08 Aug Early Warning Scoring Systems: Got Smart Bioanalytics?

Early Warning Scoring Systems: Got Smart Bioanalytics?
In medicine, every second counts. A patient can be stable one minute and crash during the next moment. Early detection, timeliness, and competency of clinical response are a triad of determinants that impact clinical outcomes of people with acute illness. Results from observational studies confirm that patients often show signs of clinical deterioration during the 24 hours before a severe event requiring clinical intervention.1
Timely detection of those subtle clinical warning signs has its own set of challenges. When those clinical values (especially vital signs) cross a critical threshold, they usually alert the bedside staff via beeping monitors. Because of the volume of alerts and the mountain of tasks that bedside staff manage, many alarms are simply silenced in seemingly stable patients. Thus, a critical value is often lost and not documented in the EMR system. Documentation of an alert is another task that can be triaged and forgotten. In some cases, especially in non-critical care settings, critical (outlier/severe) values may not trigger an alert, or the vital signs may not be taken as frequently.
Automated capture of vital signs and real-time alerts could reduce the burden on bedside staff while increasing data capture. However, the intense amount and frequency of data that is generated via an automated capture system introduces new challenges. A system may need to filter what data is real versus noise. Automated data capture also leads to increasing sets of alarms and thereby alarm fatigue. Bedside staff can be overwhelmed with false alarms; thus, they must be able to triage which alarms are likely the most critical. Another challenge with some systems is the inability to capture more than just routine vital signs. Derangement of a single vital sign is just one factor and does not provide a complete picture of the patient’s condition. Because many systems are designed to alert based on a single clinical sign, a large portion of alerts require no action and mainly contribute to alert fatigue.
To address these set of challenges, Early Warning Scores (EWS) were developed.2 Most EWS uses physiologic and weighted parameters to create a composite score that determines the criticality of the patient, also known as triage. The goal of all EWS is to identify those patients at risk before they decompensate. When an at-risk patient is identified, early interventions could reduce risks, enable timely transfers to the intensive care unit (ICU), or entirely prevent a catastrophic situation. Thus, hospital systems are testing, optimizing, and implementing early warning scoring systems (EWSS) whenever possible.
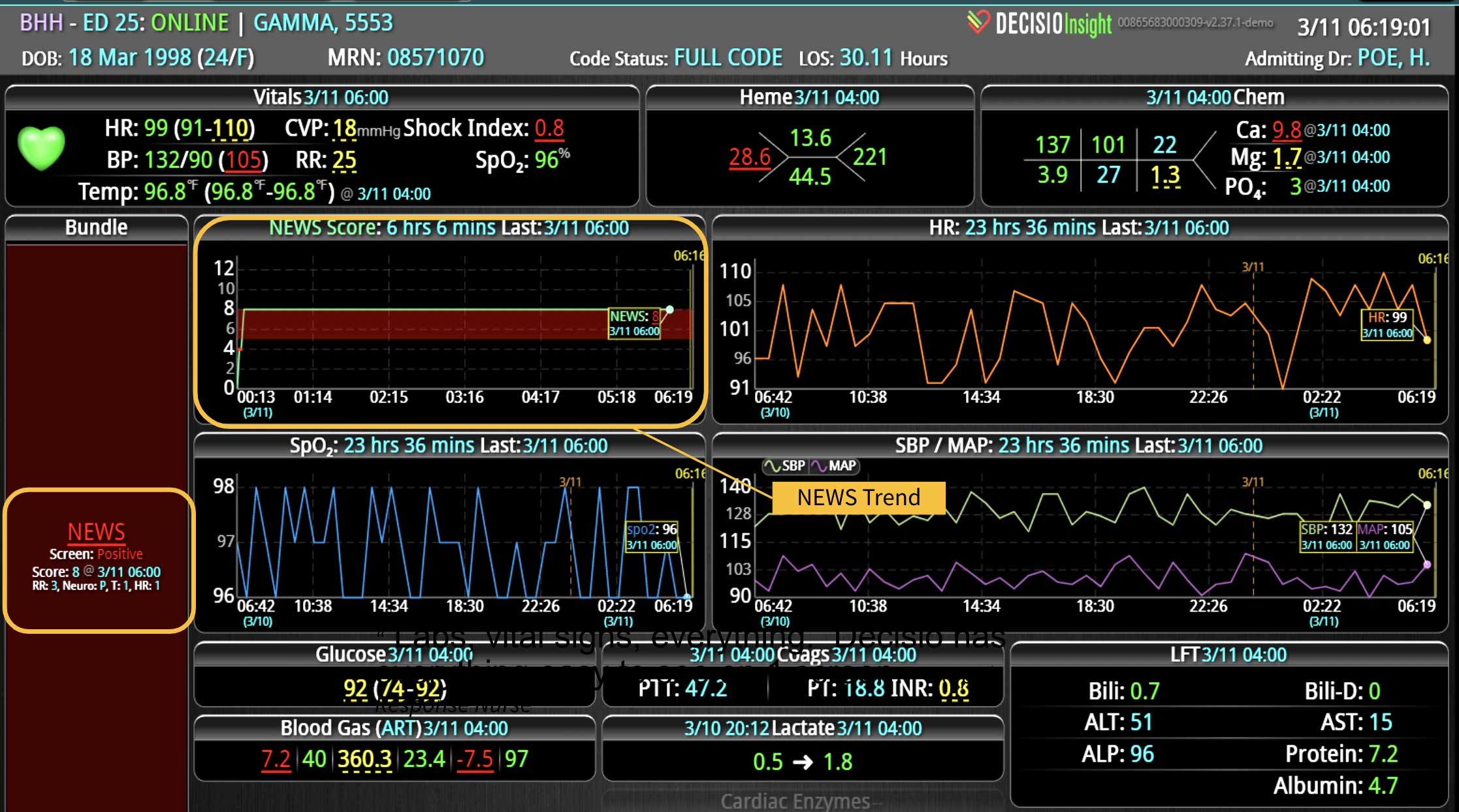
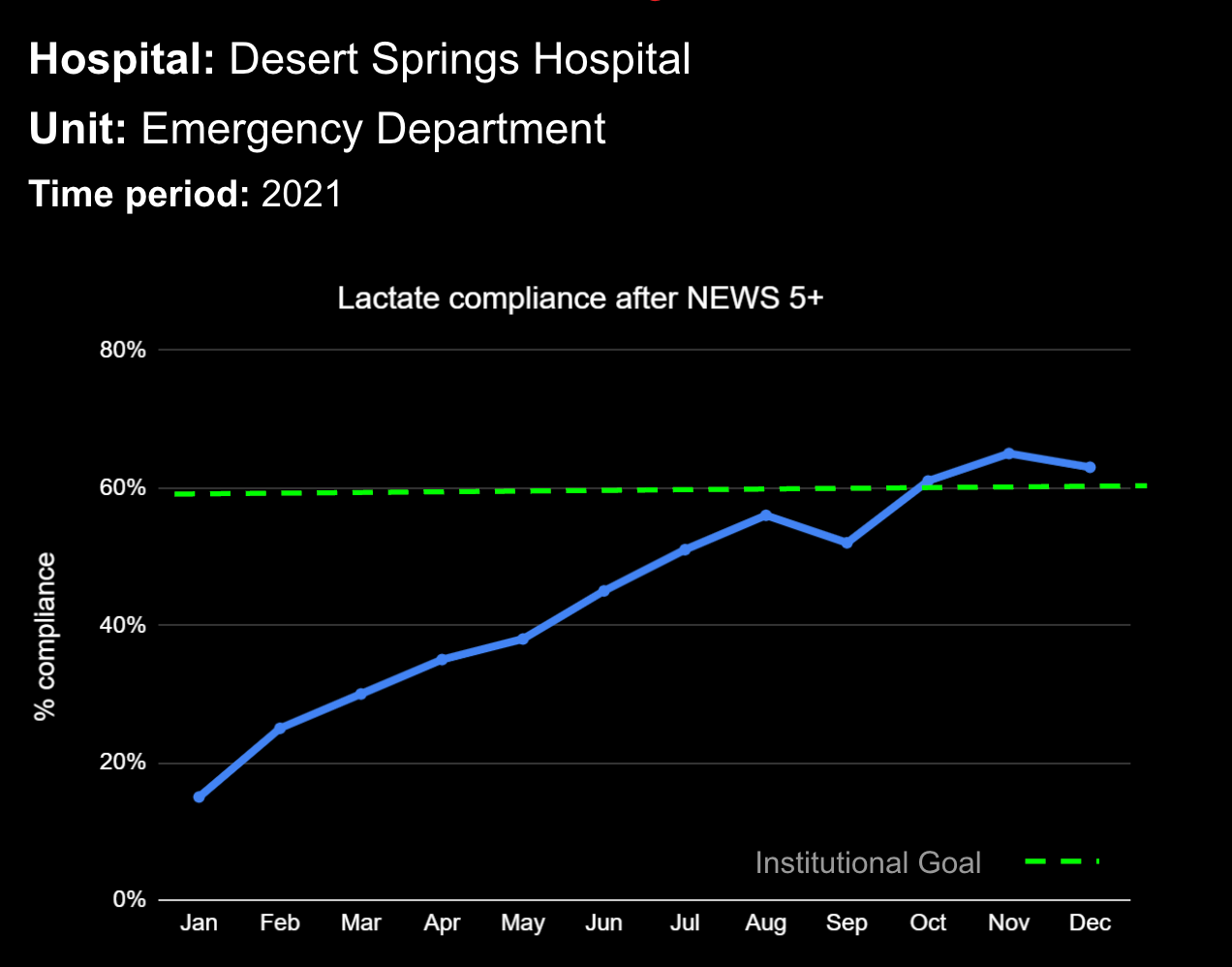
One of the first and most common EWS was the National Early Warning Score (NEWS),3 which was developed in the UK to triage patients during their Emergency Department (ED) visits. NEWS is a weighted composite of the first set of physiological parameters, oxygenation status, and neurological parameters on admission. The final score determines how serious the patient’s condition is. It’s simple to calculate and can be done in a matter of minutes. The same score can be utilized in hospitalized patients to determine their acuity during unit transfers or to monitor their progress during hospitalization. Depending on the patient population, NEWS can be very sensitive, which means it is not likely to miss a patient that may deteriorate; however, the score is not highly specific, so there is a very high likelihood of having a lot of false alerts.
To that regard, multiple variations of NEWS are being used with either a change in the weighted values, or by adding new patient variables. These modified early warning systems (MEWS) use similar data to predict impending decompensation or the need for ICU care. New EWSs are regularly introduced; each based on evidence and clinical need. Currently, a plethora of options are being validated and implemented. Each department or system may have its own go-to EWS for monitoring clinical inputs proven to predict decompensation or unfavorable outcomes in their population. Depending on the variables that make up the EWS score, they may require sophisticated calculation systems.
By monitoring a patient’s EWS, clinical deterioration signs can be identified before disaster strikes. While validated scoring systems have been tested in many hospital scenarios, calculating the score frequently can be cumbersome and often requires manual work from the bedside providers. Further, manual calculations are subject to common human errors. While a few EMR systems can calculate an EWS, they are often limited by data availability challenges. Some EMRs don’t have access to the data that is needed for the calculation, or they have an over-availability of data that can overwhelm the system. If the score requires coordinated time point collections, many EMRs cannot collect the needed information at the same time frame. This leads to reliability issues and introduces variability and inaccuracies in score calculation. Another challenge is that the alerts are still subject to bedside and chart visits. Some EMR systems only display an alert when a bedside staff opens the chart and not when the EWS crosses a critical threshold.
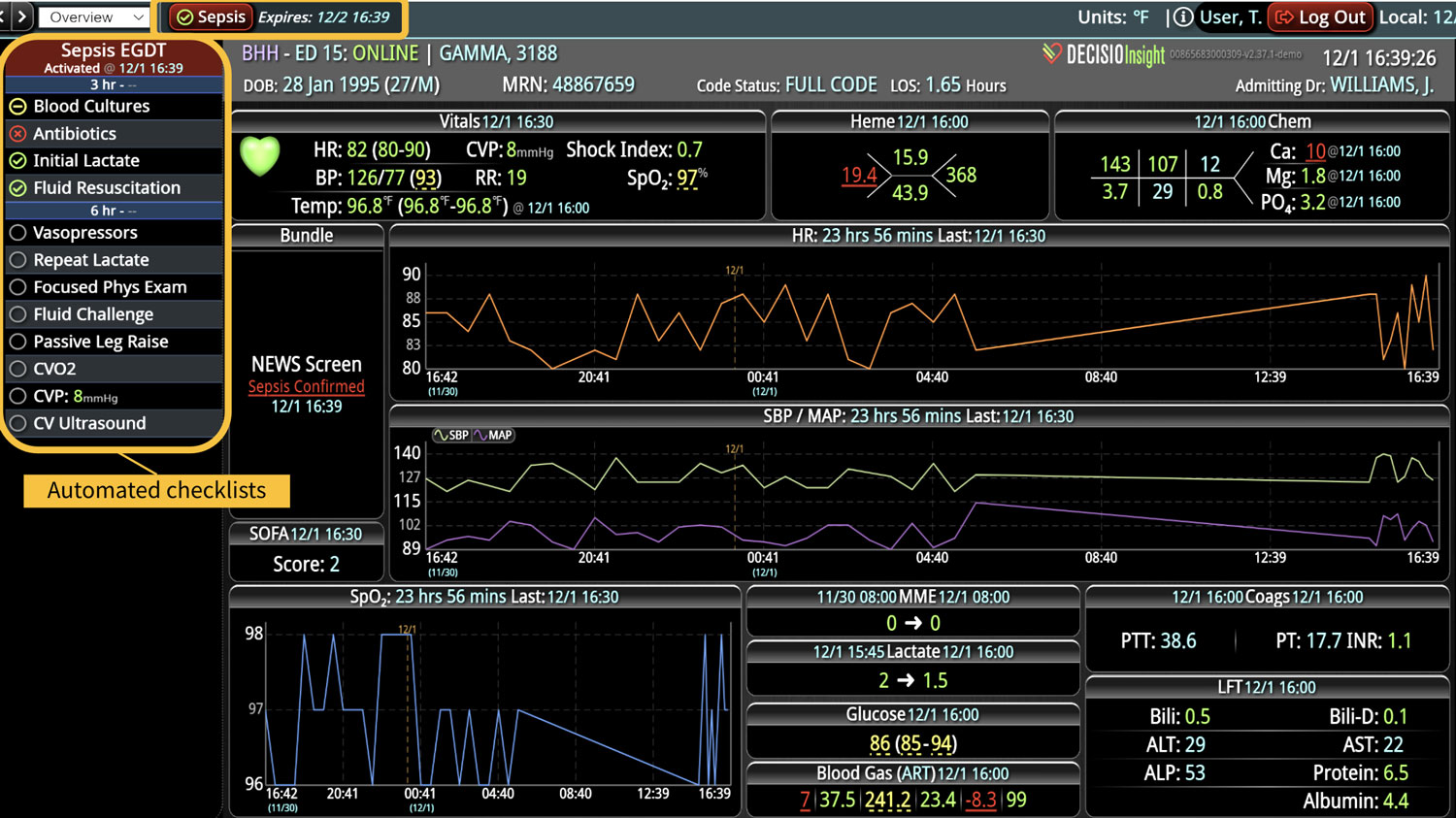
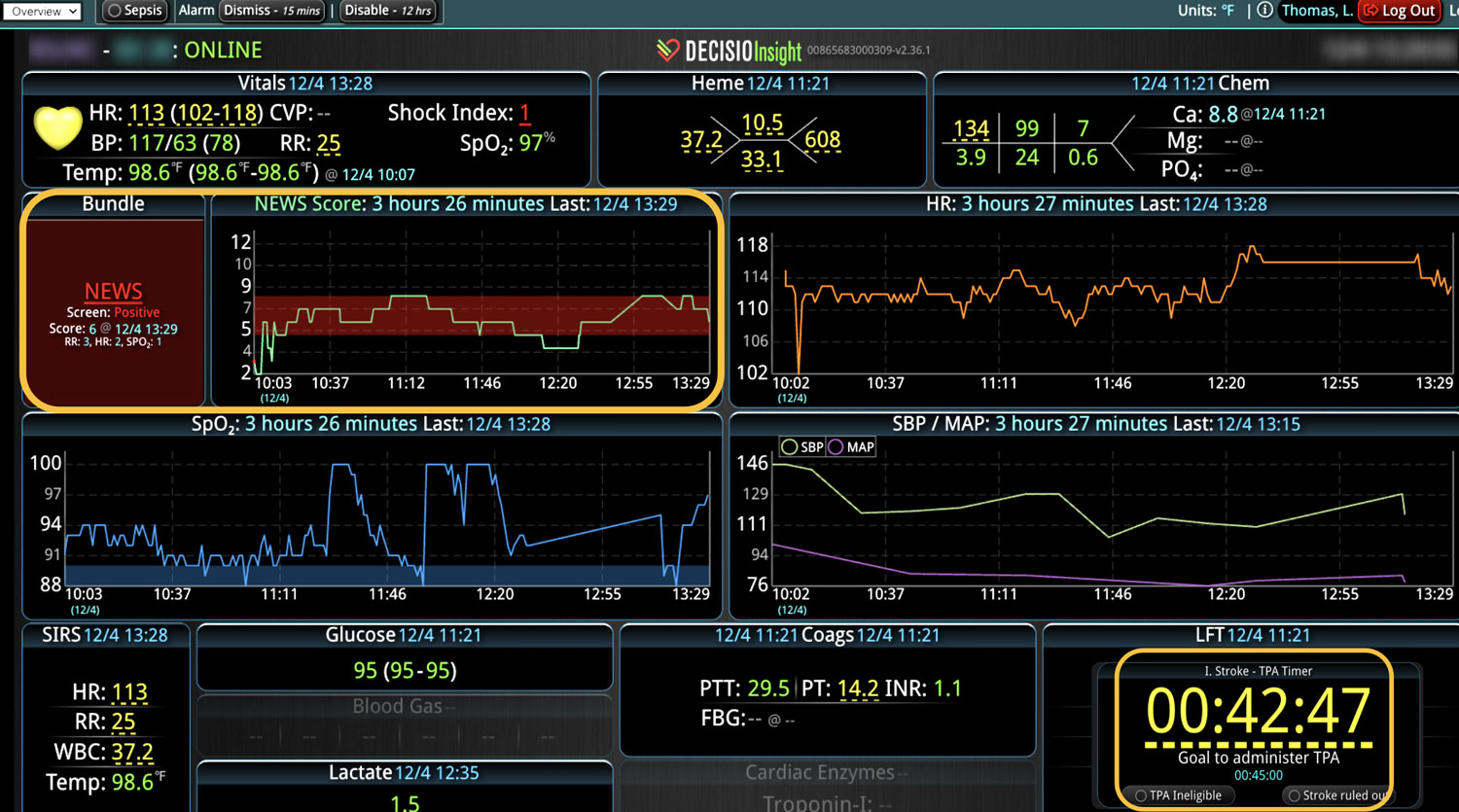
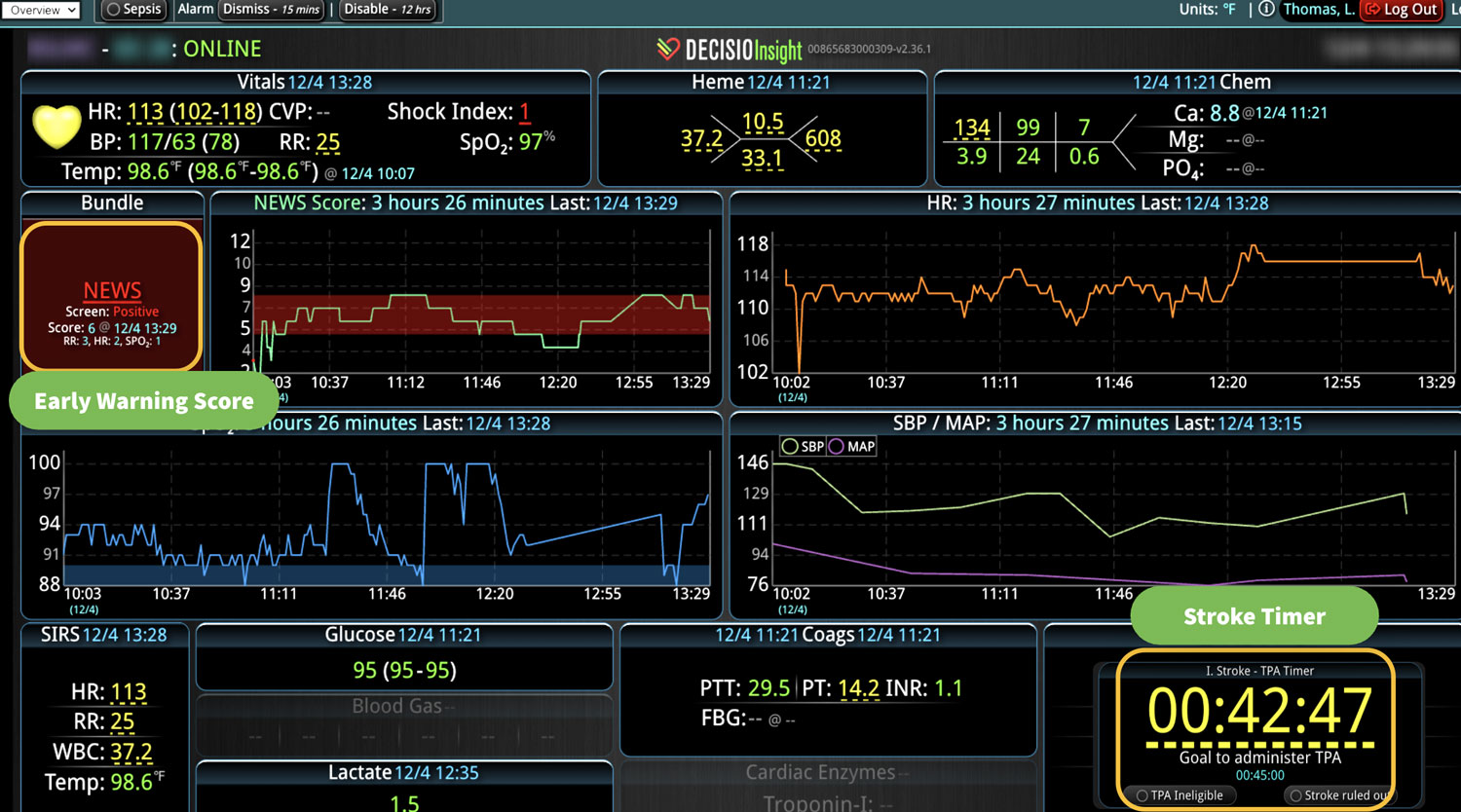
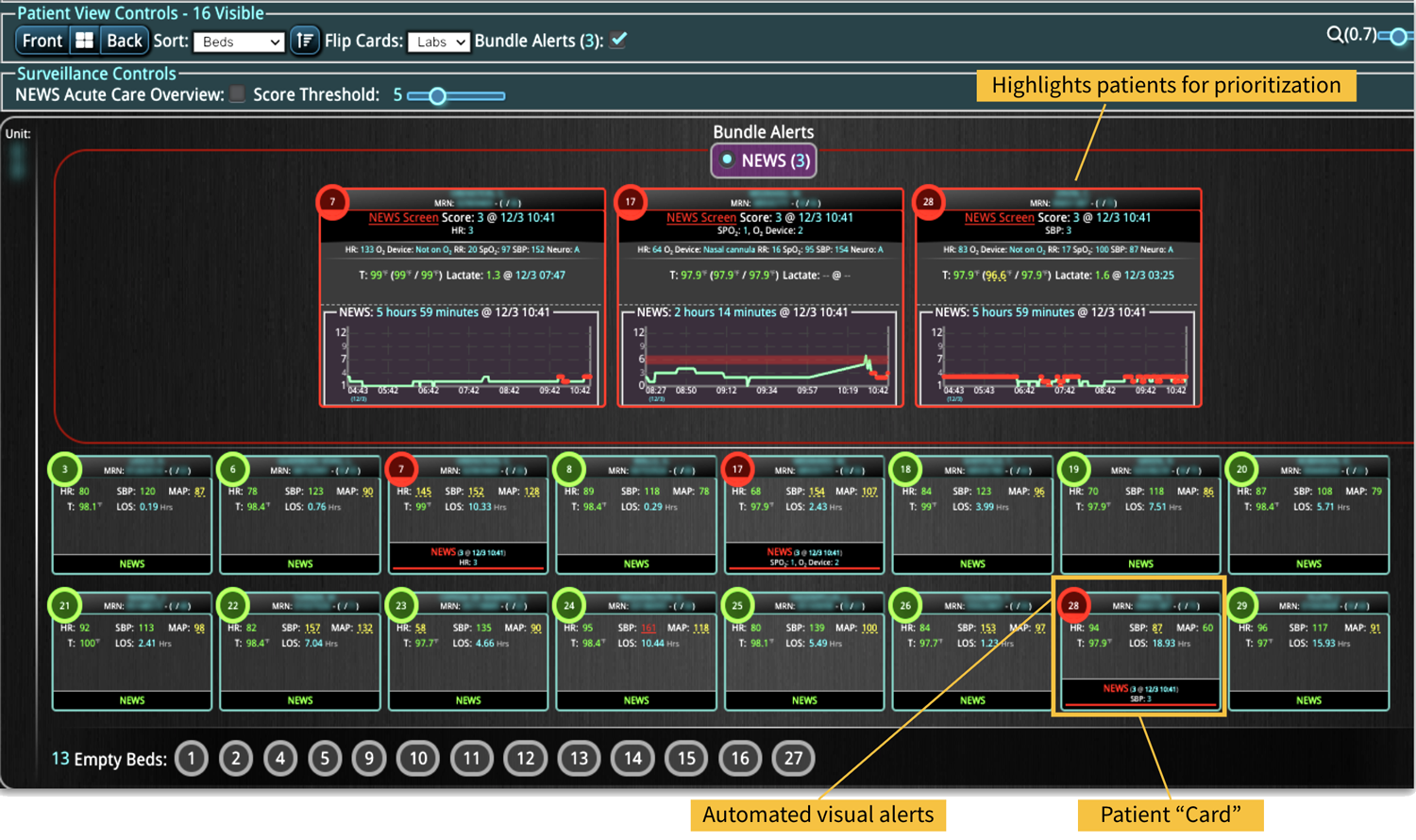
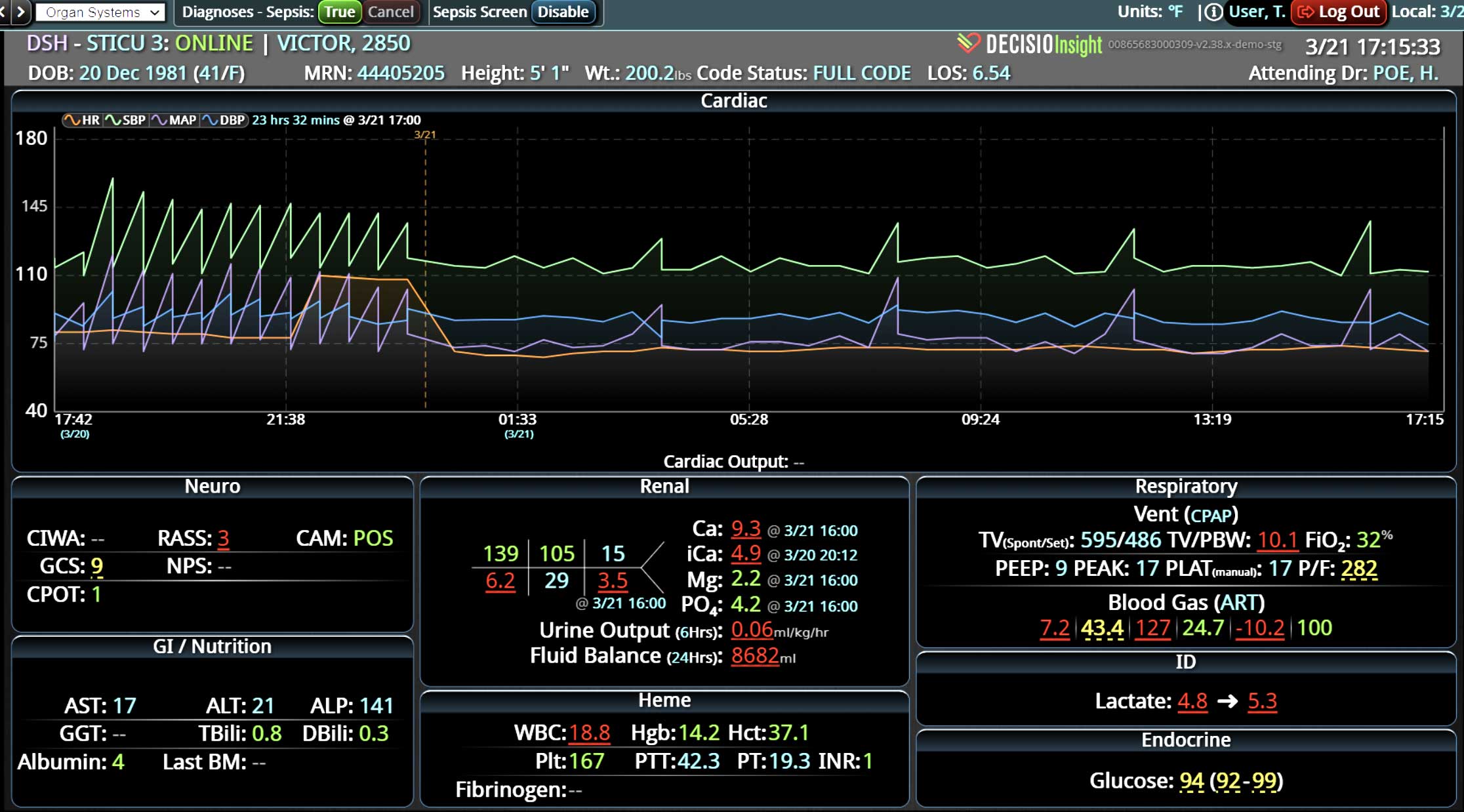
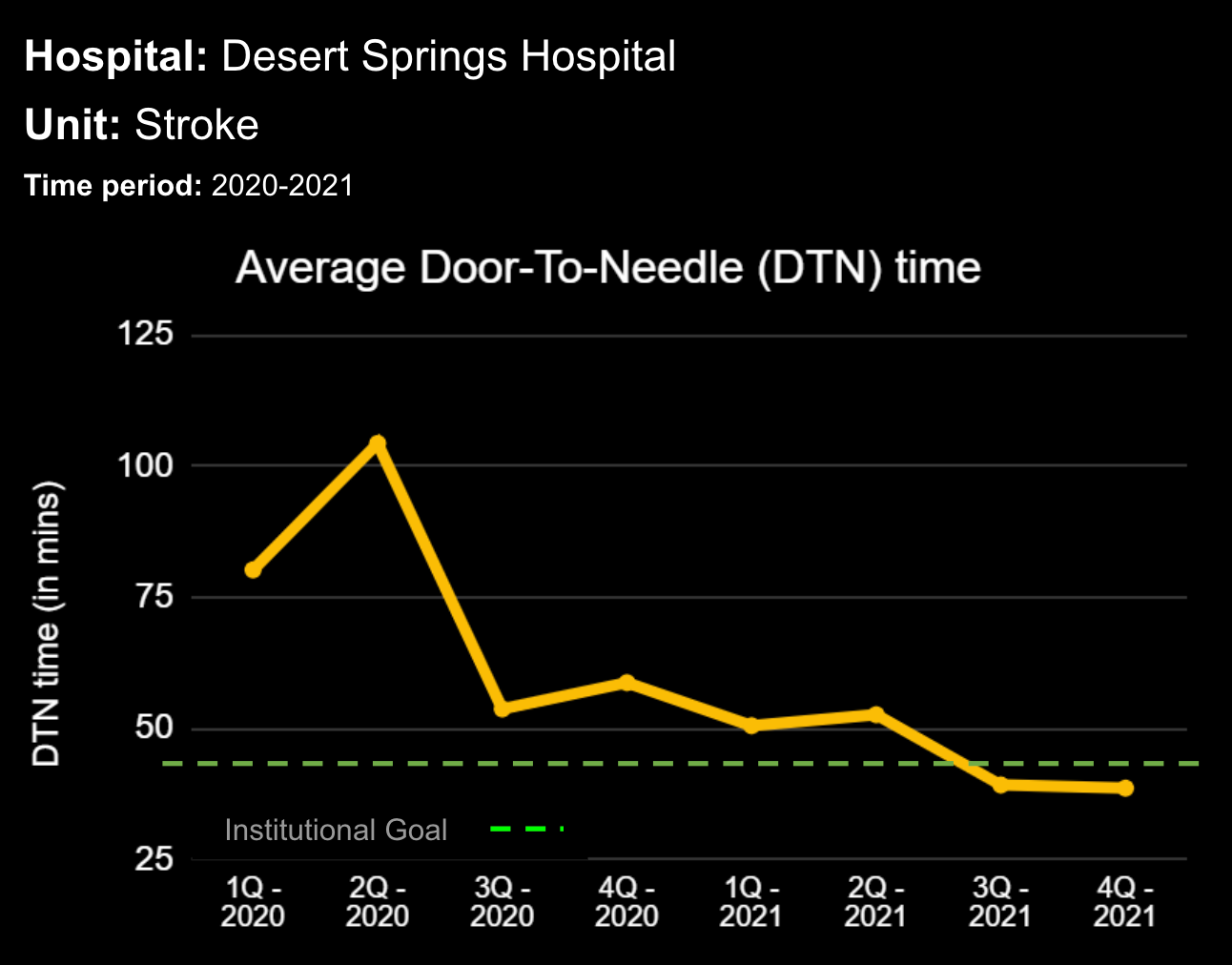
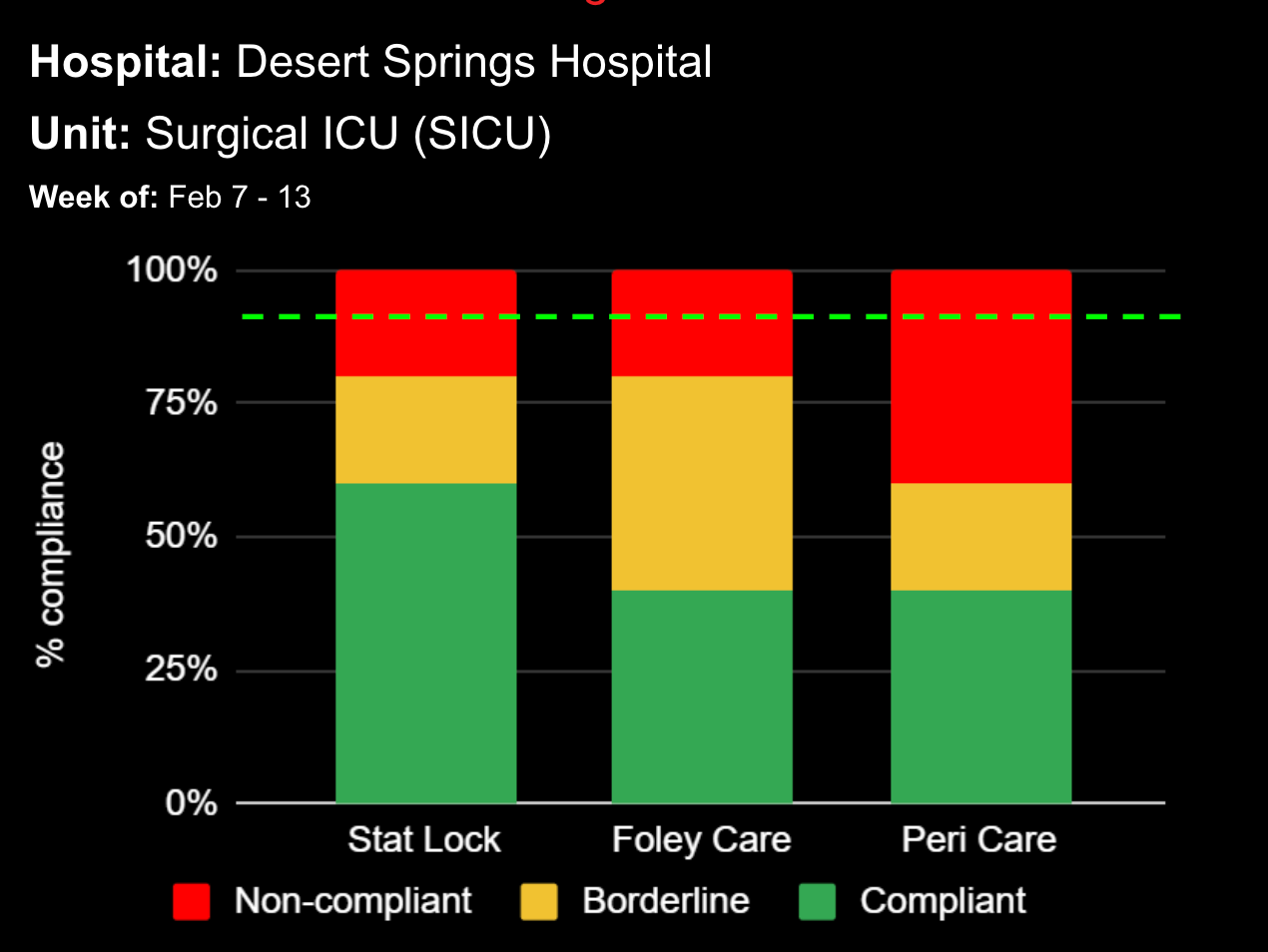
While valuable, just implementing the use of an EWS and the technology is not going to immediately solve failure-to-rescue challenges. A clinical workflow has to be developed around the technology that provides continuous, auto-calculated EWS for patient surveillance along with real-time alerts that avoid creating alert fatigue environments. In a large urban hospital, a rapid response team for critical patients was supplemented with the technology that helped reduce in-hospital mortality by 47%, and the hospital length of stay by 4.7 days.4 When an ED implemented the technology, mortality was reduced by 12% and length of stay decreased by 6.5%.5
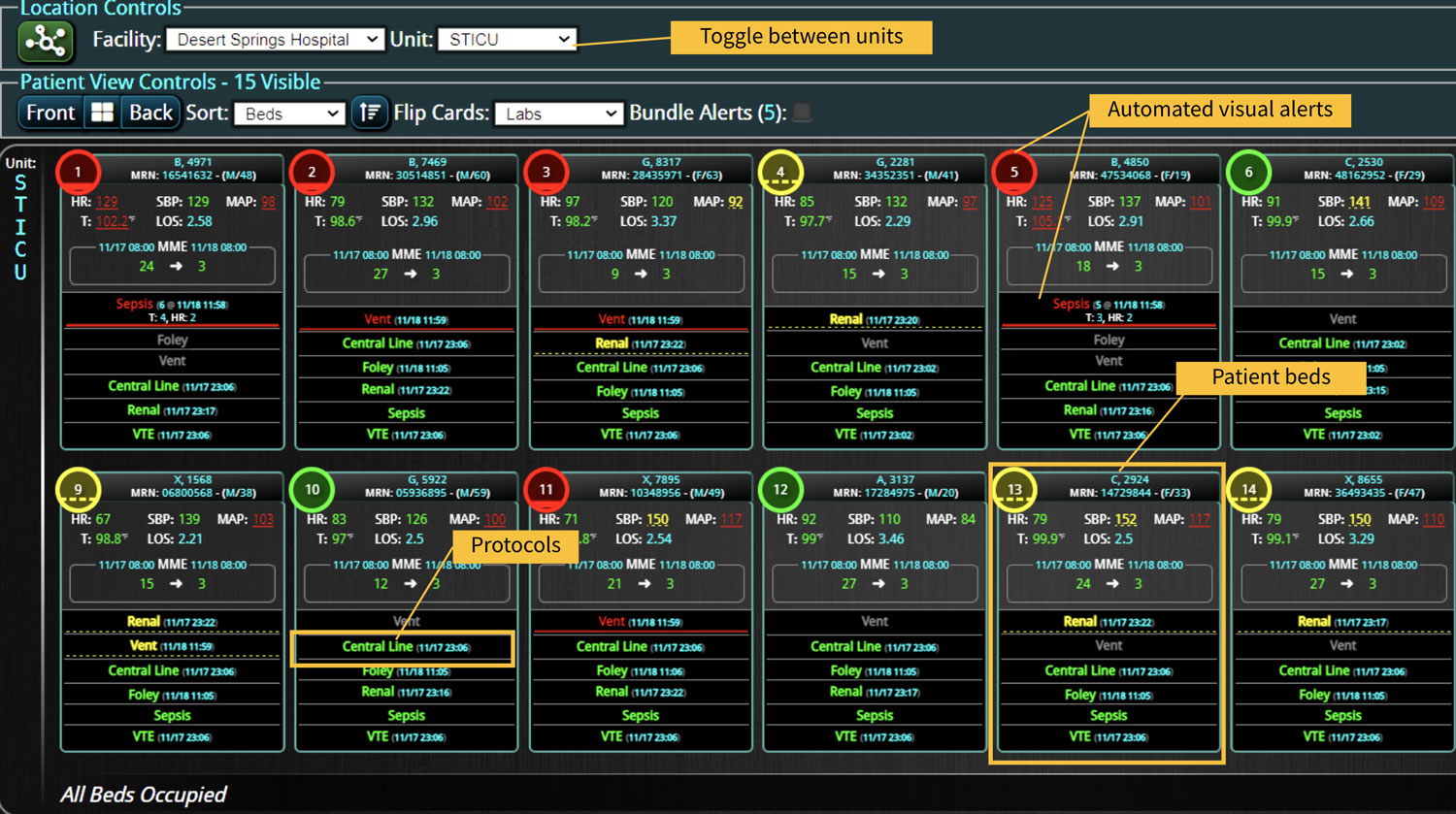
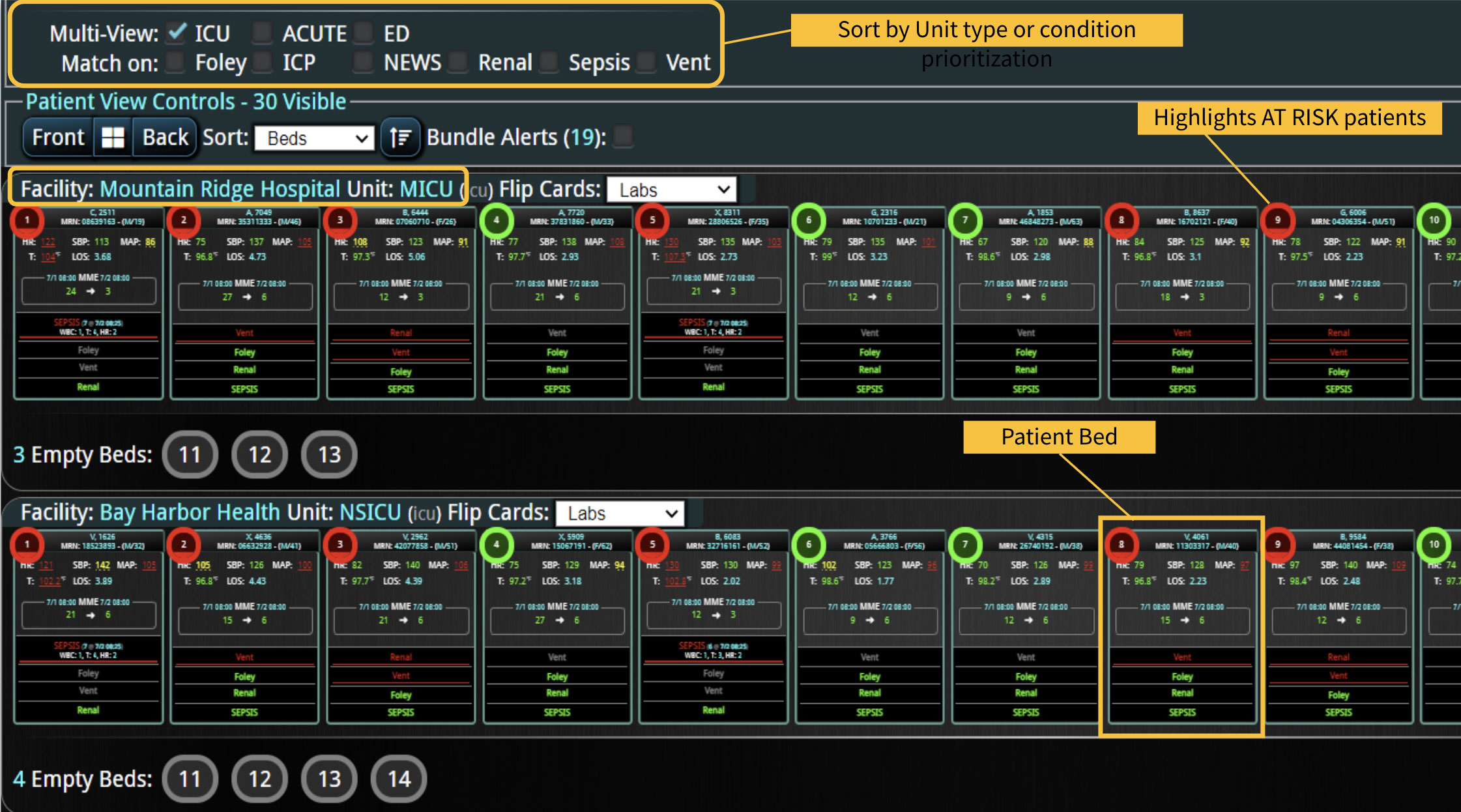
The technology that provides a smart clinical surveillance system must provide a “complete” picture of a patient. Thus, a robust combination of automated data collection and real-time monitoring to include EWS calculations are needed to reduce the clinical burden and create the ideal alert system to improve patient outcomes. Further, cloud-based technology is needed to enable improved remote monitoring and communication among teams. Technology that improves patient monitoring will improve patient safety, thus, the ideal system must continuously triage patients of a department or hospital, so that teams can respond to critical patients in an expedient manner.
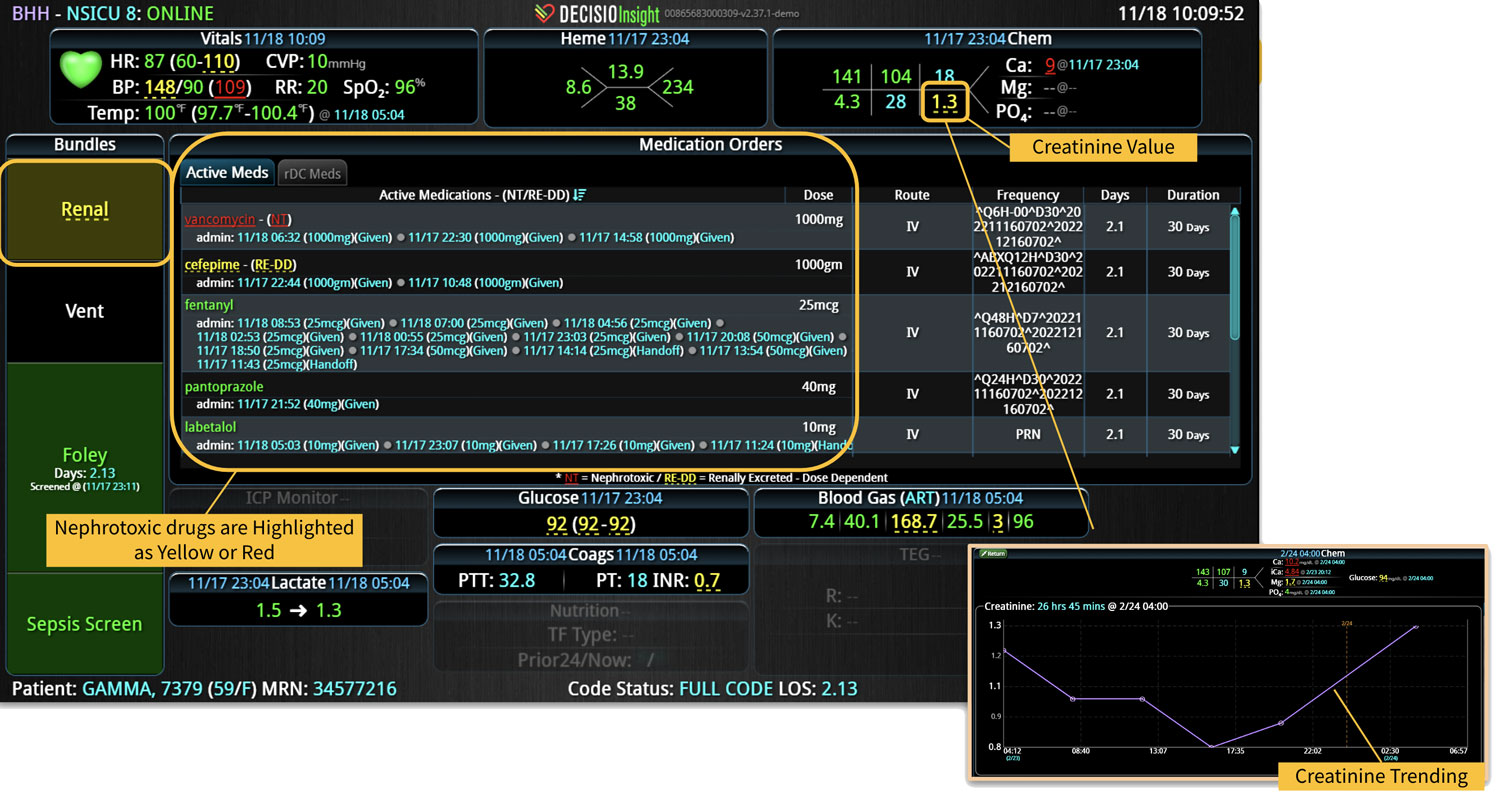
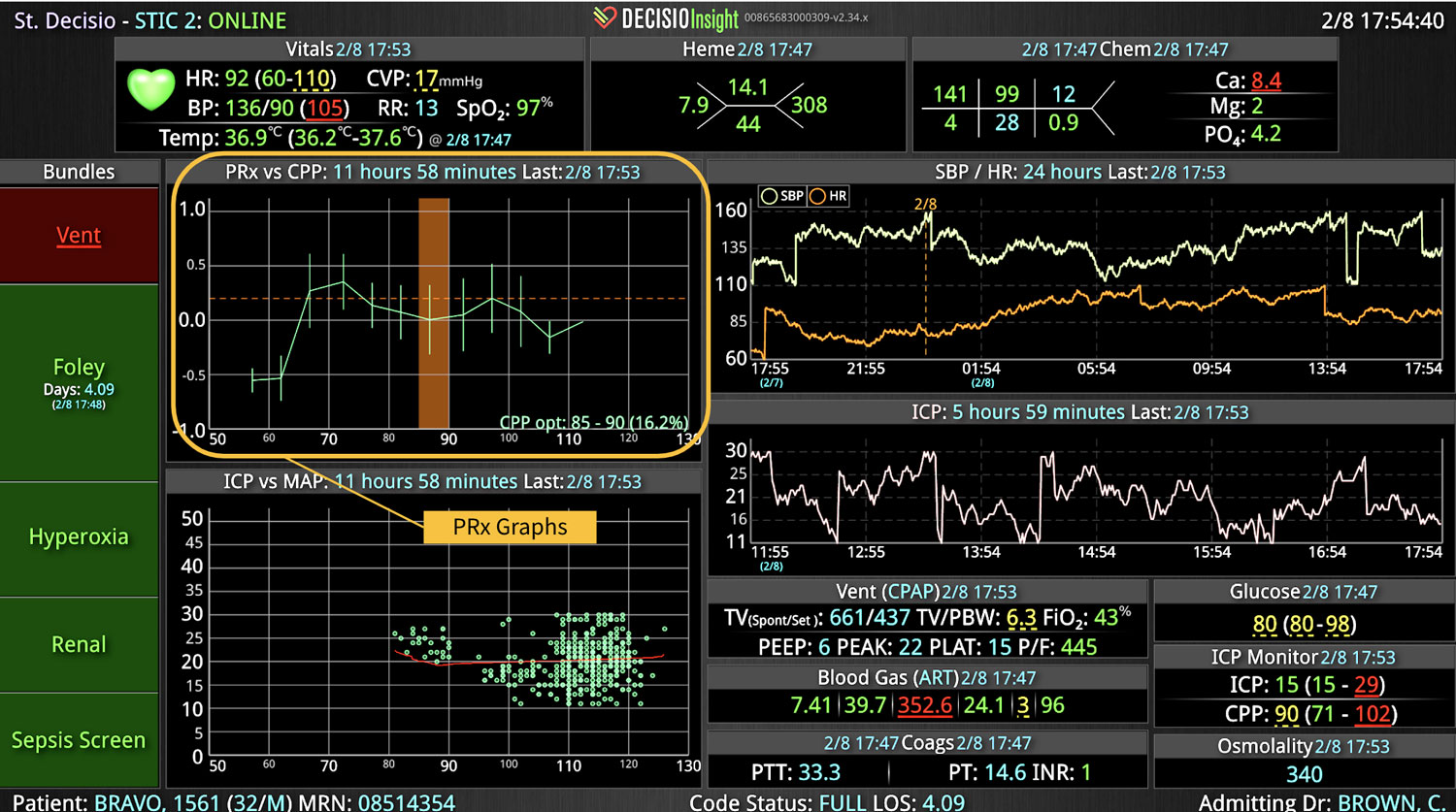
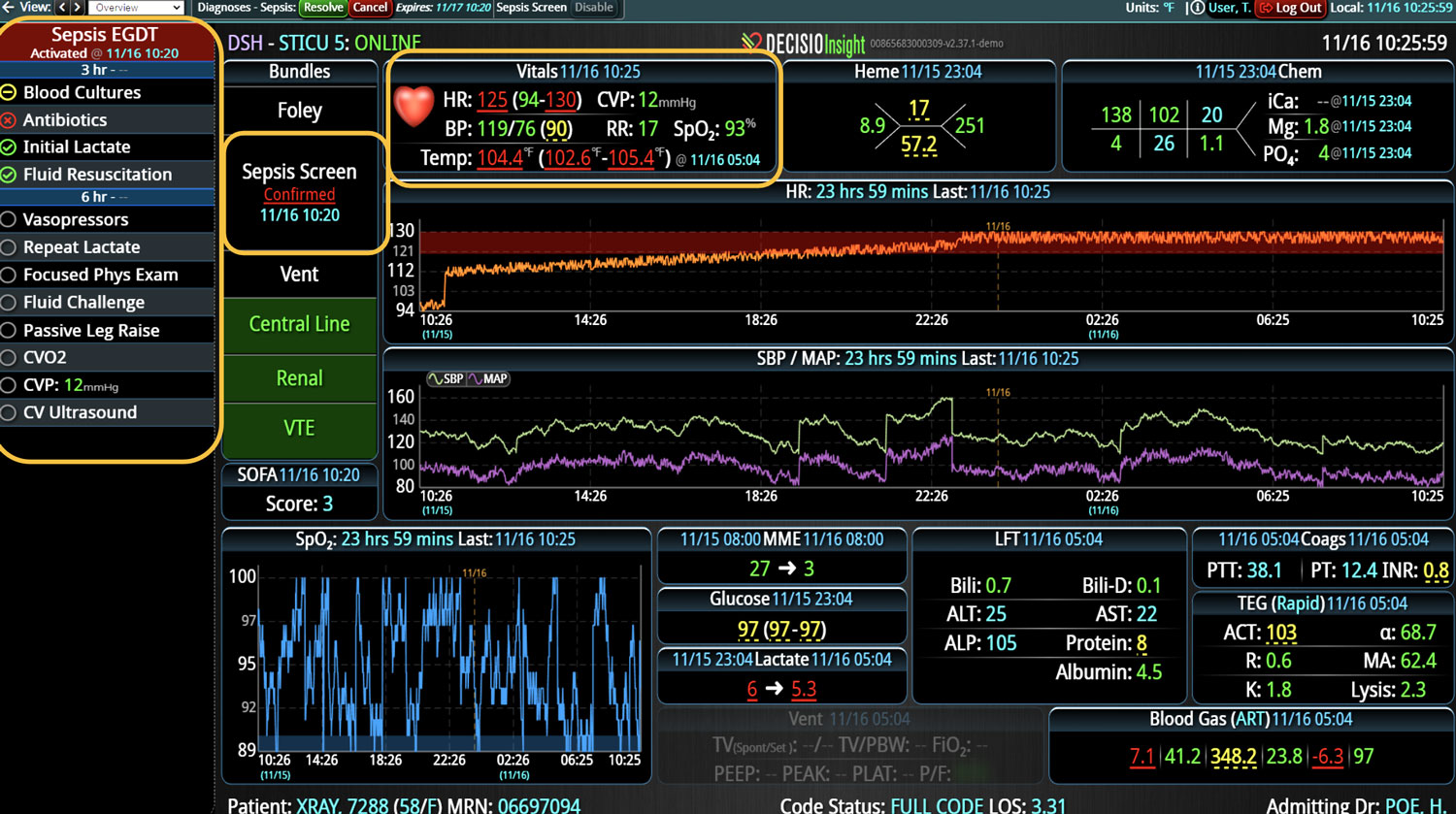
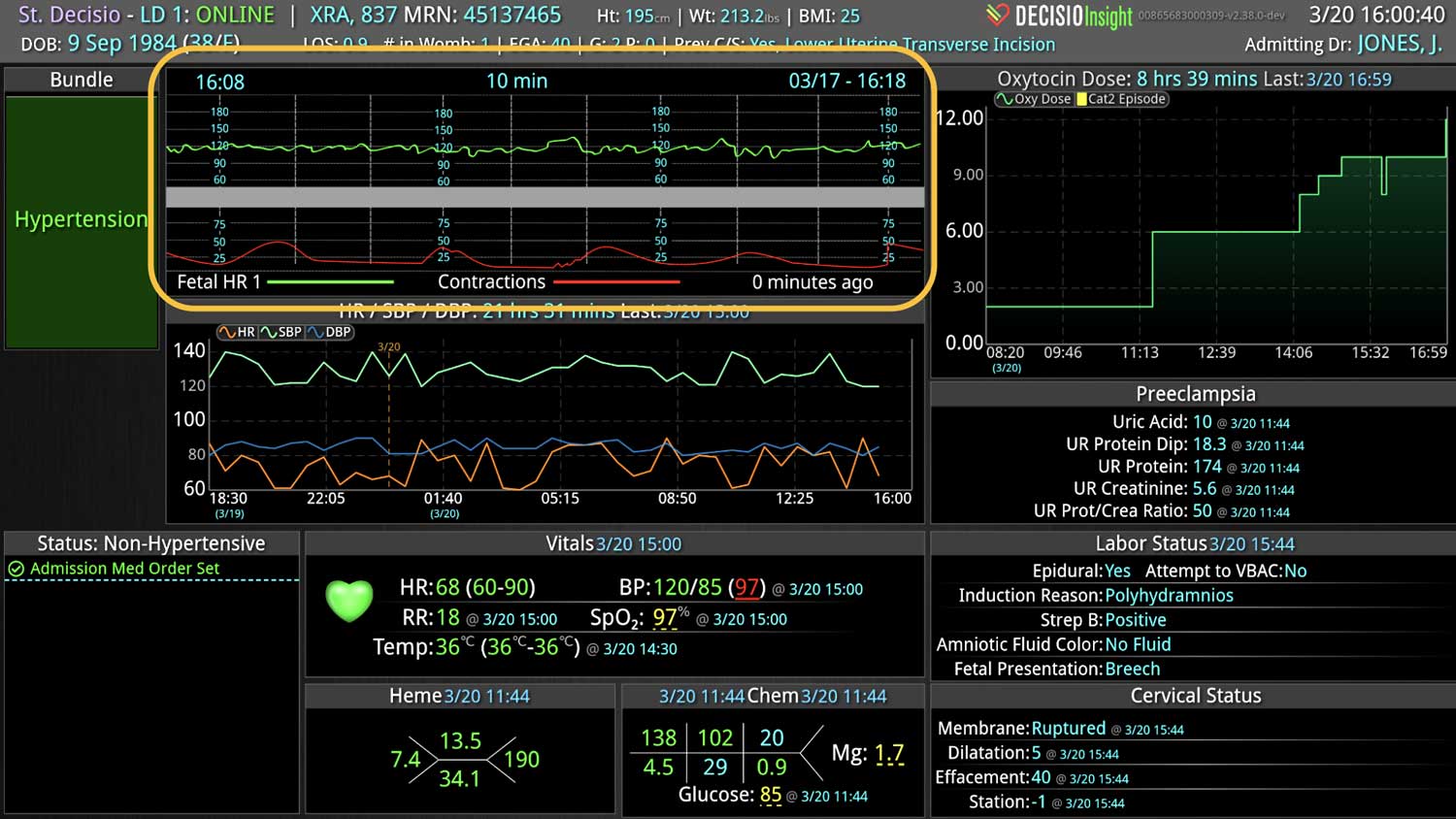
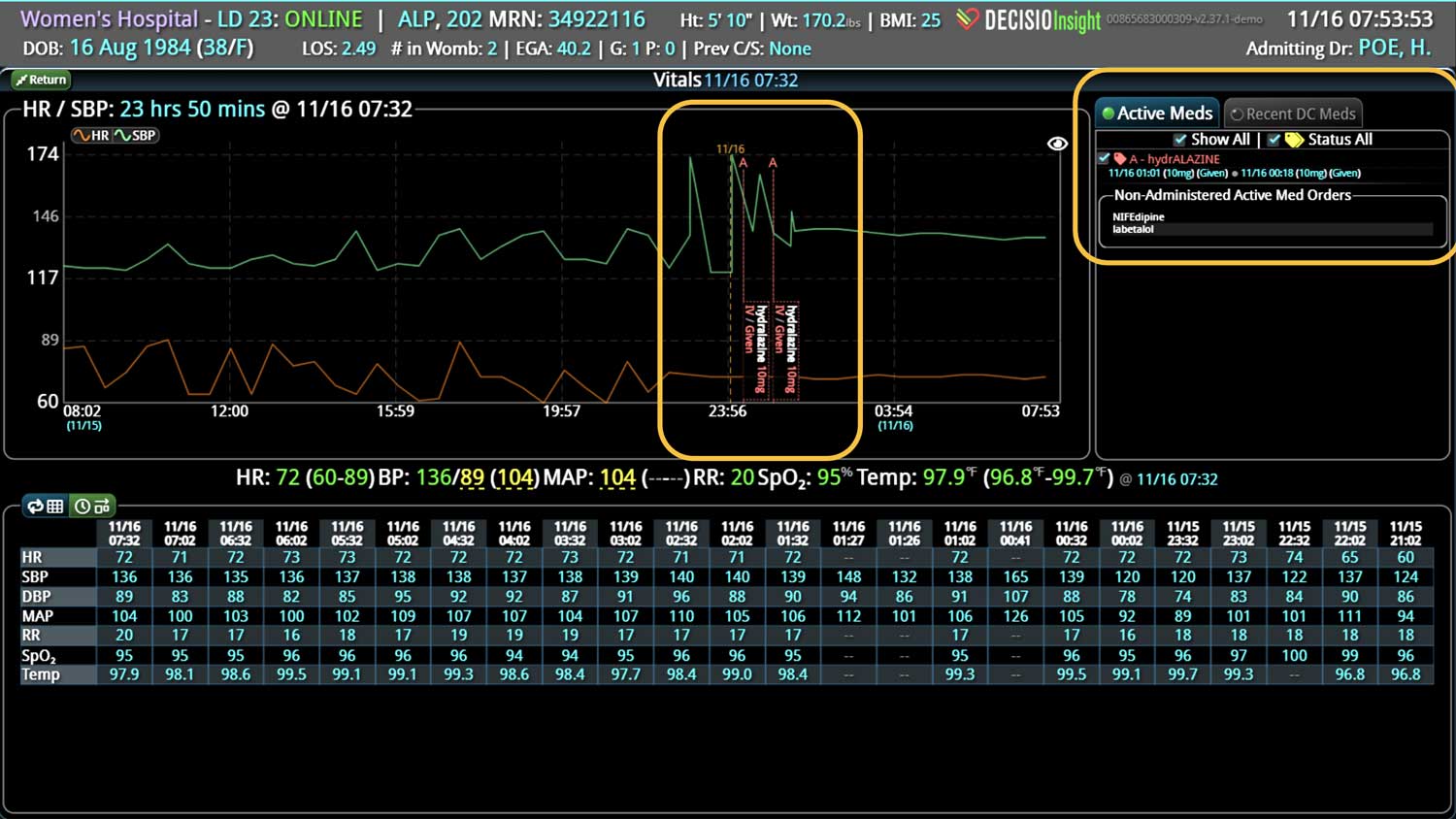
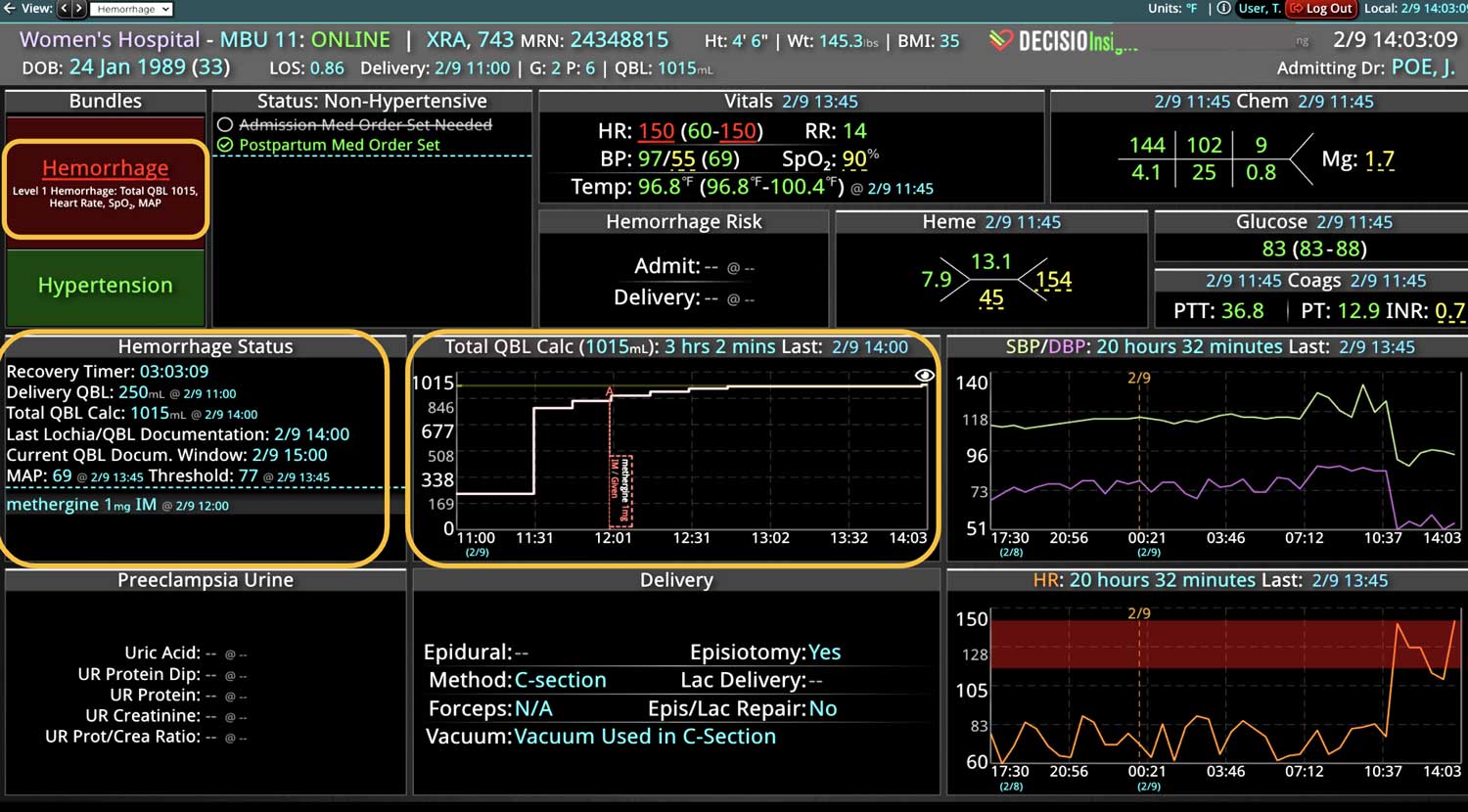
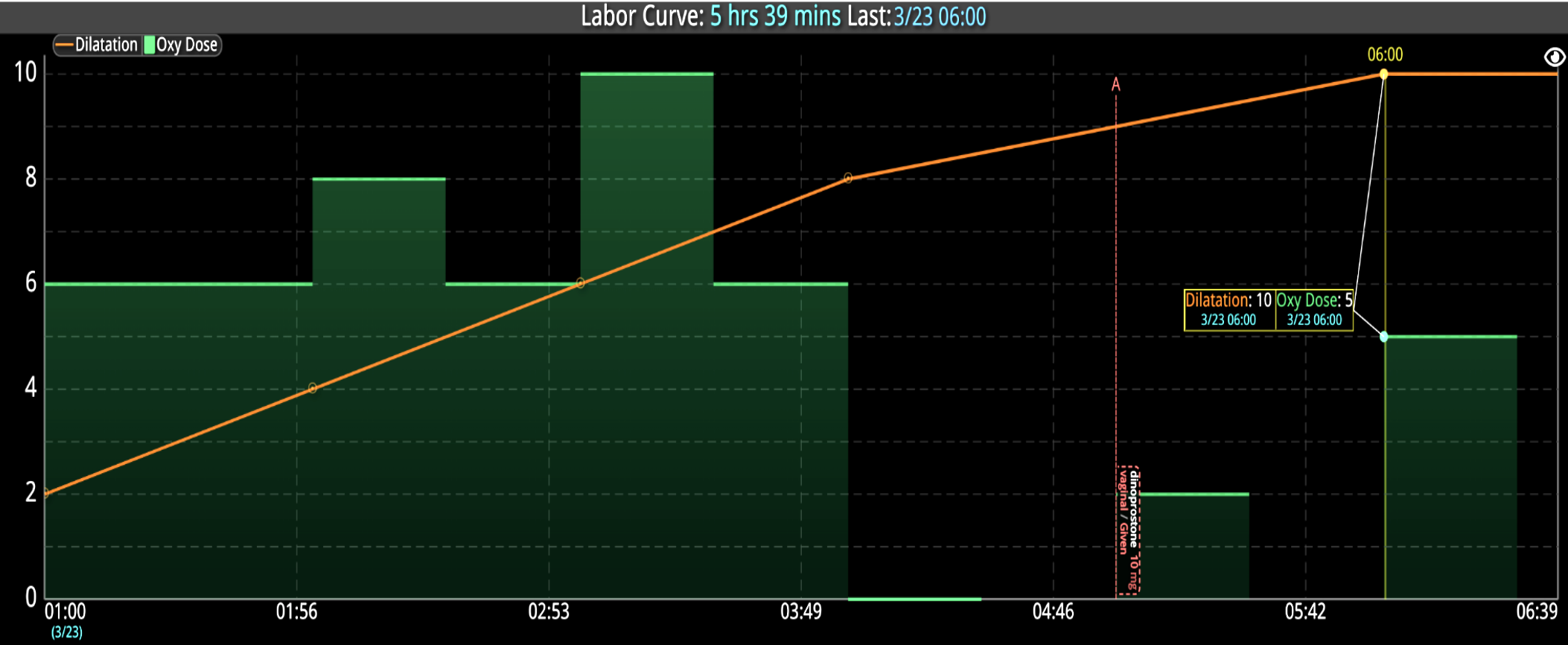
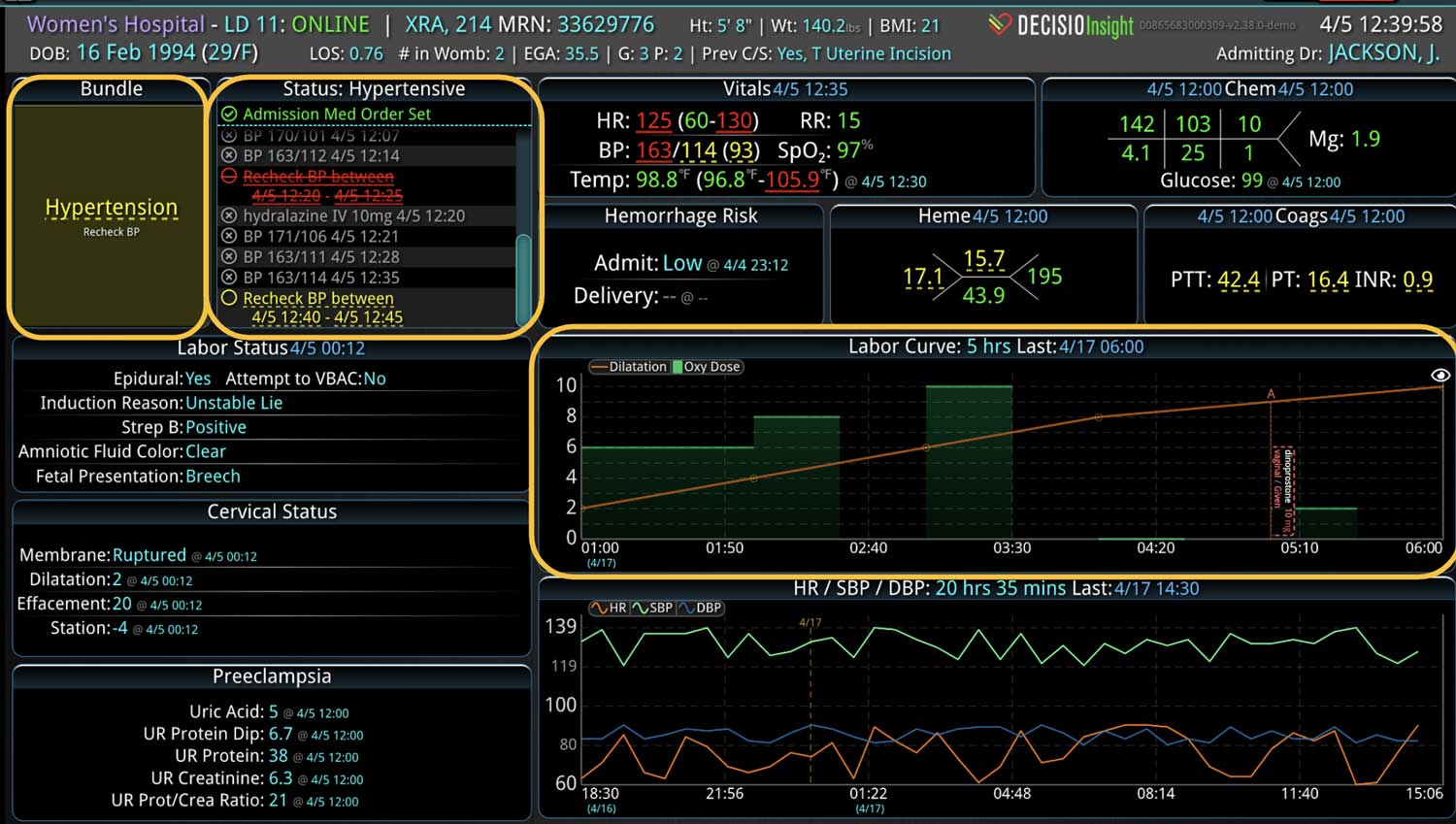
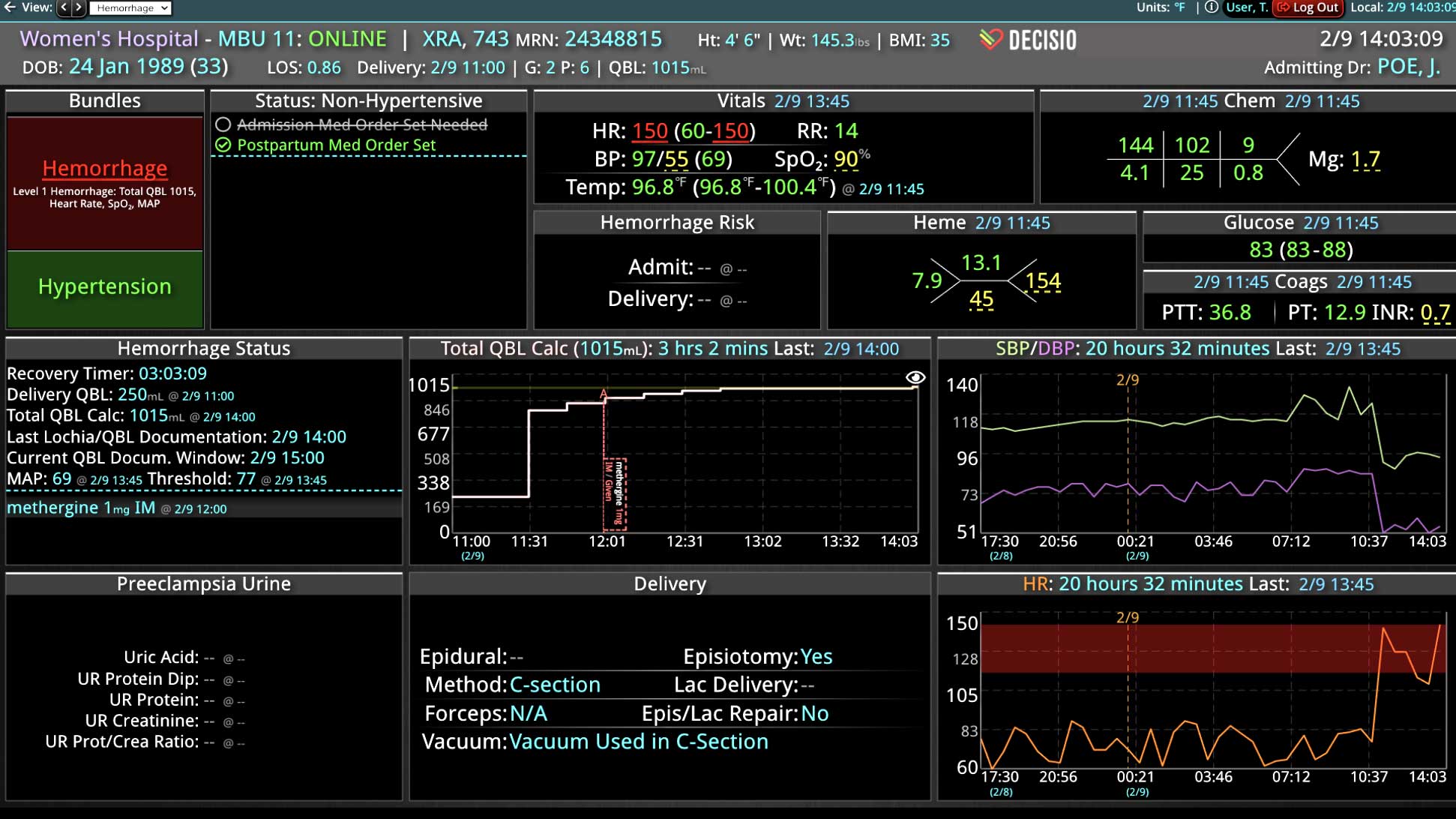
If you or your hospital is interested in implementing a smart clinical surveillance system that incorporates EWSs, consider the InsightIQ platform. InsightIQ is an FDA-cleared, web-native software that uses continuous, smart bedside monitoring that empowers clinical teams to identify at-risk patients and efficiently comply with established clinical guidelines. InsightIQ is a product of DECISIO, a company that applies smart bioanalytics to design software solutions for clinical challenges.
DECISIO is a Texas-based company with deep expertise in the health care industry and information technology. Our software experts work alongside clinicians and administrators to develop unique programs to incorporate EWS calculations that quickly alert teams.
Learn more about InsightIQ and DECISIO’s suite of products at: https://www.decisiohealth.com
References
1. McGaughey J, Alderdice F, Fowler R, et al. Outreach and Early Warning Systems (EWS) for the prevention of intensive care admission and death of critically ill adult patients on general hospital wards. Cochrane Database Syst Rev. 2007;(3):CD005529. doi: 10.1002/14651858.CD005529.pub2
2. Smith MEB, Chiovaro JC, O’Neil M, et al. Early Warning System Scores: A Systematic Review [Internet]. Washington (DC): Department of Veterans Affairs (US); 2014 Jan. Available from: https://ncbi.nlm.nih.gov/books/NBK259029/
3. Royal College of Physicians. National Early Warning Score (NEWS): Standardising the assessment of acute-illness severity in the NHS. Report of a working party. London: RCP, 2012. Available from: https://www.rcplondon.ac.uk/file/32/download
4. Morgan CK, Amspoker AB, Howard C. Continuous Cloud-Based Early Warning Score Surveillance to Improve the Safety of Acutely Ill Hospitalized Patients. J Healthcare Qual. 2021;43(1):59-66. doi: 10.1097/JHQ.0000000000000272
5. Howard C, Amspoker AB, Morgan CK, et al. Implementation of automated early warning decision support to detect acute decompensation in the emergency department improves hospital mortality. BMJ Open Qual. 2022;11(2):e001653. doi: 10.1136/bmjoq-2021-001653
Learn more About How we help clinicians improve patient outcomes
Schedule a call with our team to discuss how we are helping our clients revolutionize how clinicians manage patient interventions.