22 Jul Five Steps to Address Failure to Rescue

Five Steps to Address Failure to Rescue
You may have heard of the term failure to rescue or the abbreviation FTR when discussing patient outcomes. Traditionally, FTR is defined as unexpected deterioration of a patient or death due to a complication. The complication could be due to an underlying illness or related to medical care. Both hospitals and physicians recognize FTR as an urgent problem with numerous and multifaceted contributing factors. A patient’s poor outcome due to FTR could be related to any of the following challenges:
- Inadequate or inconsistent method of collecting vital signs data
- Failure to recognize and respond rapidly to abnormal vital signs
- Delays in timely escalation of care for patients showing signs of clinical deterioration
Many hospitals manually collect vital signs, where data is entered by a health care professional into the patient’s electronic health record (EHR) every 4 to 12 hours. This approach represents single data points in time but does not reflect what happens during time intervals between data captures. During these undocumented intervals, patients may rapidly or subtly deteriorate. By the time clinicians become aware of this decline, the complication may be full blown and lead to an FTR episode.
How can a health care organization reduce the number of FTR cases?
1. Automate the Capture of Patient Vitals
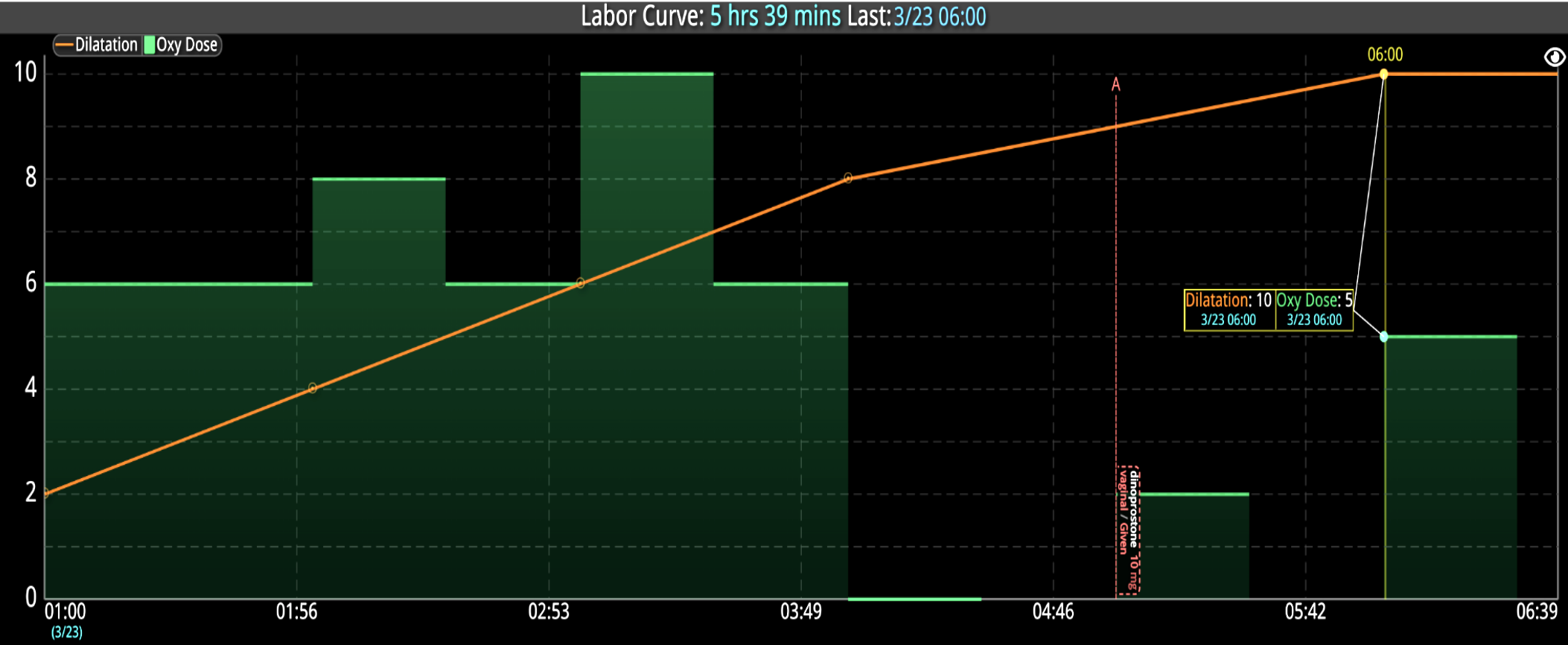
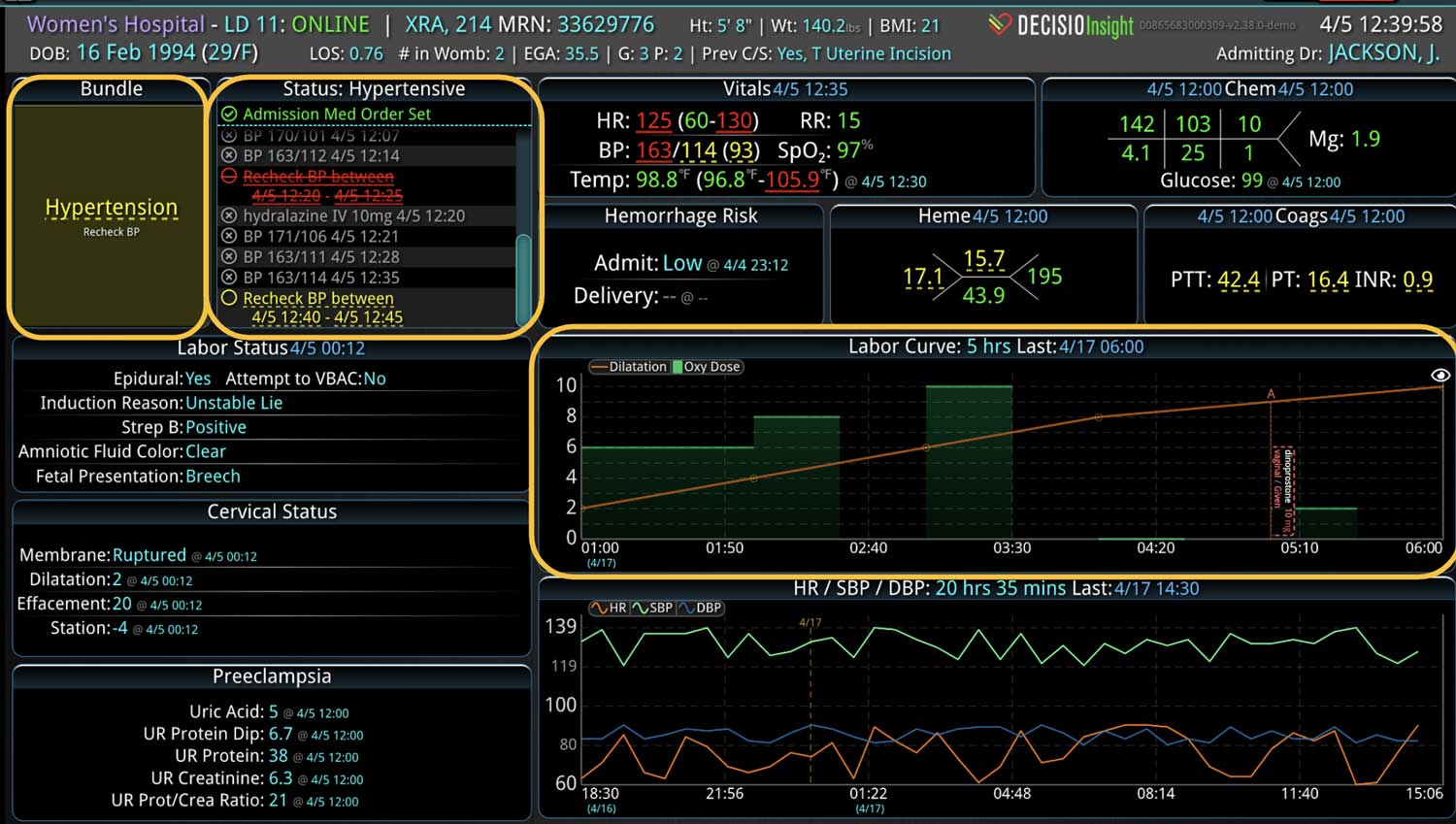
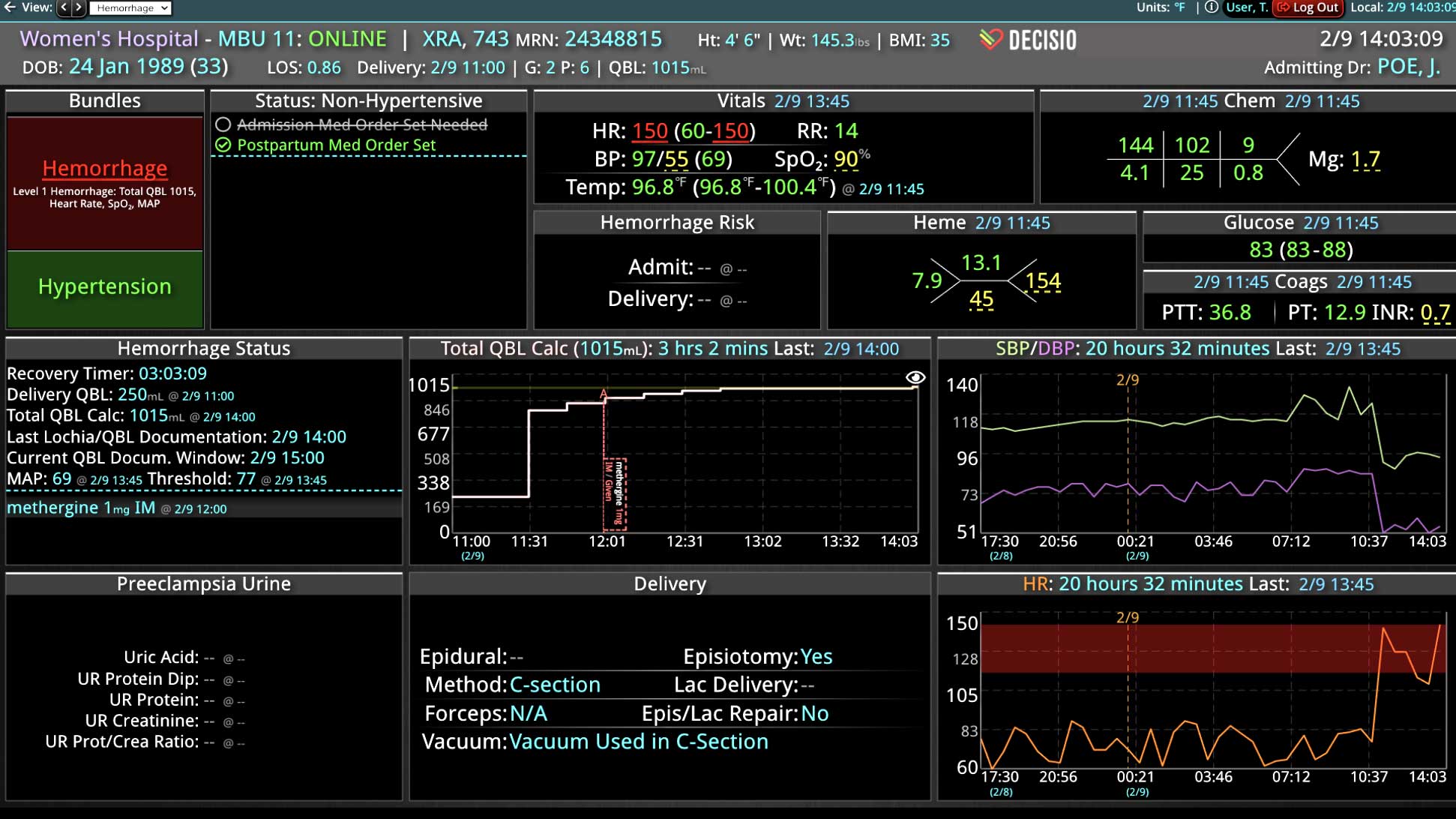
Taking patient vitals is one of the most critical components of quality healthcare, but it can also be one of the most labor-intensive duties that falls upon health care providers. Using automated technology that monitors patients and captures validated vital signs right from the bedside provides tremendous benefits to both patient and clinicians. Automating this process reduces risks of human error associated with the manual entry of patient information into the EHR. Automation efficiently delivers timely, accurate electronic vital signs data and clinical observations, delivering actionable insights and providing clinicians more time with patients.
This type of enhanced vitals monitoring provides continuous data, which enables a more detailed monitoring report for the health care team. Real-time data logging enables providers to build a comprehensive picture of the current patient’s health status. Most importantly, automated monitoring can immediately alert the team when intervention and rapid response are crucial in addressing a patient’s changing health condition.
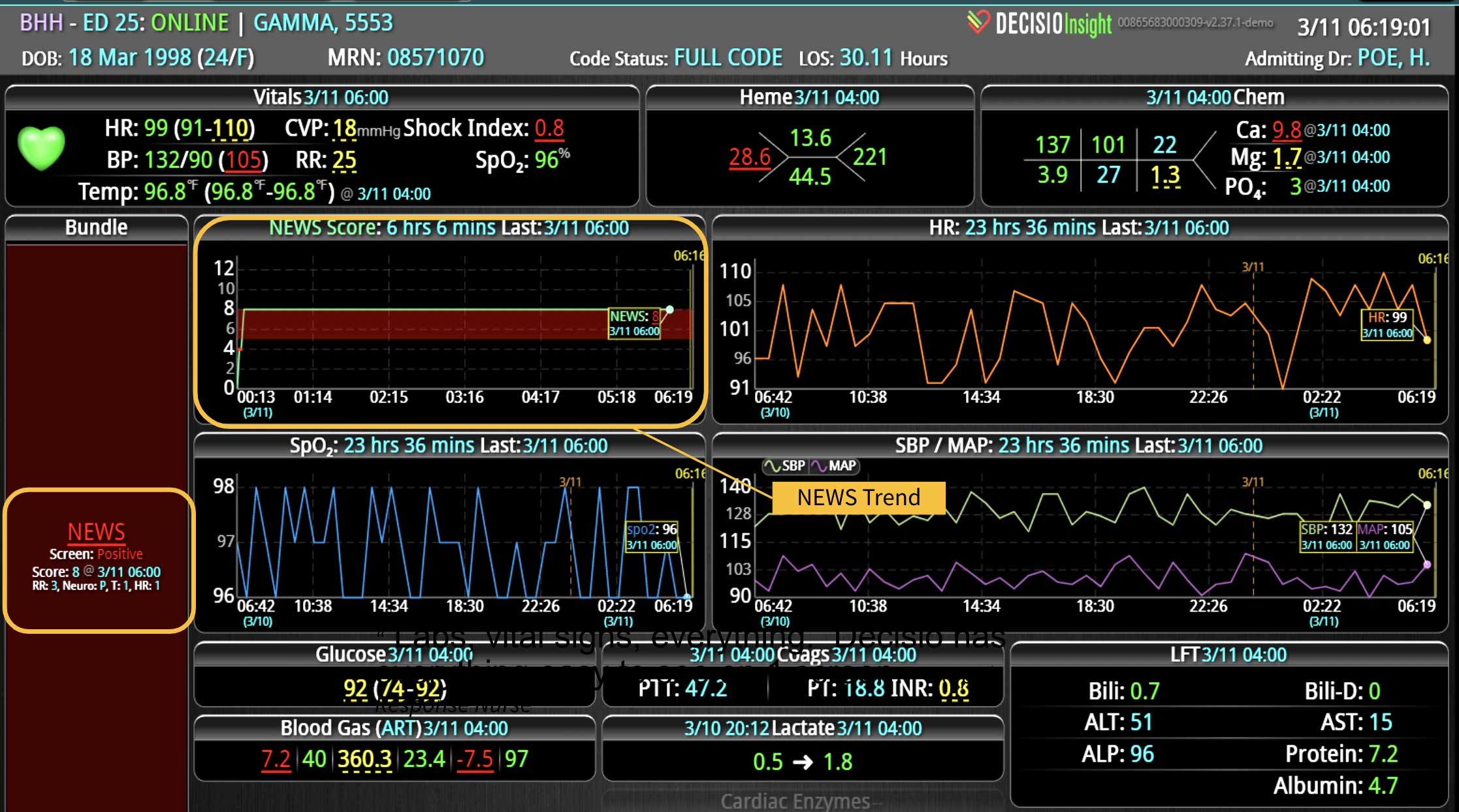
2. Track and Score Early Warning Signs
It is not uncommon for hospitalized patients to exhibit early warning signs before deteriorating. The key to positive clinical outcomes is early recognition of these signs, followed by a provider’s appropriate and timely response.
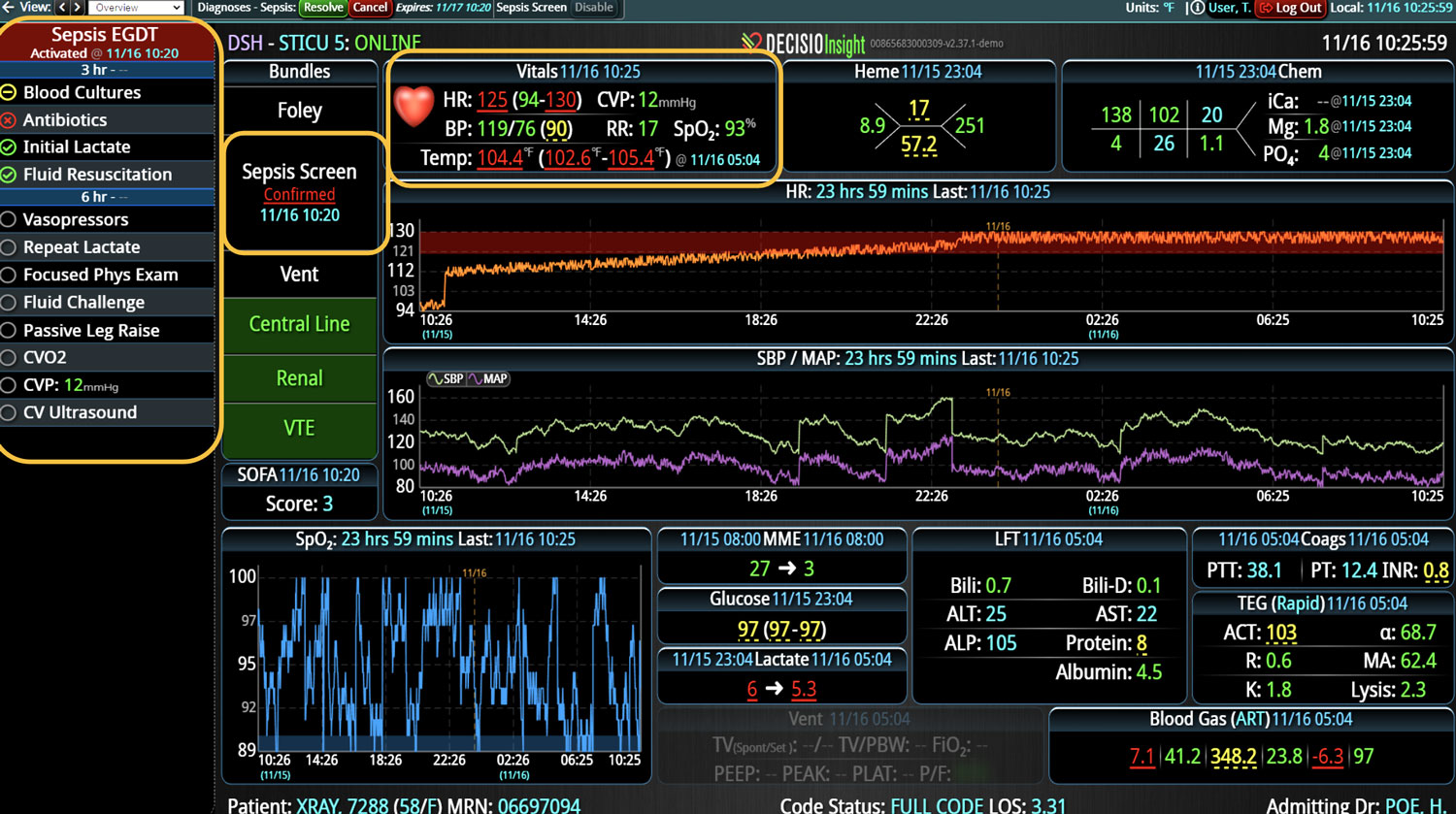
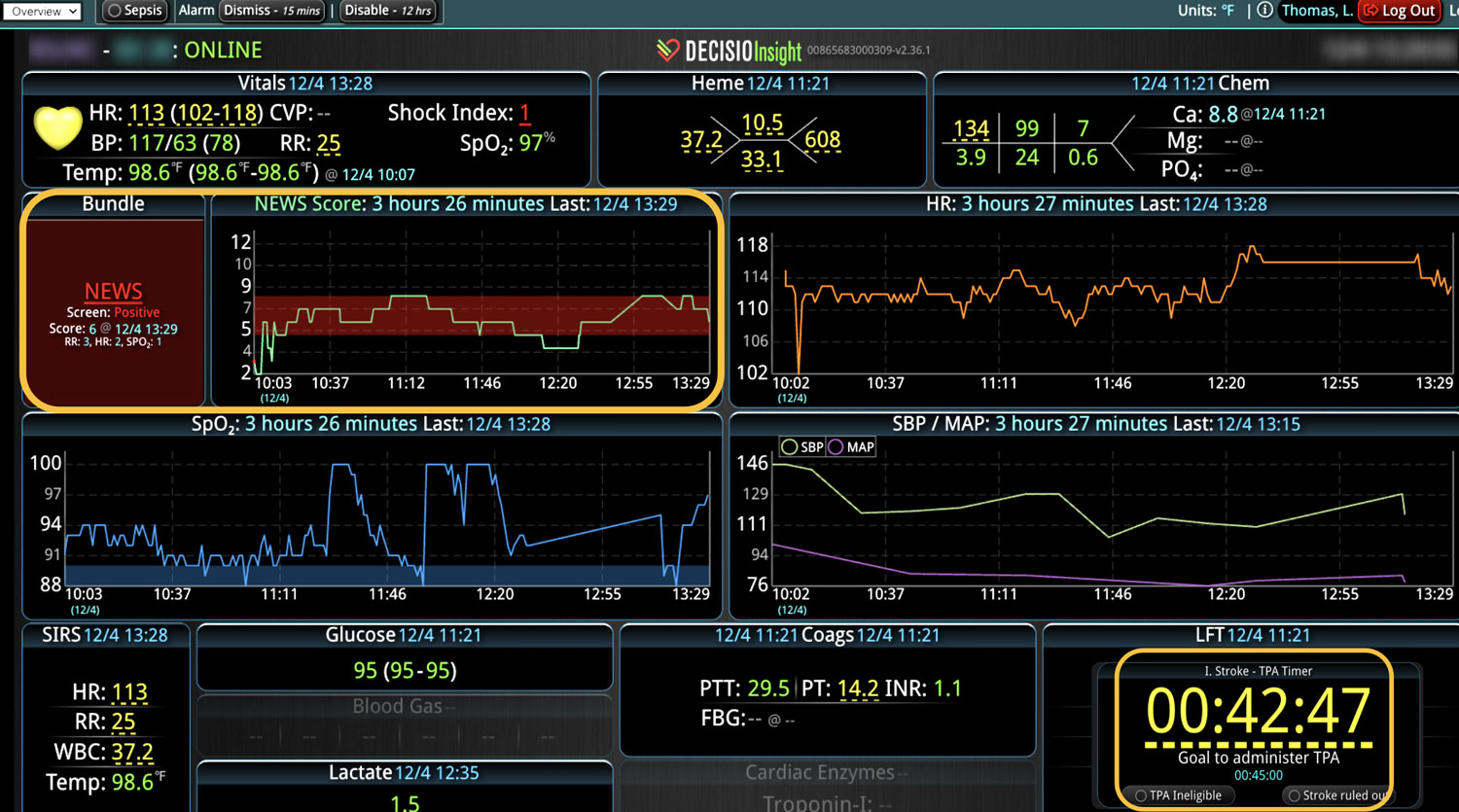
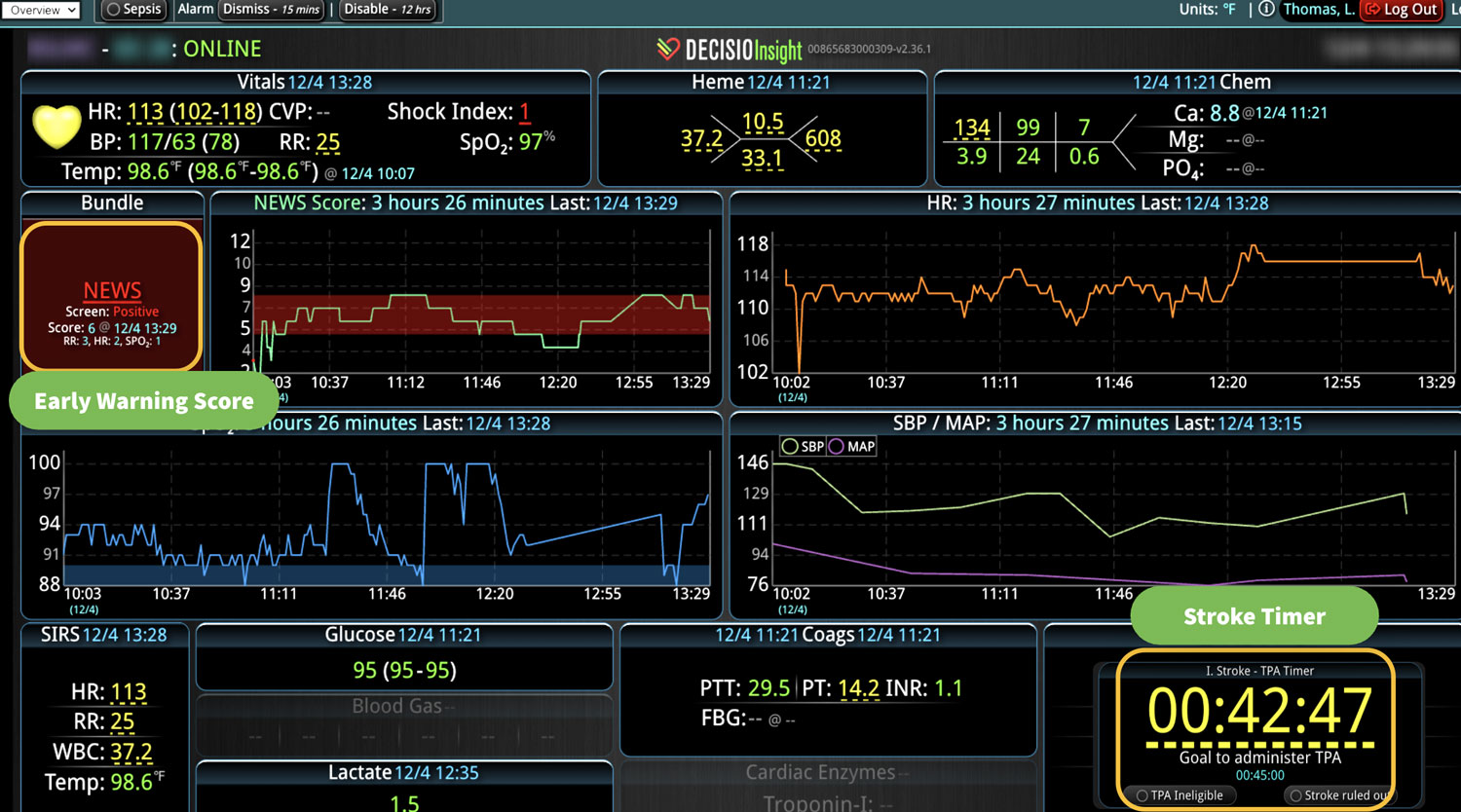
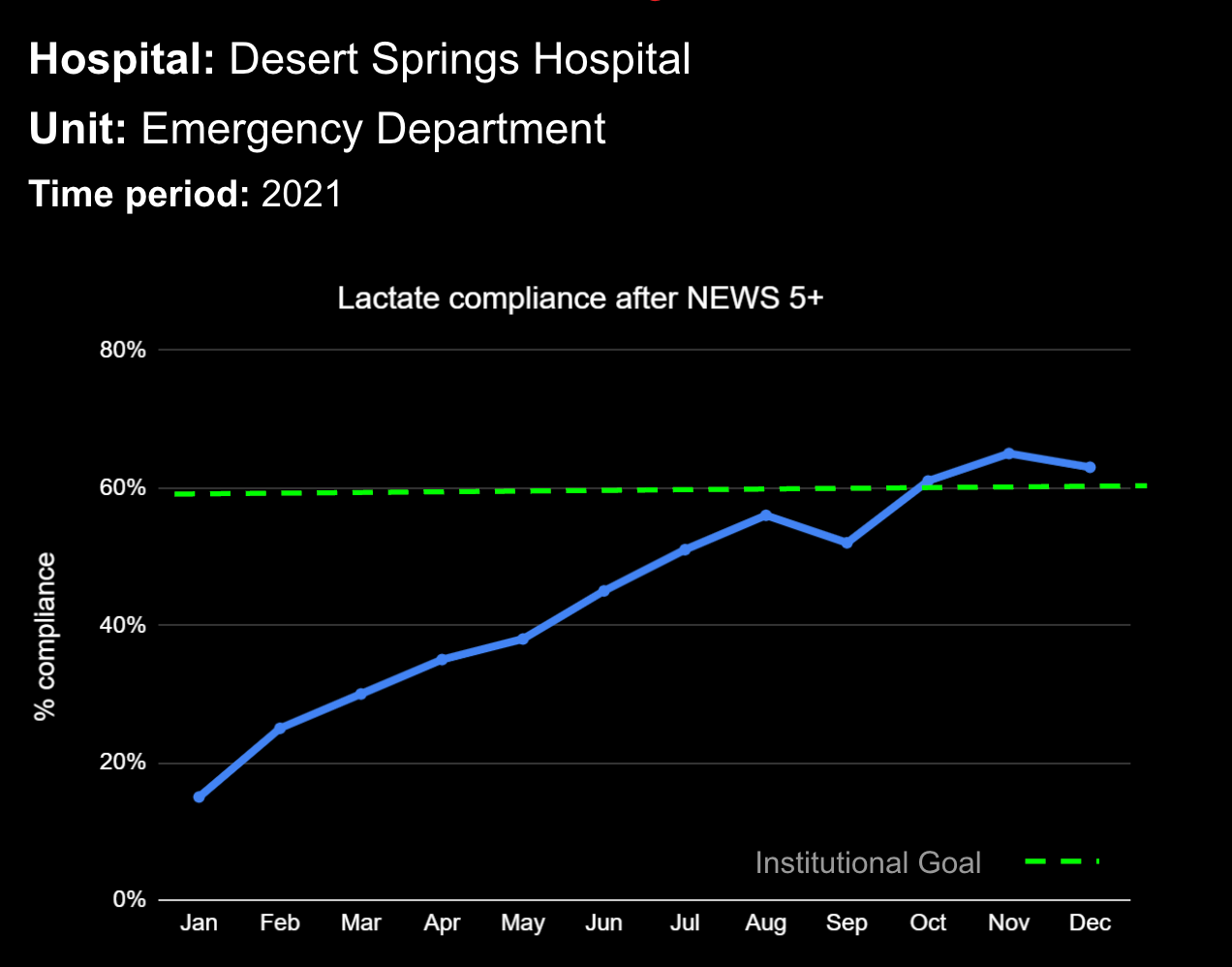
Implementing an early warning scoring system (EWSS) can assist in early intervention, timely transfer to a higher level of care, and prevent emergency code conditions. Early detection of unfavorable changes in a patient’s vital signs can lead to a life-saving difference by alerting providers and allowing the health care team to intervene earlier.1
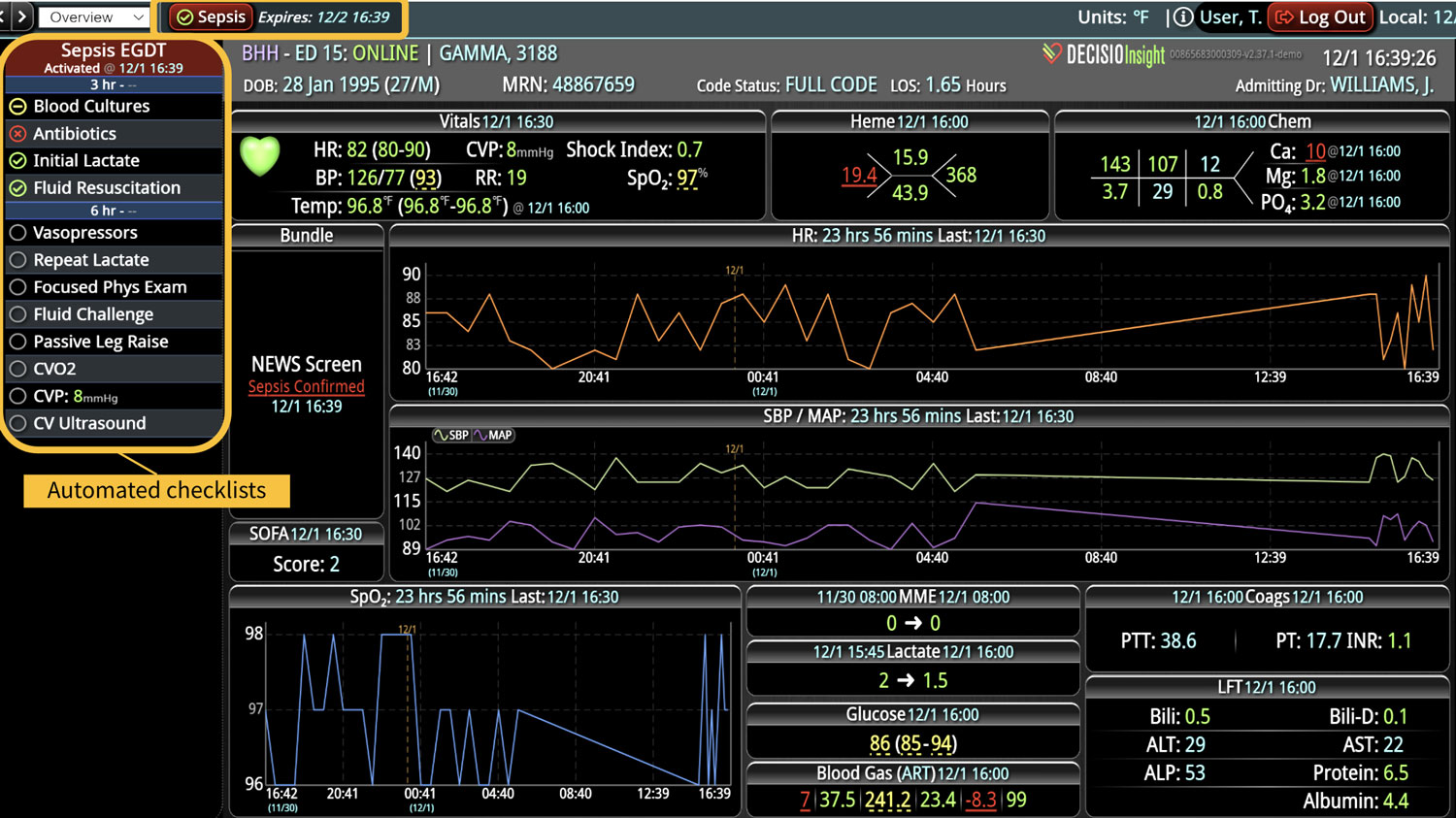
An efficient EWSS must be able to register subtle changes in vital signs and provide an immediate acuity score based on readily available clinical physiologic data, including blood pressure, heart rate, respiratory rate, and temperature. Incorporating an EWSS into automated patient monitoring technology eliminates manual calculations while reducing guesswork and lag time, helping teams respond quickly and appropriately during dire life-threatening situations.
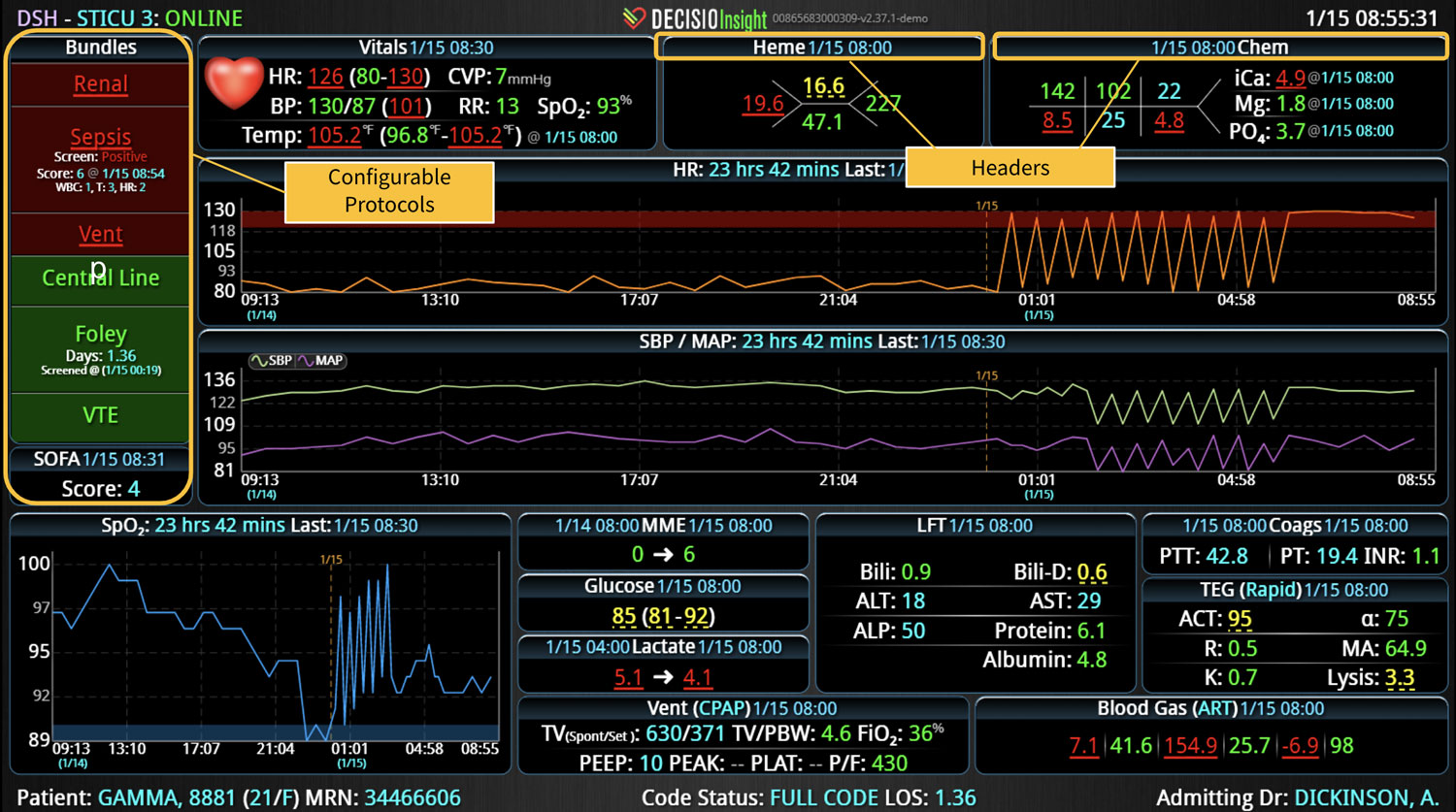
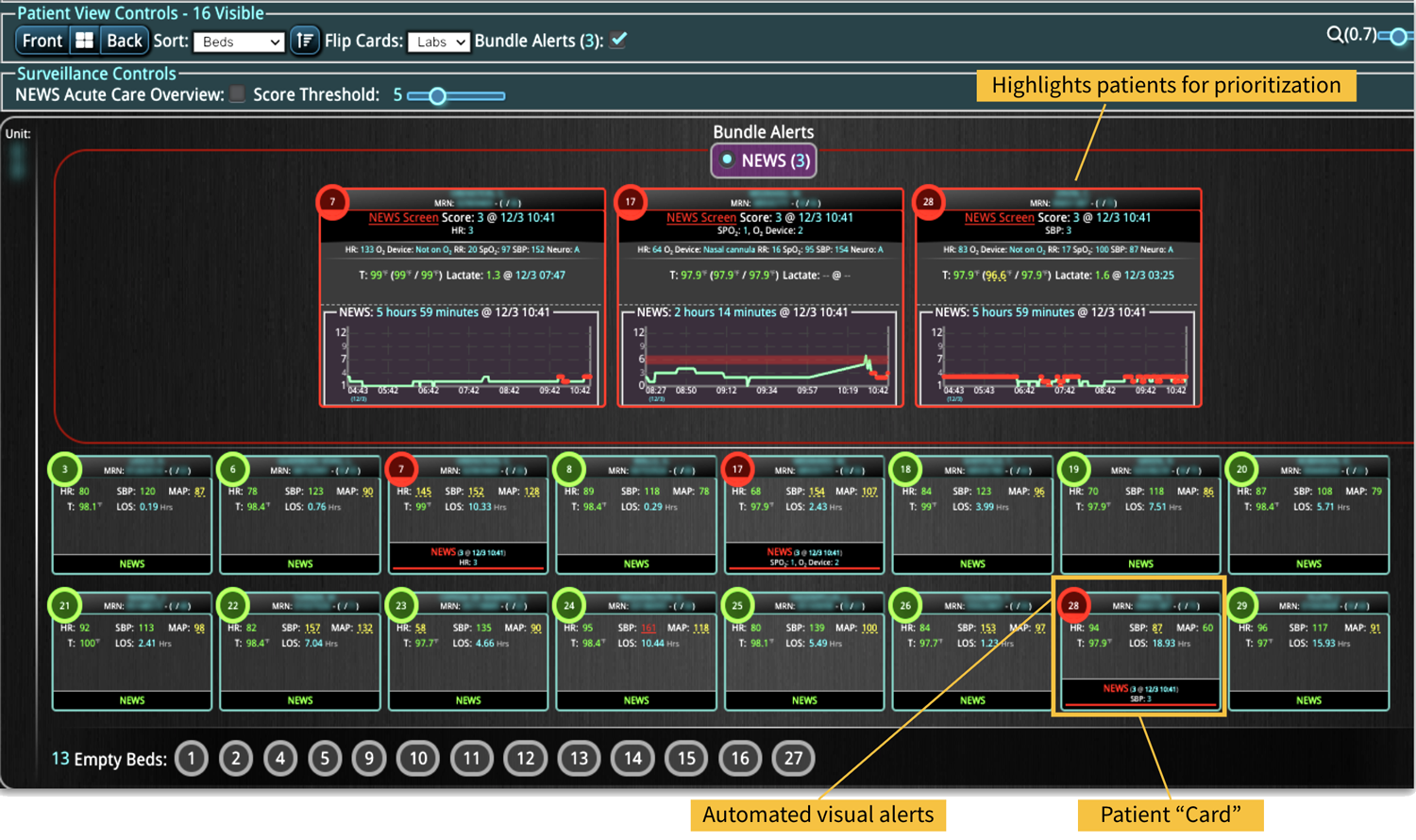
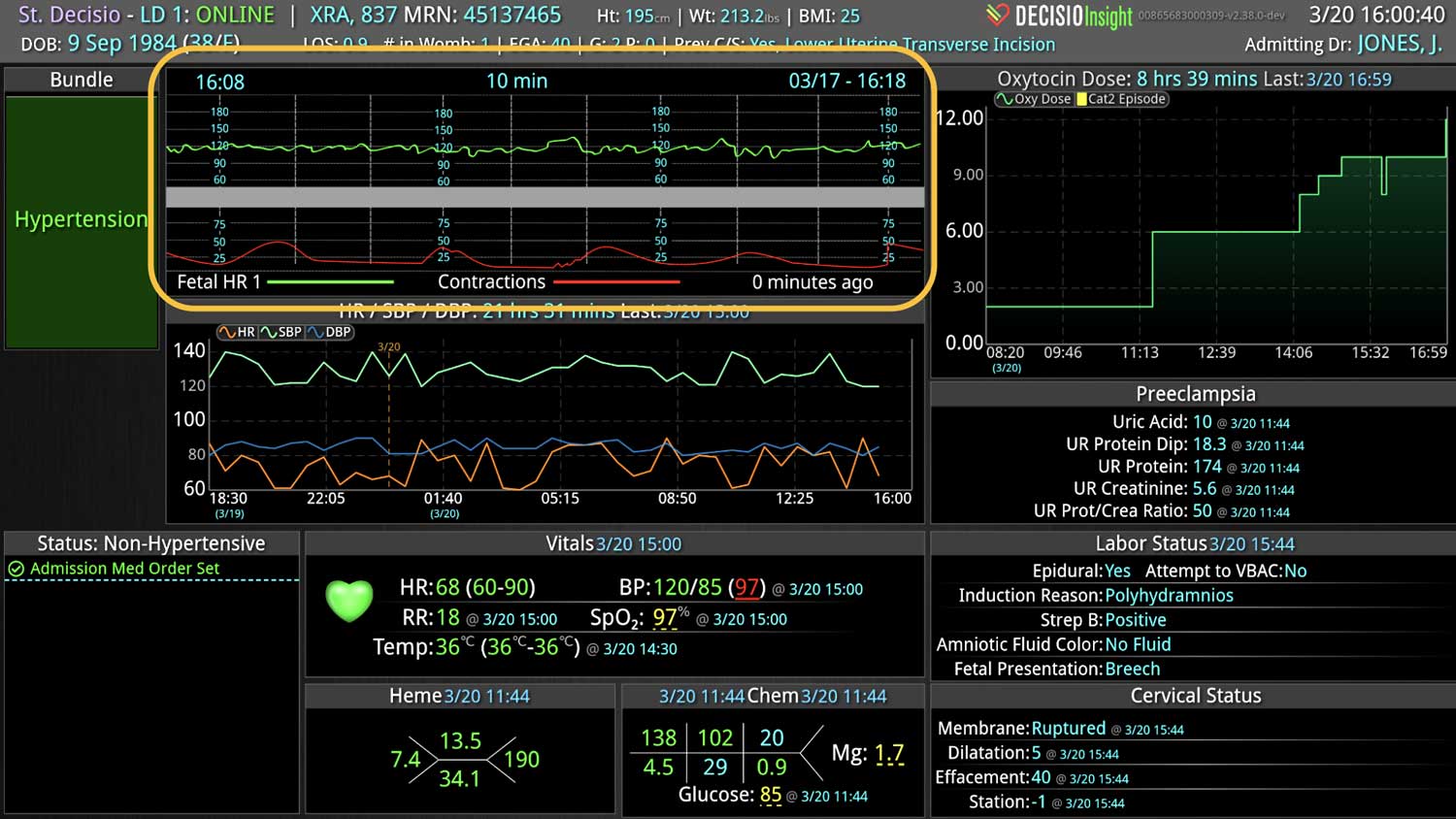
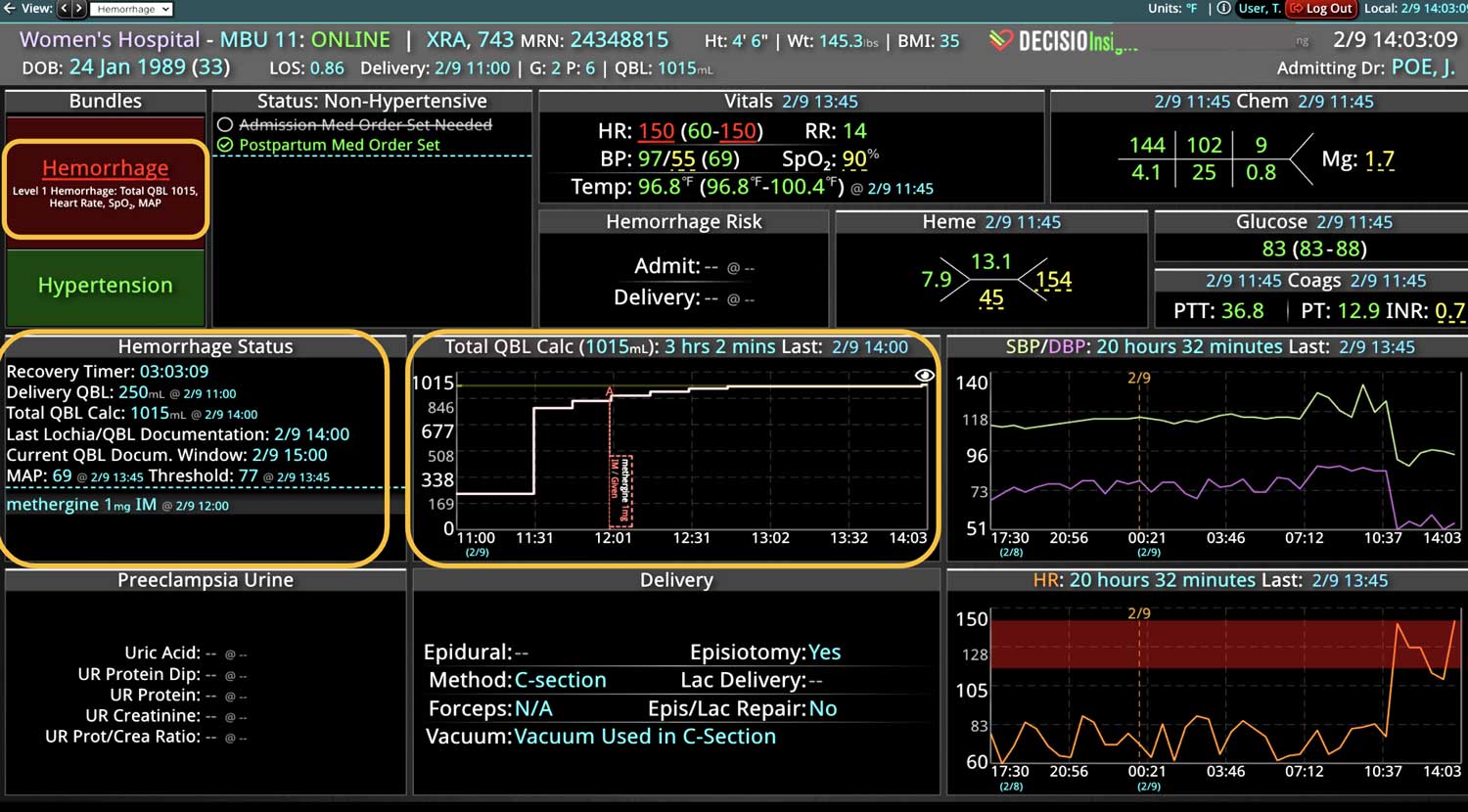
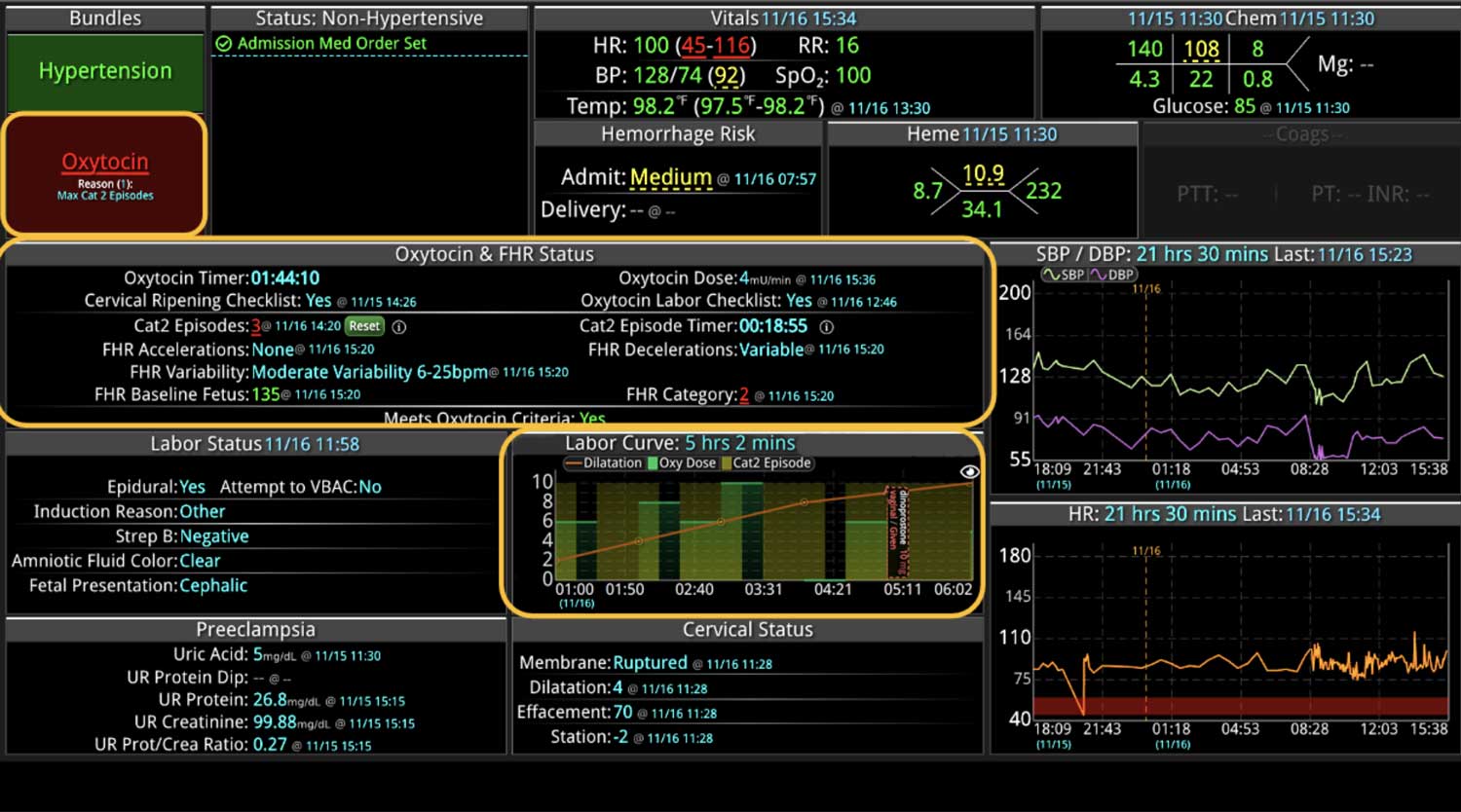
3. Implement Smart Clinical Surveillance
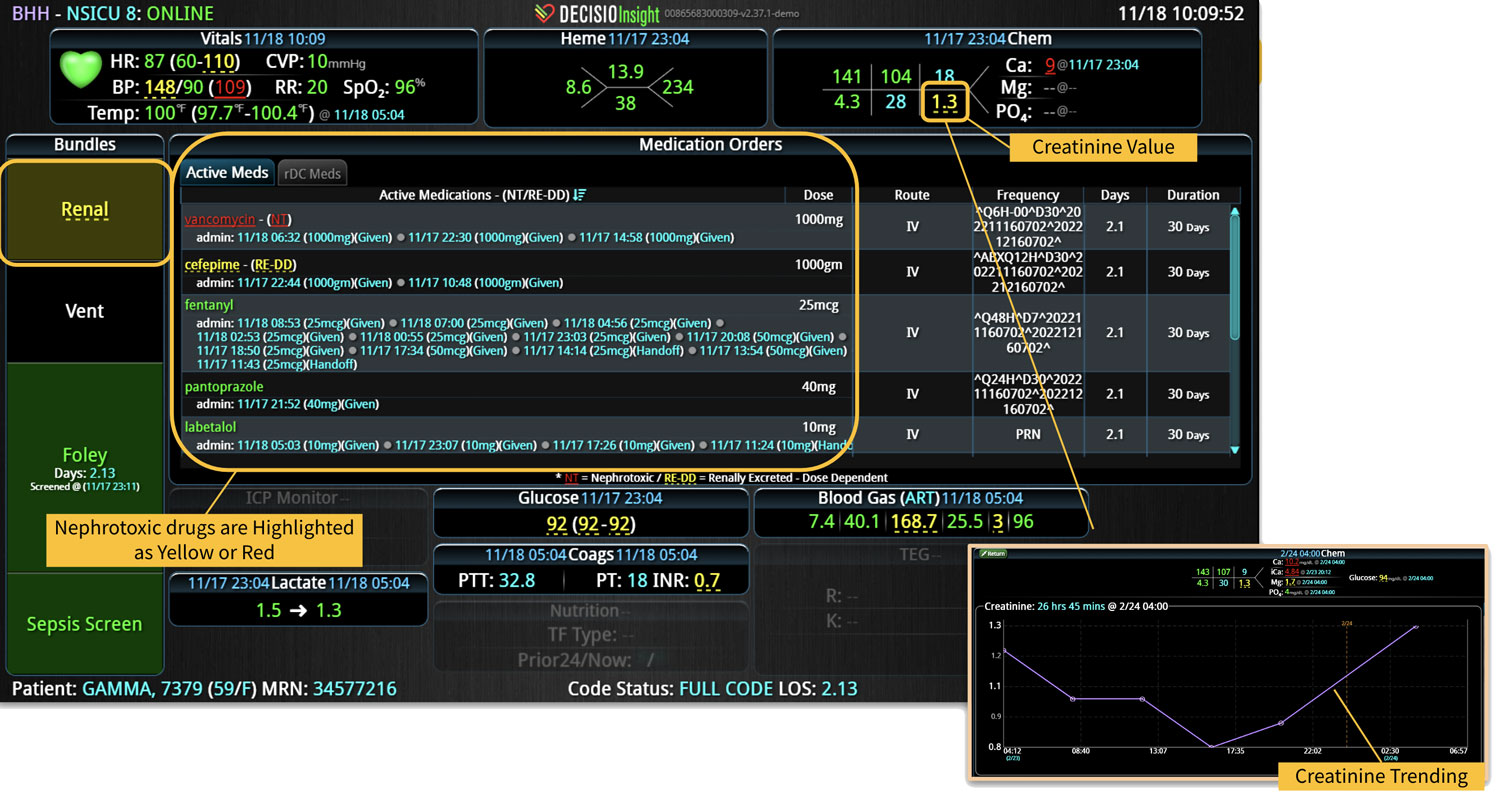
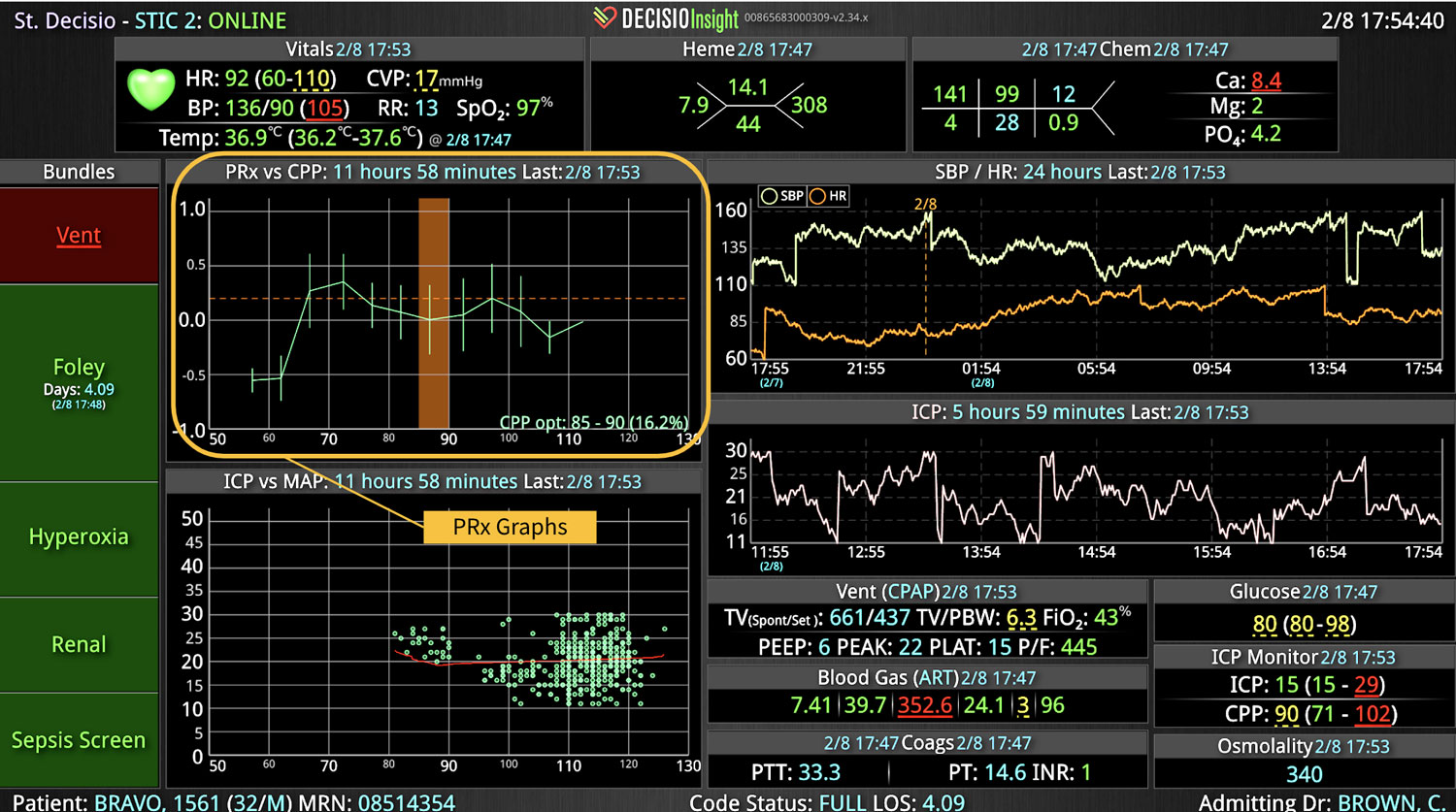
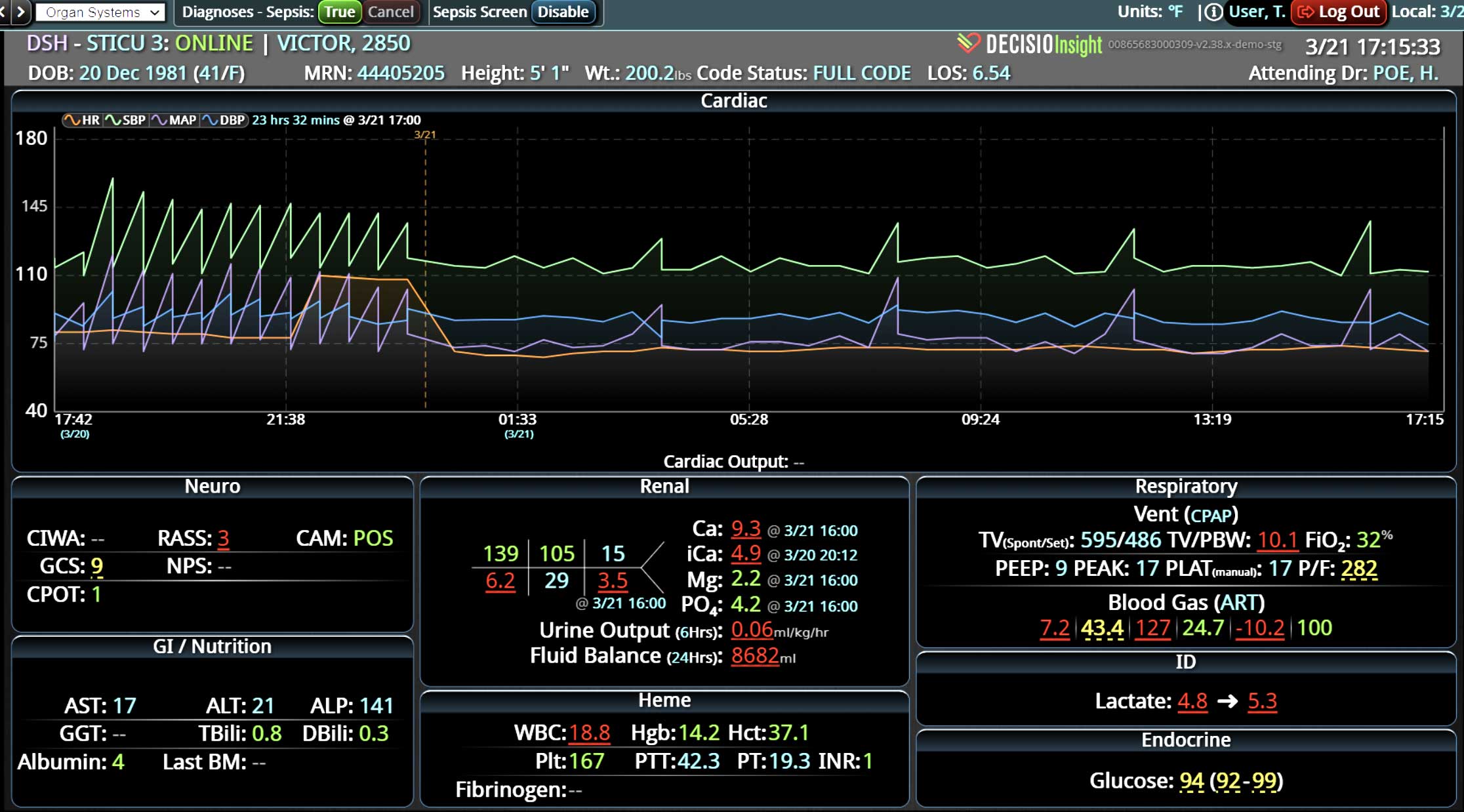
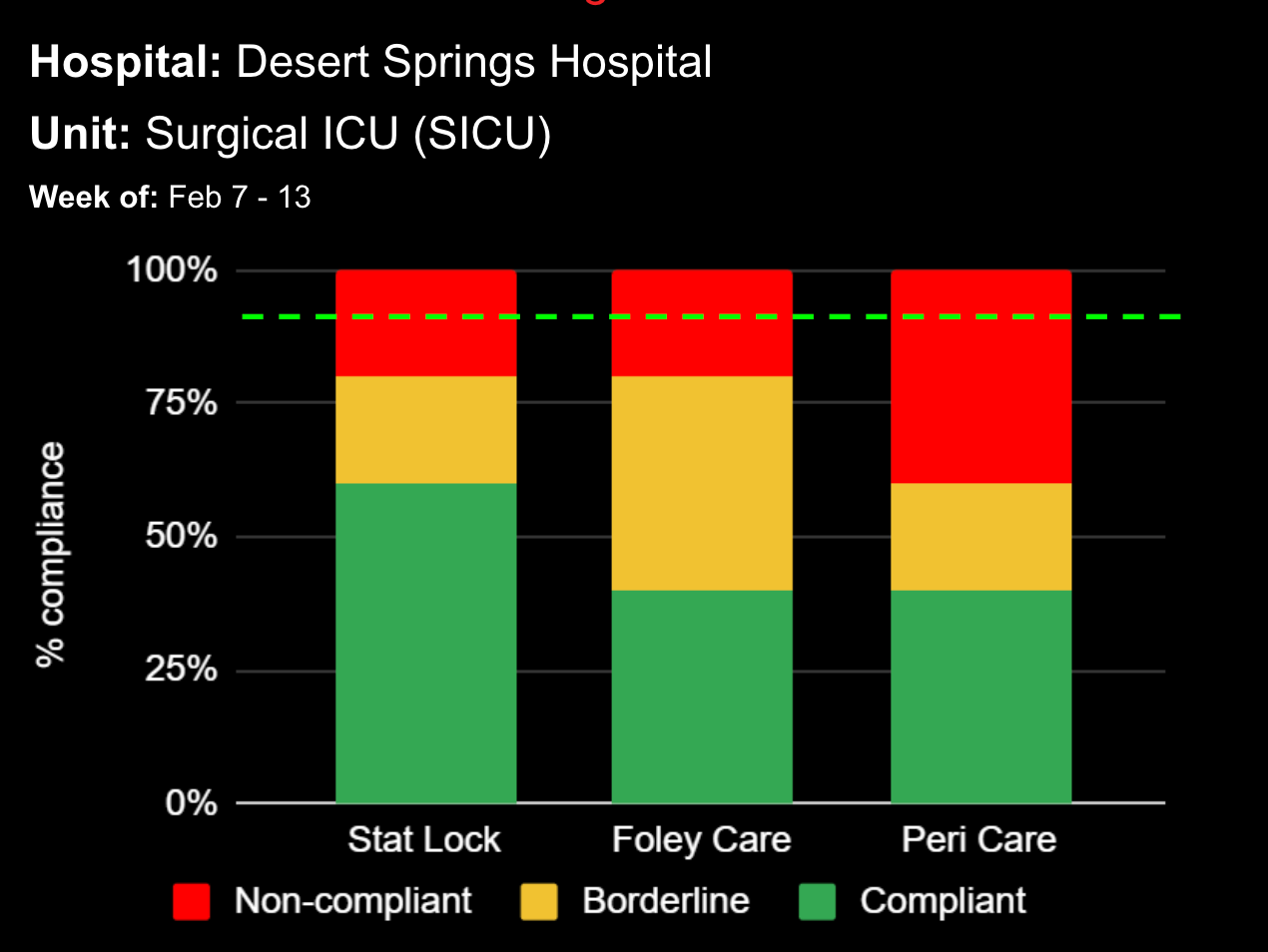
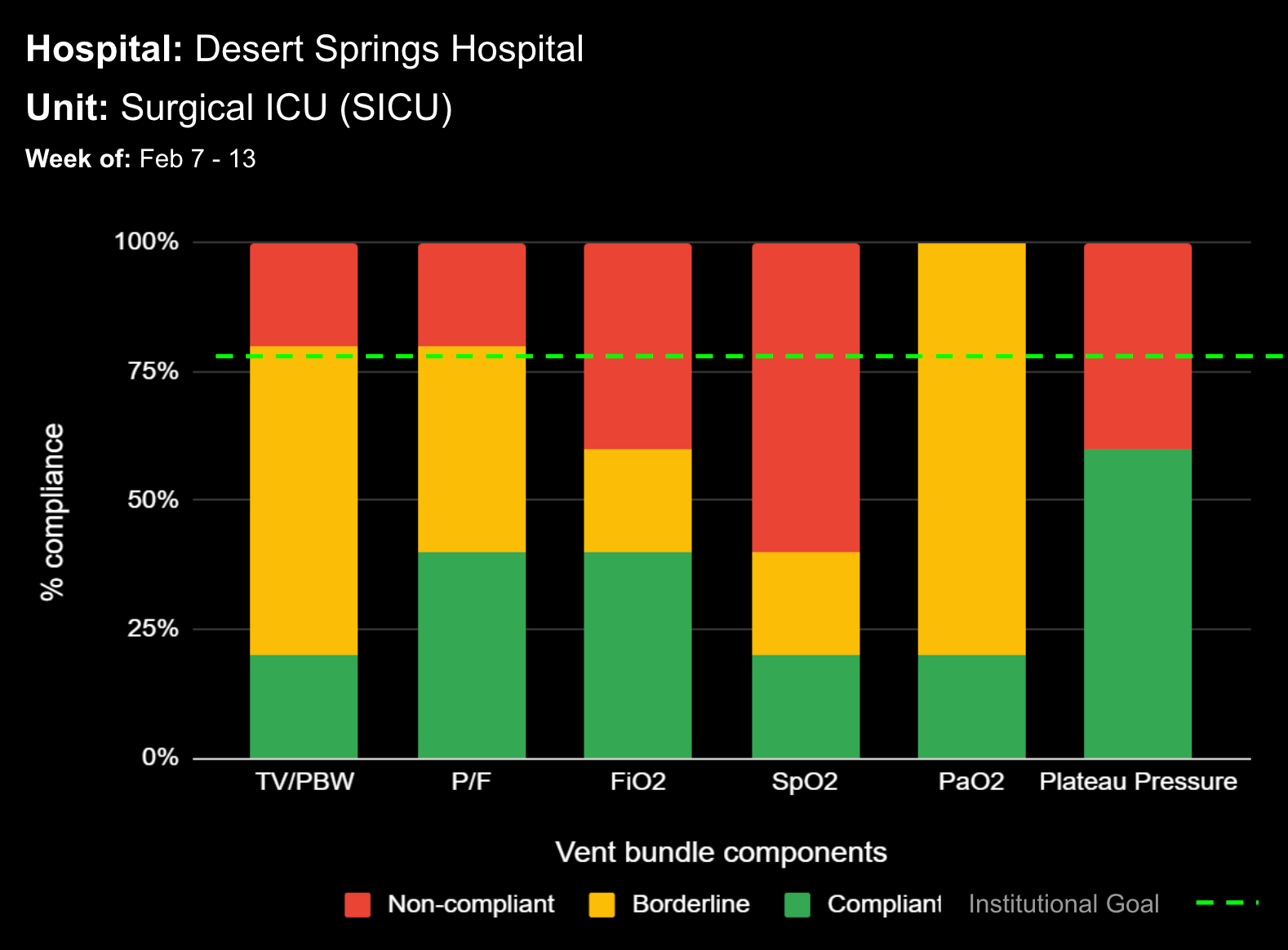
Continuous clinical surveillance integrates analytical capabilities to reveal insights that can be applied to ongoing patient care. More than a patient safety measure, clinical surveillance is a viable and sustainable solution to identify deteriorating patients for early interventions. When used in conjunction with digitized evidence-based care bundles (and their goal-directed processes), the surveillance can detect physiological changes in patients early, interpret the potential clinical implications of those changes, and alert clinicians to intervene rapidly and efficiently.
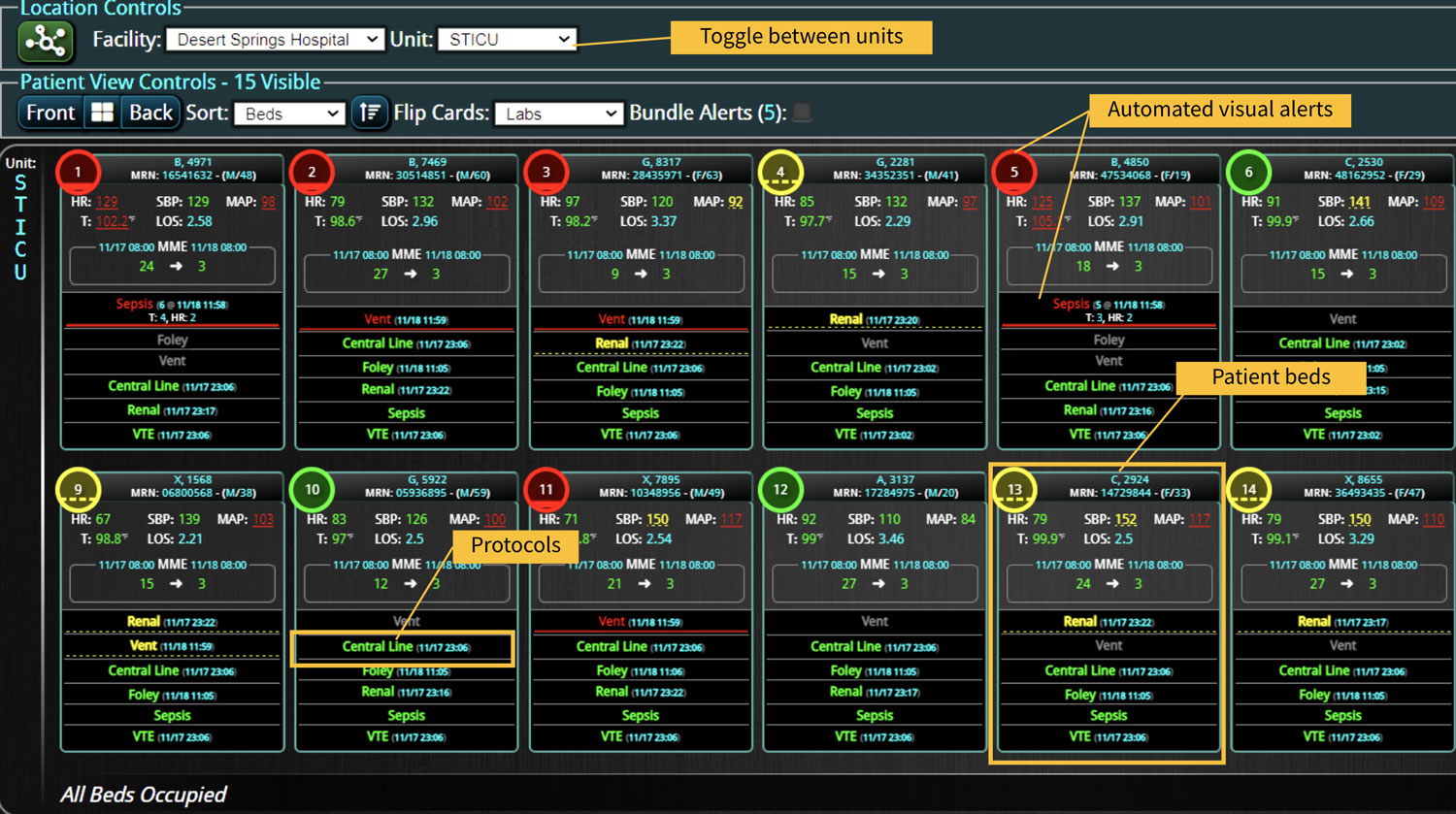
With the right technology, clinicians can monitor patients in emergency, intensive care units (ICUs), and other health care settings – at the unit, hospital, or across the health system. The surveillance system should connect to various medical devices, including ventilators, infusion pumps, and patient care monitors, and aggregate the data to identify patient developments in real time. Additionally, it should link retrospective patient data from the EHR with real-time patient vitals for early warning notifications leading to early life-saving interventions.
4. Establish a Rapid Response Team
Research consistently shows that patients exhibit signs and symptoms of deterioration for several hours before an emergency code is called. The goal of a rapid response team (RRT) is to intervene upstream from a potential code and reach the patient before deteriorating conditions turn into a crisis. While most RRTs consist of critical care nurses, they can also include respiratory therapists, pharmacists, and physicians.
Hospitals using RRTs typically observe reductions in the number of cardiac arrests, unplanned transfers to the ICU, and overall mortality rate. A 2014 study of 471,062 adult patients most likely to benefit from an RRT showed a significant decrease in hospital mortality in the post-RRT period compared to patients in the pre-RRT period (relative risk = 0.76; 95% CI = 0.72-0.80; P < 0.001).2 Similar studies have shown reduced hospital stay, ICU admissions, and non-ICU cardiorespiratory arrest. 3
5. Leverage Technology
As in any industry, the way to guarantee that the same process is uniformly followed 100% of the time is to leverage fail-safe technology that automates the process. To that end, hospitals are increasingly augmenting their RRT programs with real-time capabilities and technology to automate rapid response triggers and minimize the risk of human error.
Clinicians realize that the EHR falls short of providing meaningful, real-time, actionable triggers. In addition to the constant alert fatigue it generates, the traditional EHR alert system uses only a fraction of the available patient data. Rather than truly automate actionable triggers, the EHR involves a cumbersome time-consuming process in which someone must log in, open the record, and assess the alert before action is taken.
Technology for automated triggers must use all the available patient data to provide real-time, actionable notifications customized for the patient population and care settings. For example, medical ward patients, emergency patients, and obstetric patients would require different data points from disparate data sources to be factored into their respective RRT trigger logic.
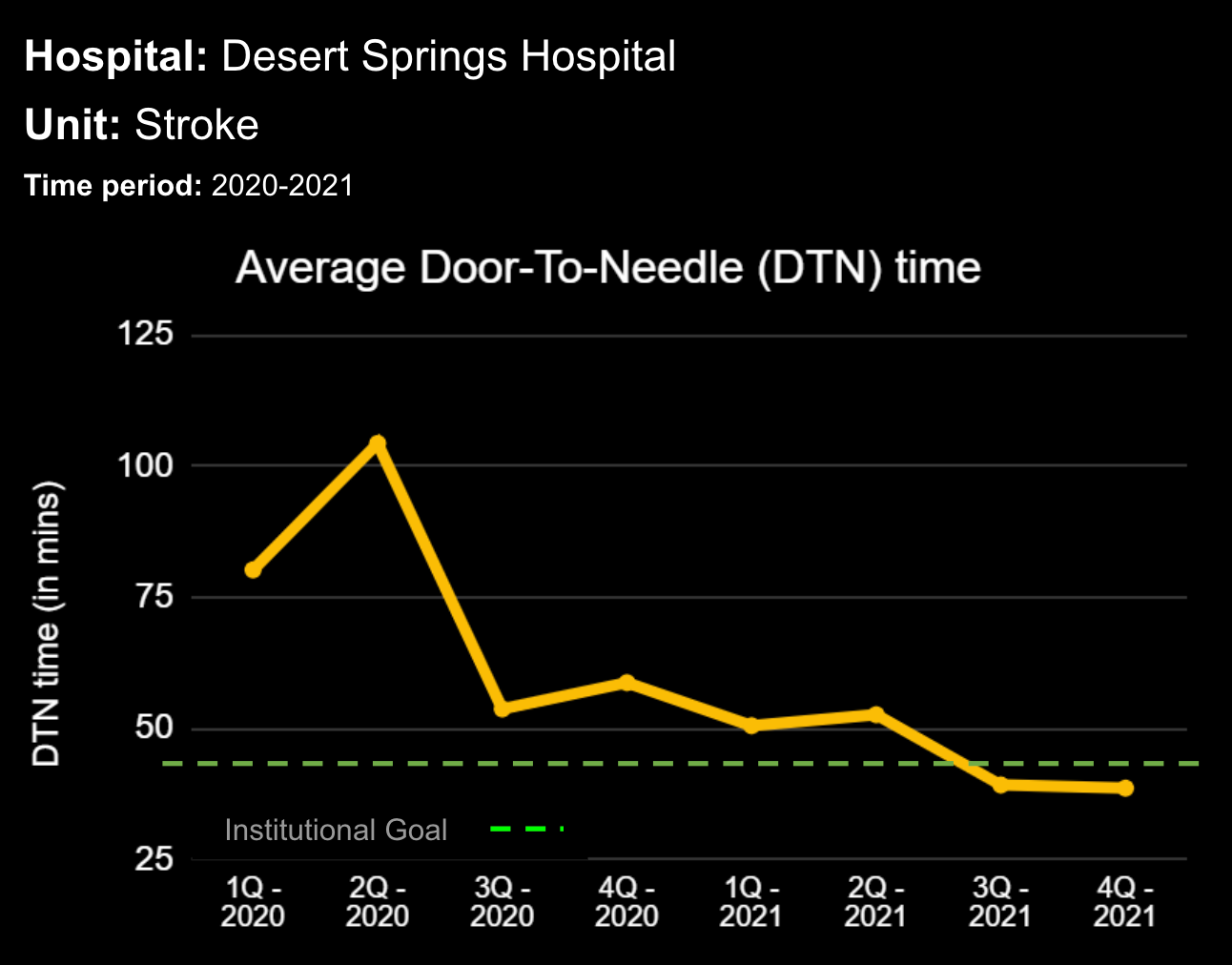
Eliminate Failure to Rescue with DECISIO’s InsightIQ
Fortunately, new RRT optimization technology exists that enables hospitals to provide real-time surveillance, beyond the EHR, for early intervention. Providing the right data, at the right time, to the right clinician 100% of the time and doing it earlier and more often is how hospitals are leading the way to the next generation of rapid response programs.
Real-time monitoring of patient populations on a single platform triggers RRTs for at-risk patients and prevents unexpected escalation of care. A single easy-to-read screen on the platform also facilitates real-time compliance with clinical protocols. Research shows that every 10% increase in compliance with recommended care reduces the risk of death by 14%.4
InsightIQ is an FDA-cleared, web-native software that uses continuous, smart bedside monitoring that empowers clinical teams to identify at-risk patients and efficiently comply with established clinical guidelines. The InsightIQ software can meet the needs of a wide range of hospital systems and departments to help your team optimize clinical workflow and responses, thereby reducing click fatigue and the length of hospitalization while contributing to improved patient outcomes.
DECISIO is a Texas-based company with deep expertise in the health care industry and information technology. Our software experts work alongside clinicians and administrators to provide a framework for developing unique programs to address specific FTR situation.
Learn more about InsightIQ and DECISIO’s suite of products at: https://www.decisiohealth.com
References
1. Smith MEB, Chiovaro JC, O’Neil M, et al. Early Warning System Scores: A Systematic Review [Internet]. Washington (DC): Department of Veterans Affairs (US); 2014 Jan. Available from: https://ncbi.nlm.nih.gov/books/NBK259029/
2. Salvatierra G, Bindler RC, Corbett C, et al. Rapid Response Team Implementation and In-Hospital Mortality. Crit Care Med. 2014; 42(9): 2001-6. doi: 10.1097/CCM.0000000000000347
3. Stolldorf DP, Jones CB. The Deployment of Rapid Response Teams in U.S. Hospitals. Jt Comm J Qual Patient Saf. 2015; 41(4): 186–183. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4445360/
4. Shafi S, Barnes SA, Rayan N, et al. Compliance with Recommended Care at Trauma Centers: Association with Patient Outcomes. J Am Coll Surg. 2014; 219(2):189-98. doi: 10.1016/j.jamcollsurg.2014.04.005
Learn more About How we help clinicians improve patient outcomes
Schedule a call with our team to discuss how we are helping our clients revolutionize how clinicians manage patient interventions.