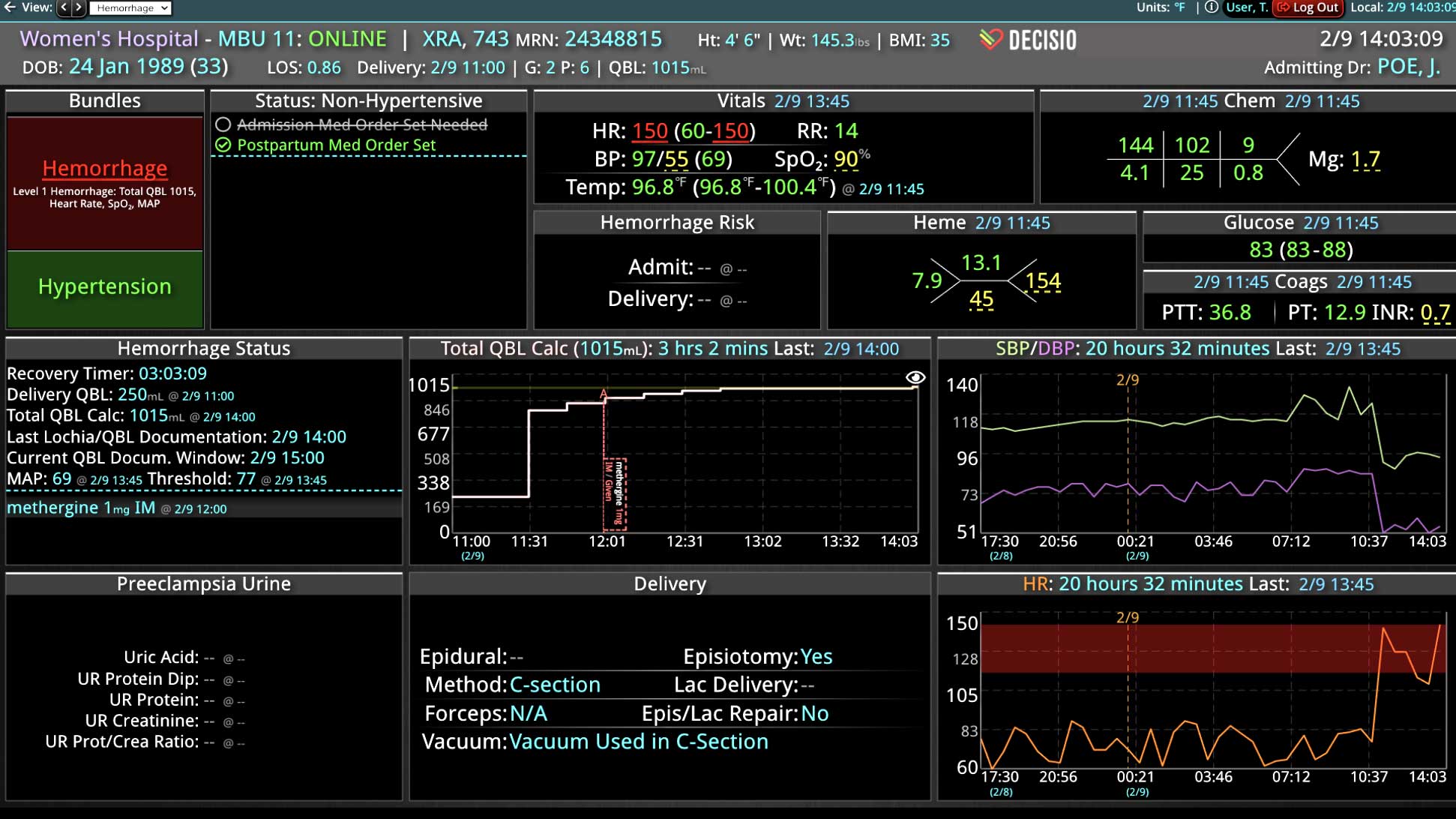
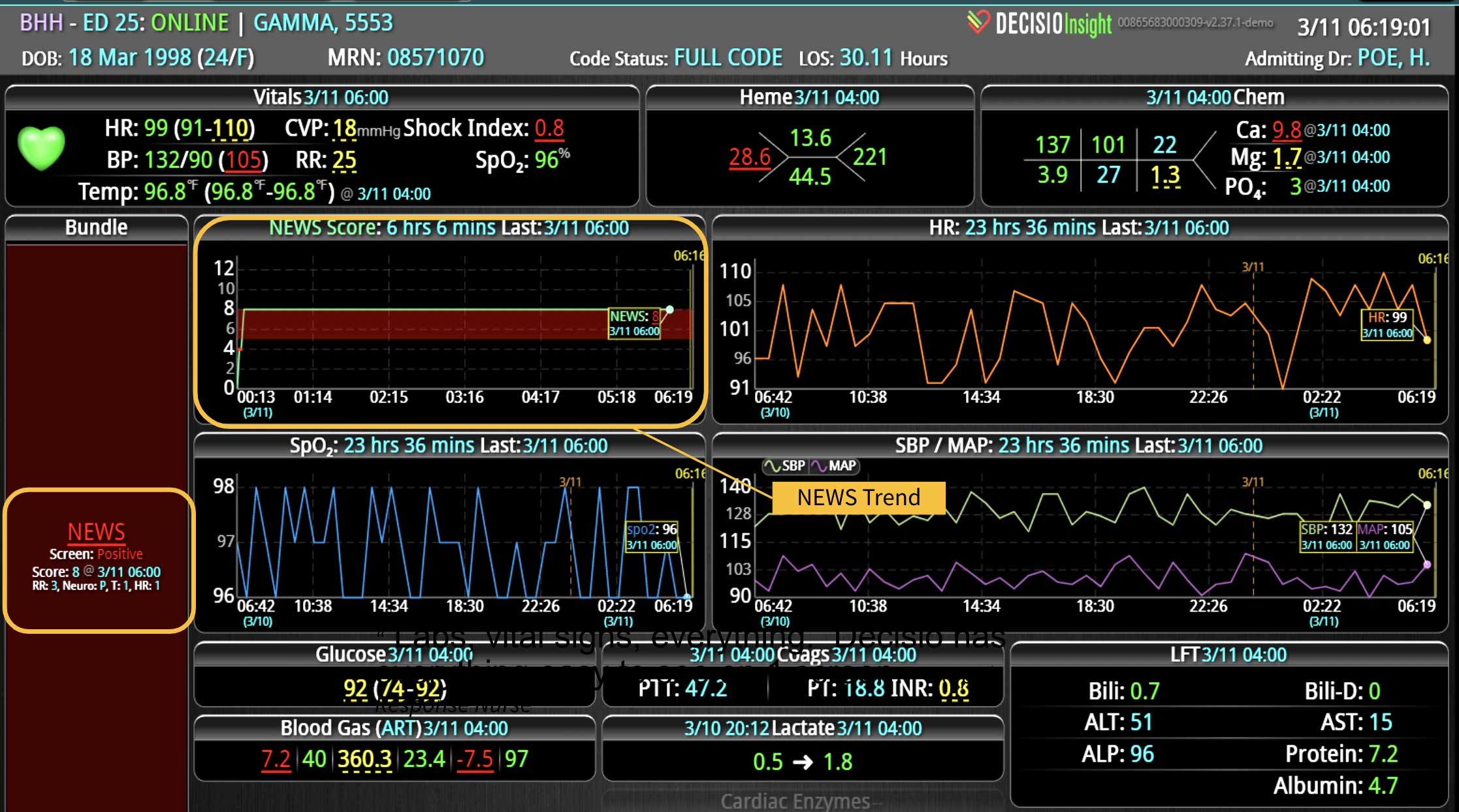
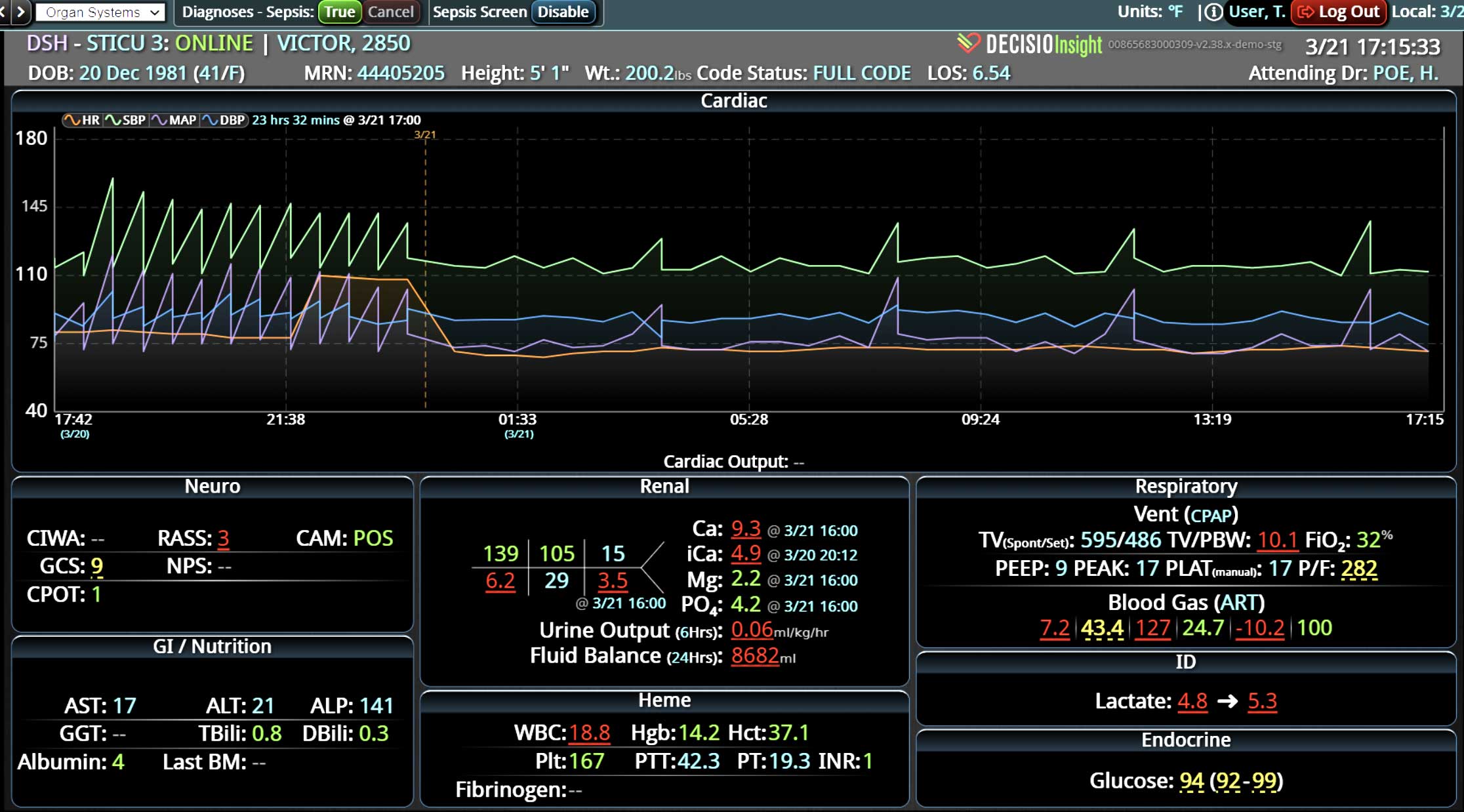
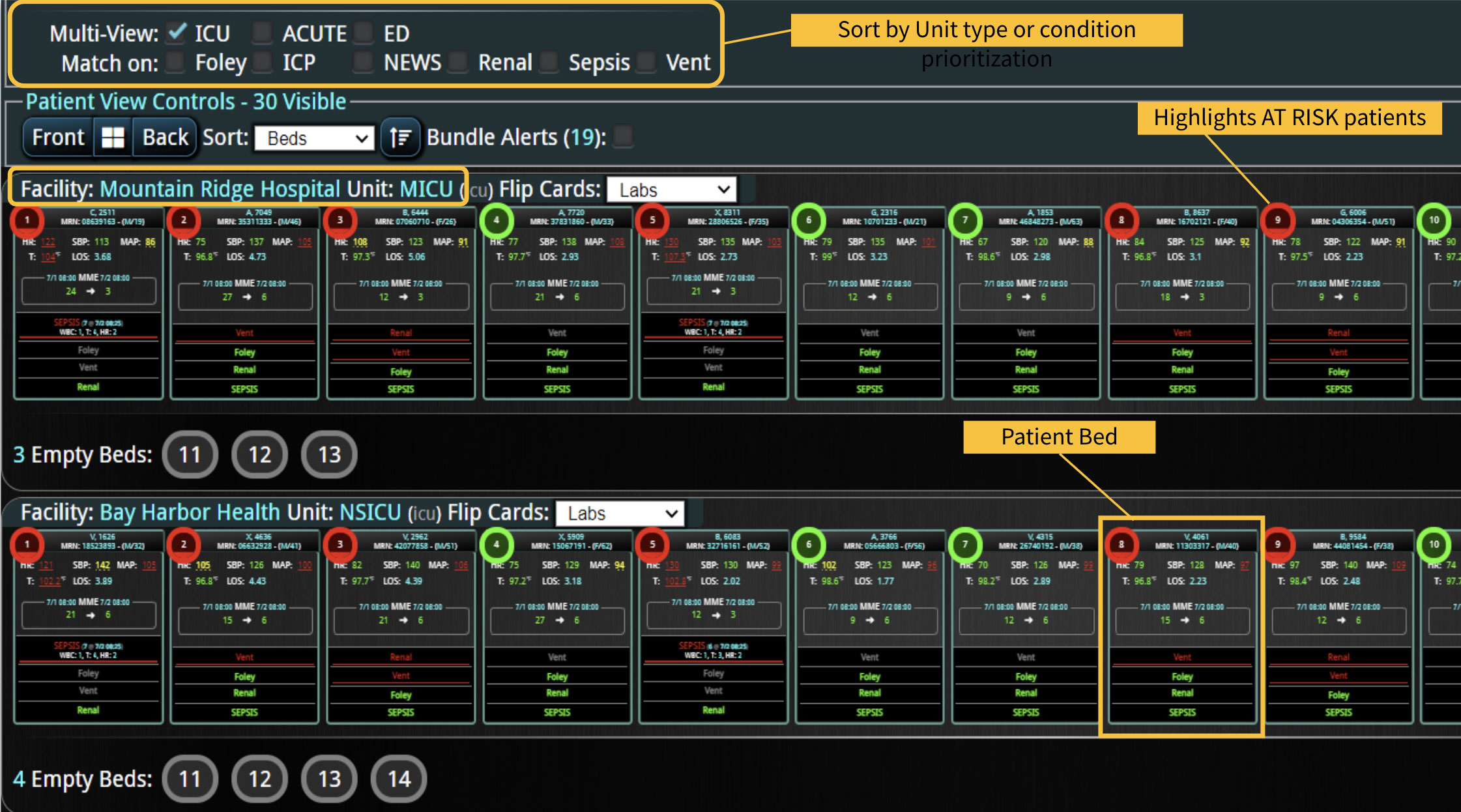
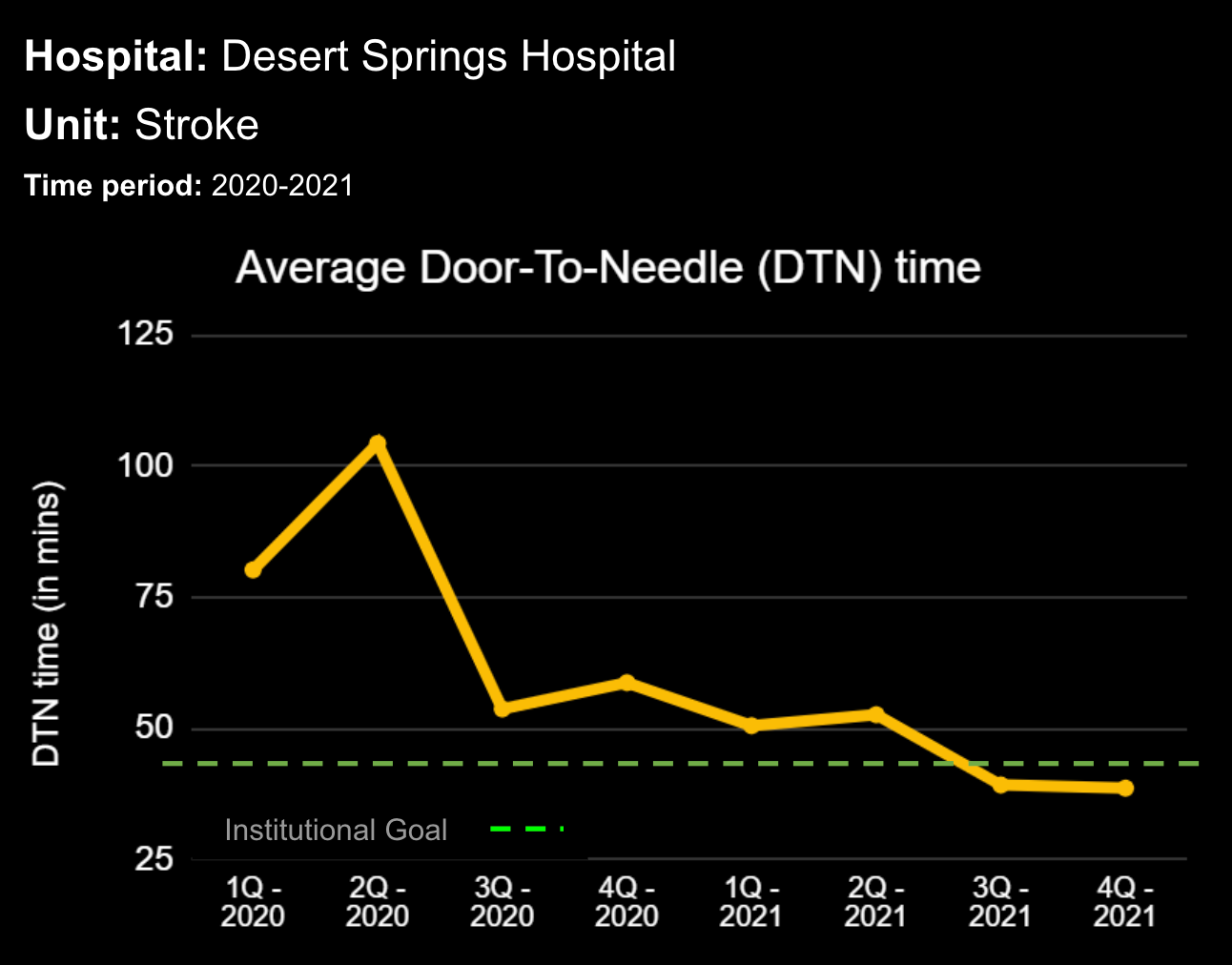
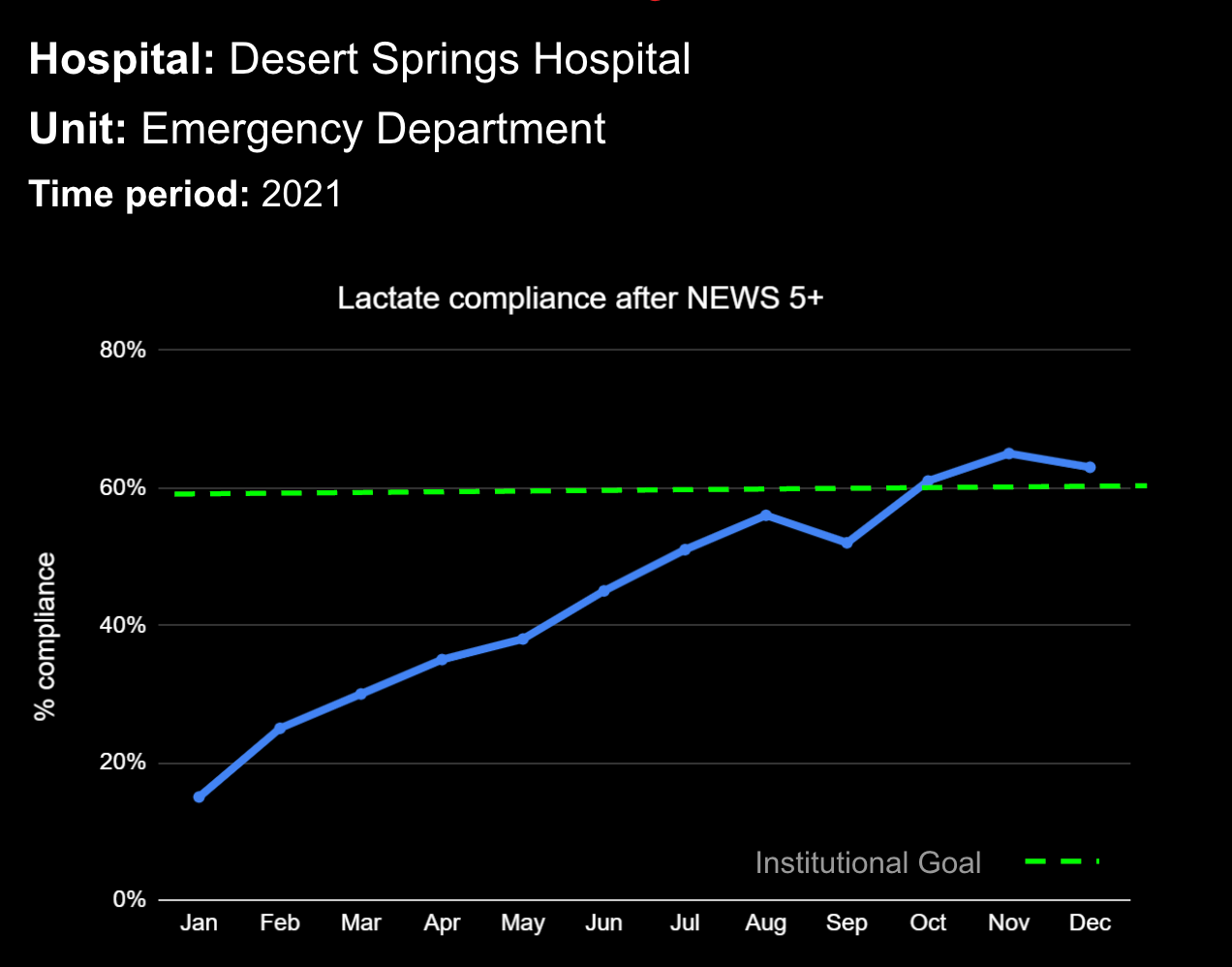
Clinical decision support systems are critical in helping clinical teams manage central line’s in hospitals. Our solution, InsightIQ, enables near real-time monitoring and visualization, helping healthcare providers to promptly identify and track the status of a central line. InsightIQ integrates with electronic health records to provide continuous updates on catheter duration, care, and patient conditions, facilitating early detection of potential complications. This information is accessible in a single view for an individual patient, a specific hospital unit, an entire facility, and even patients across multiple facilities.
Our software solution, combined with a virtual nursing team, can provide bedside nurses with the support needed to identify catheters requiring attention. Virtual nursing solutions enhance care by offering remote oversight and intervention, ensuring adherence to best practices and timely removal of unnecessary catheters. Together, these systems improve patient safety, reduce catheter-related infection incidence, and enhance overall care quality.
Learn more About How we help clinicians improve patient outcomes
Schedule a call with our team to discuss how we are helping our clients revolutionize how clinicians manage patient interventions.