25 Apr How Healthcare Information Technology is Improving Patient Safety Today
How Healthcare Information Technology is Improving Patient Safety Today
In 2009, the Health Information Technology for Economic and Clinical Health Act (HITECH) was passed by the United States Congress to “promote the adoption and meaningful use of health information technology.”1 The legislation incentivized providers and institutions to adopt the use of electronic health records that provided advantages, such as increased availability and transferability of information and legibility.2 However, like most technology, medical software has exponentially grown in capability and application. While not all systems are equal, the increased adoption of healthcare information technology has been universal, and most advanced health care teams now use clinical decision support (CDS) systems.
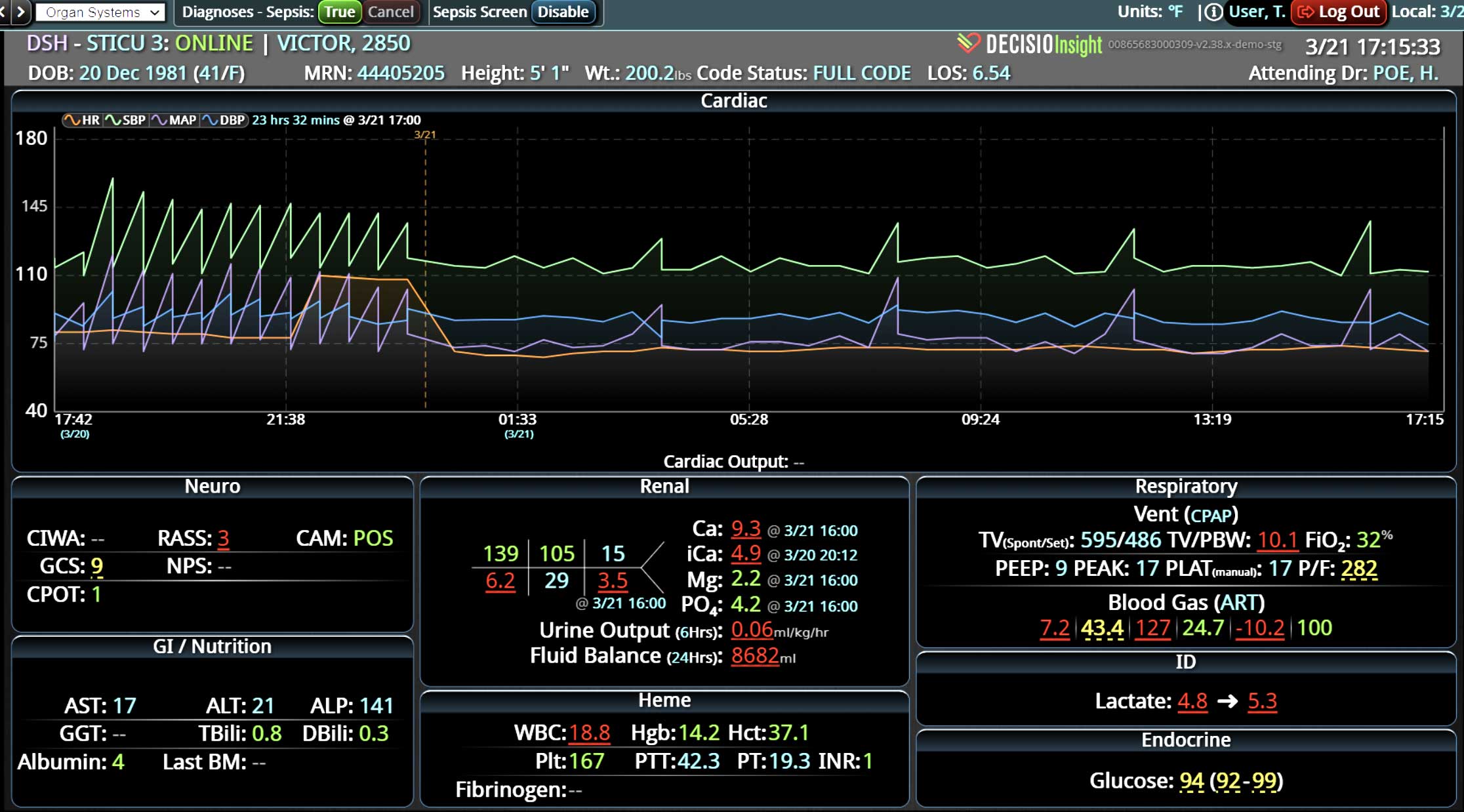
Broadly defined, CDS systems use technology, clinical evidence, and real-time patient data to support health care team decisions. The system integrates relevant patient information from multiple sources of patient data and provides real-time outputs to the clinical team. Integration of CDS with the clinical workflow can improve the quality and safety of patient care. A CDS system can also incorporate predictive analytics and machine learning algorithms to help providers identify potential risks and make more informed decisions. They can provide alerts, reminders, and suggestions for clinical decision-making, such as recommended medications, dosages, or diagnostic tests. In fact, multiple studies have shown that use of optimal technology can improve patient safety by reducing the risk of medication errors.3-5
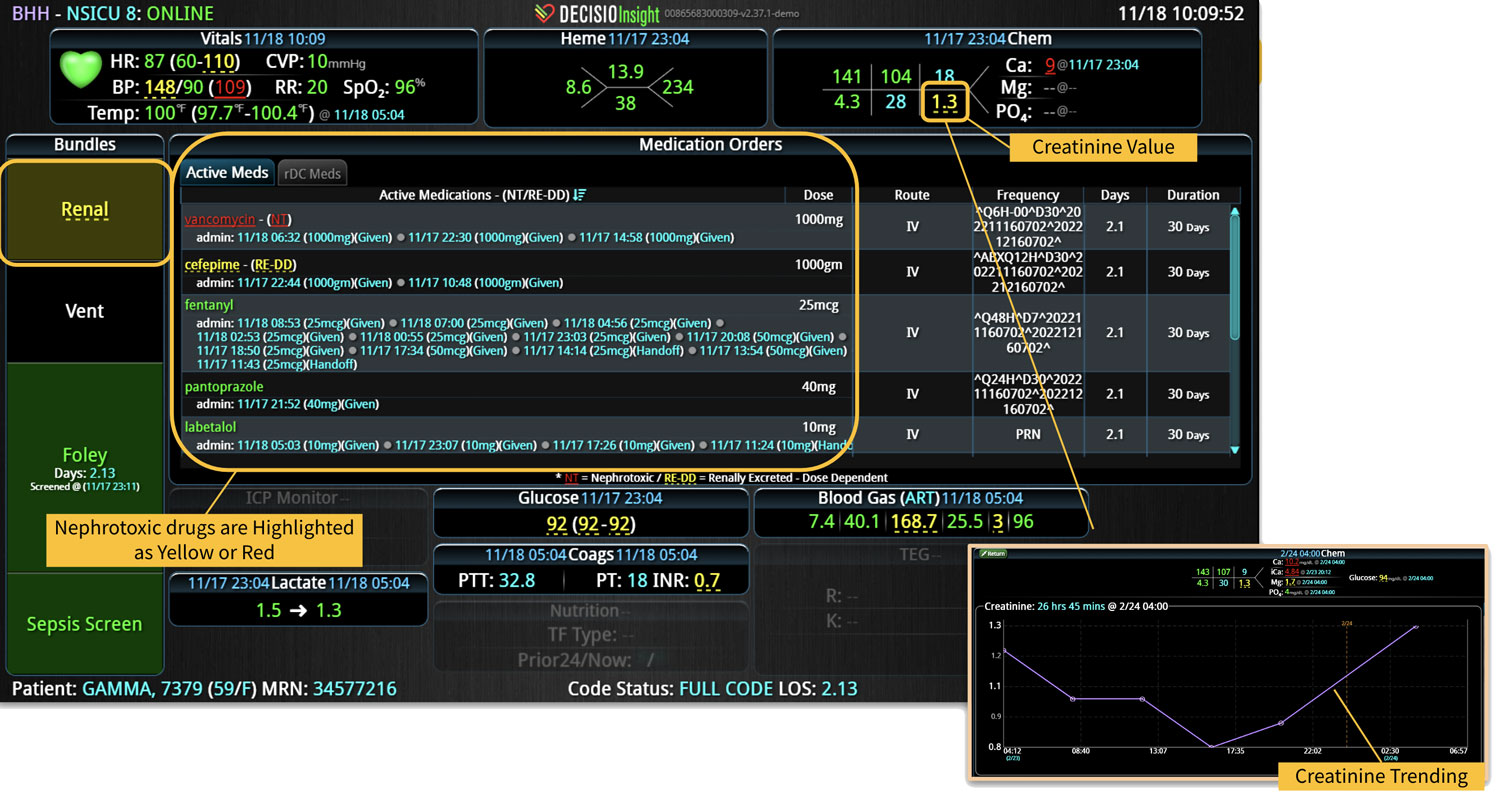
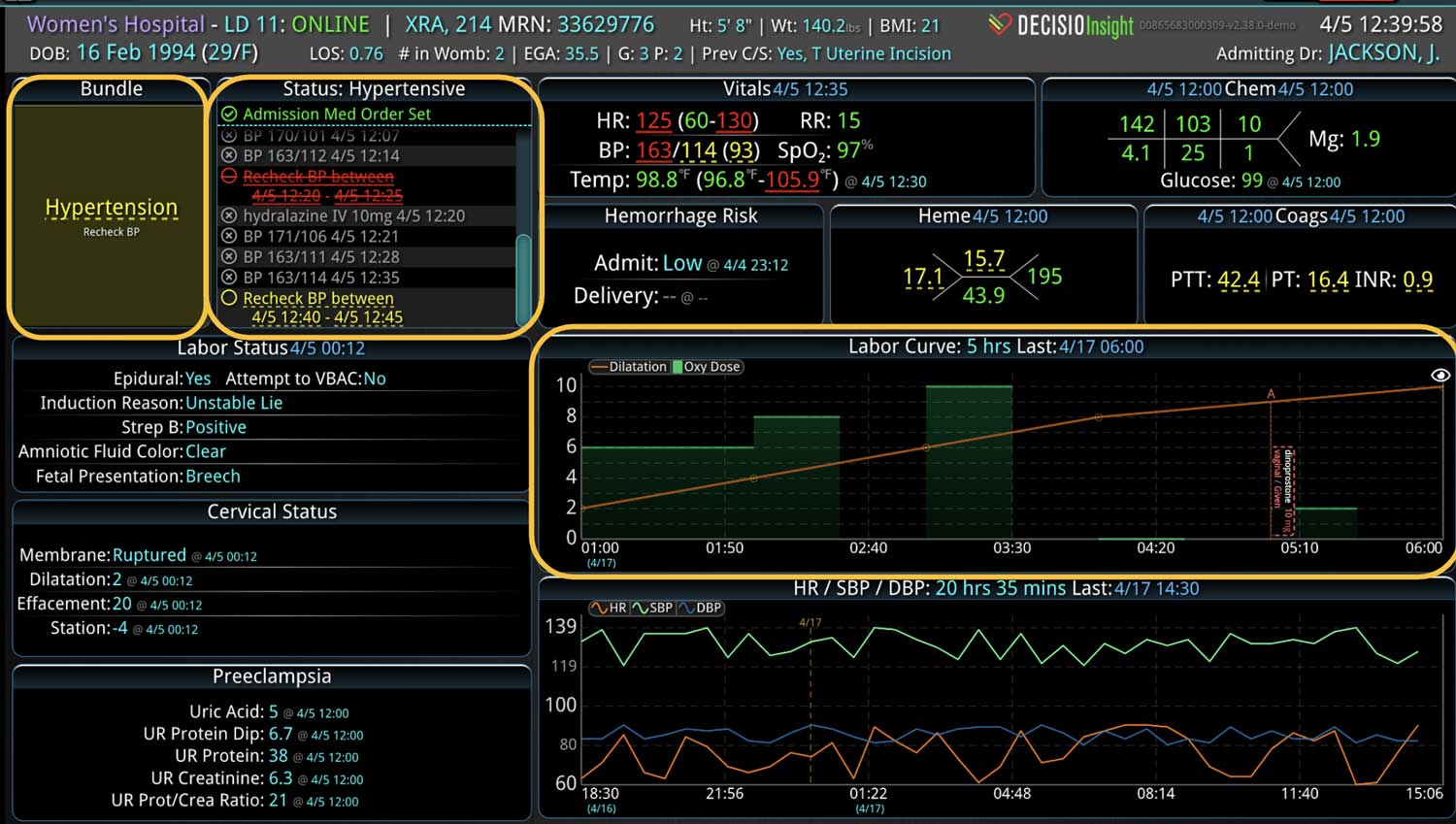
Specifically, CDS systems can improve patient safety by reducing medication error risk in multiple ways. In addition to checking for drug allergies, drug-drug interactions, or appropriate dosage recommendations, CDS systems can also provide:
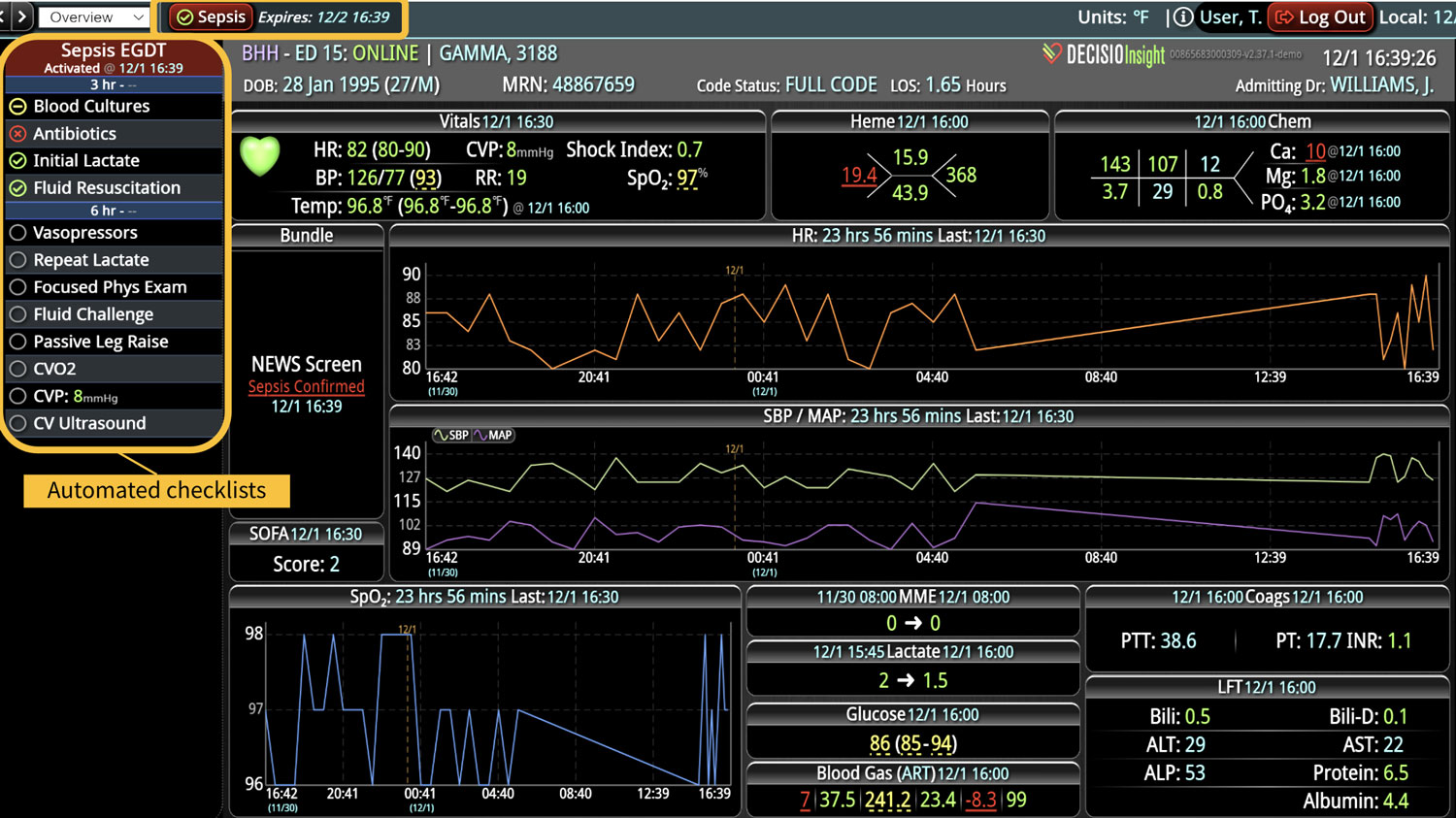
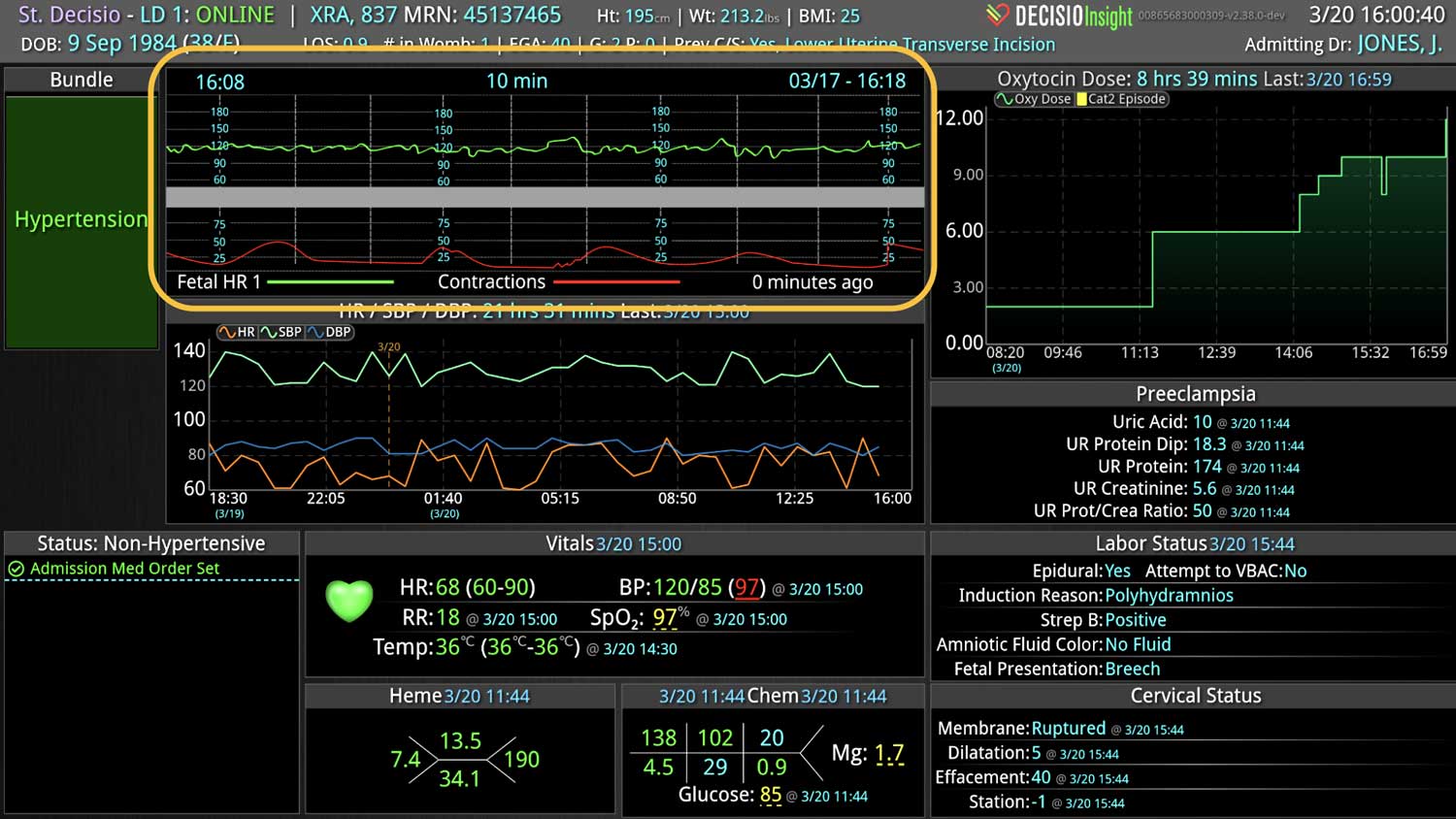
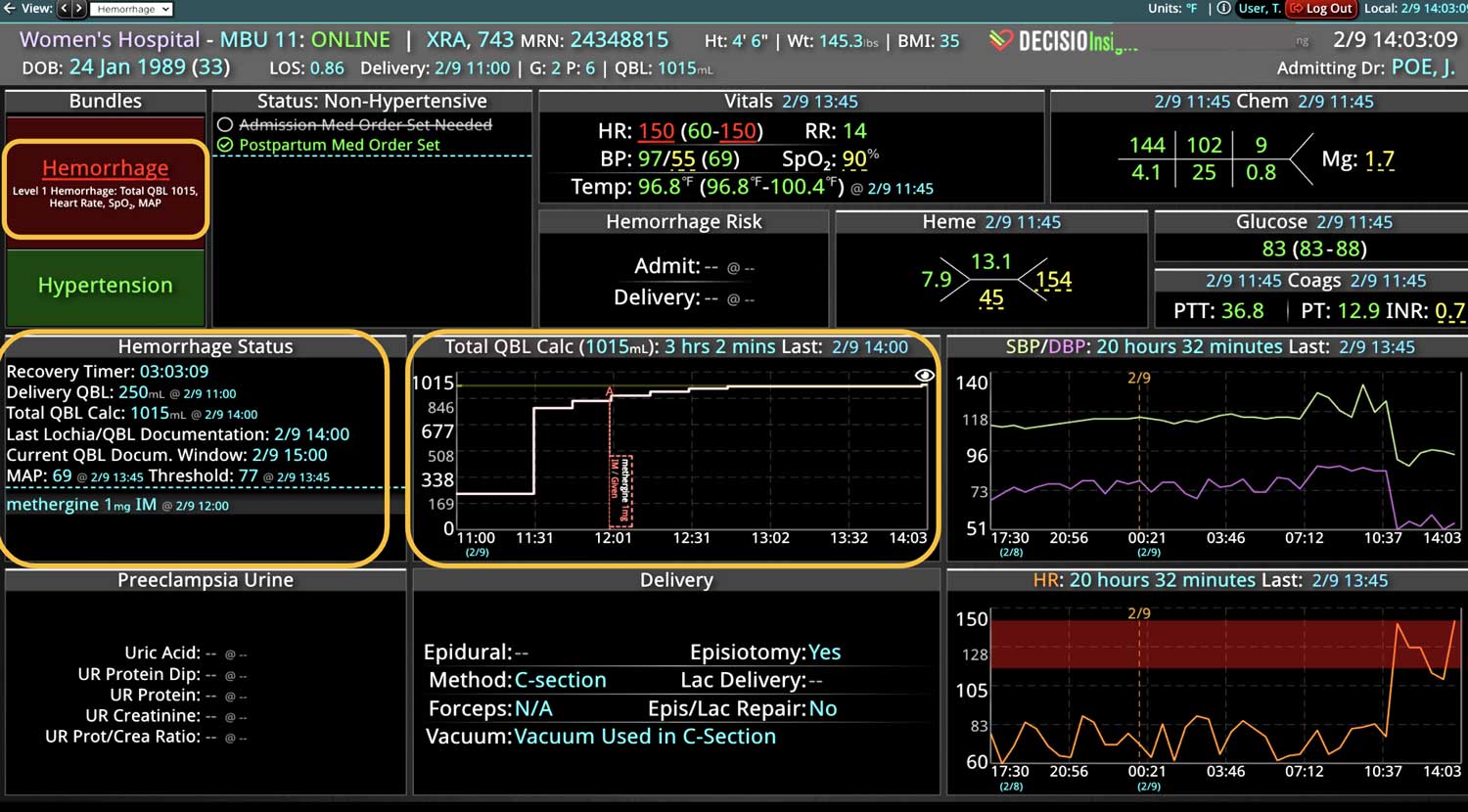
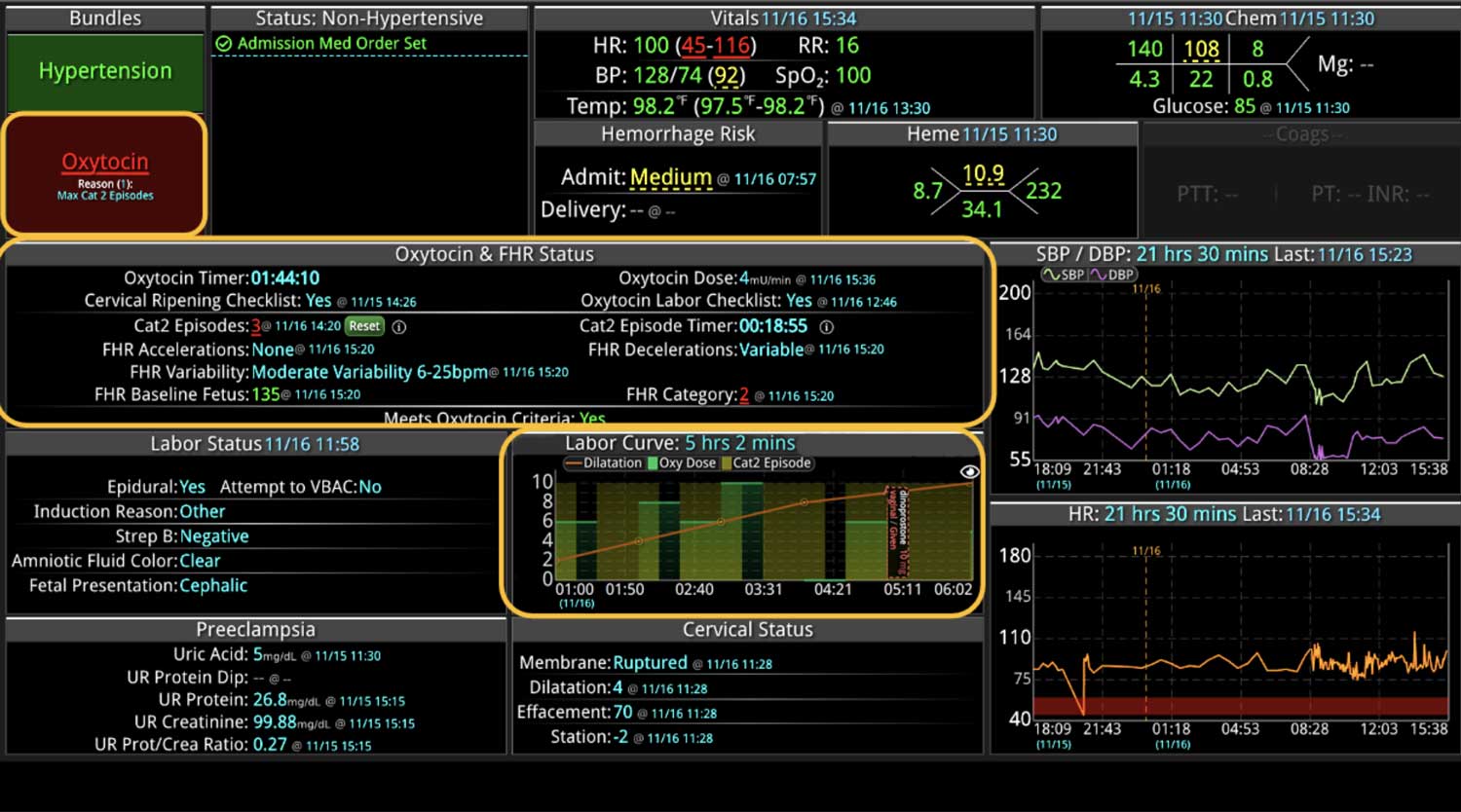
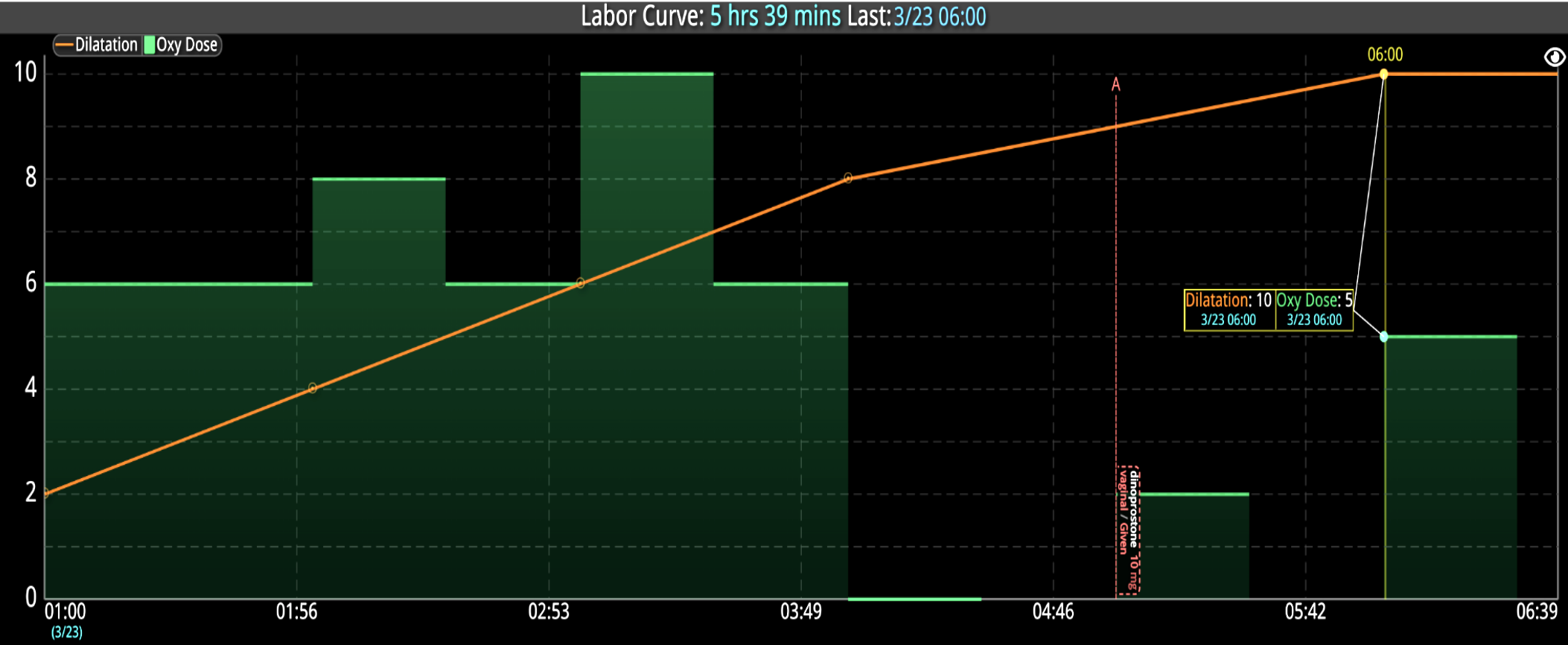
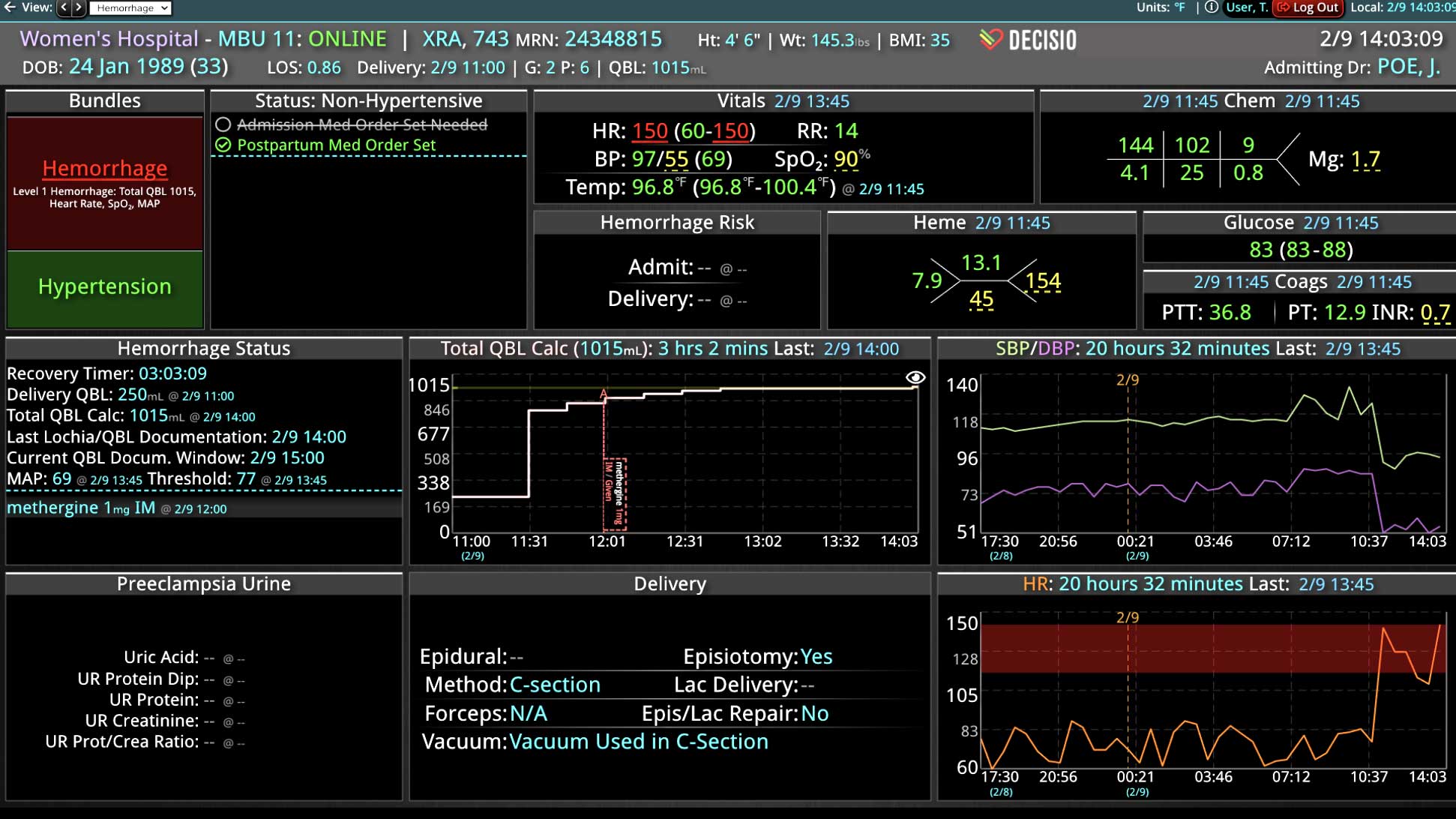
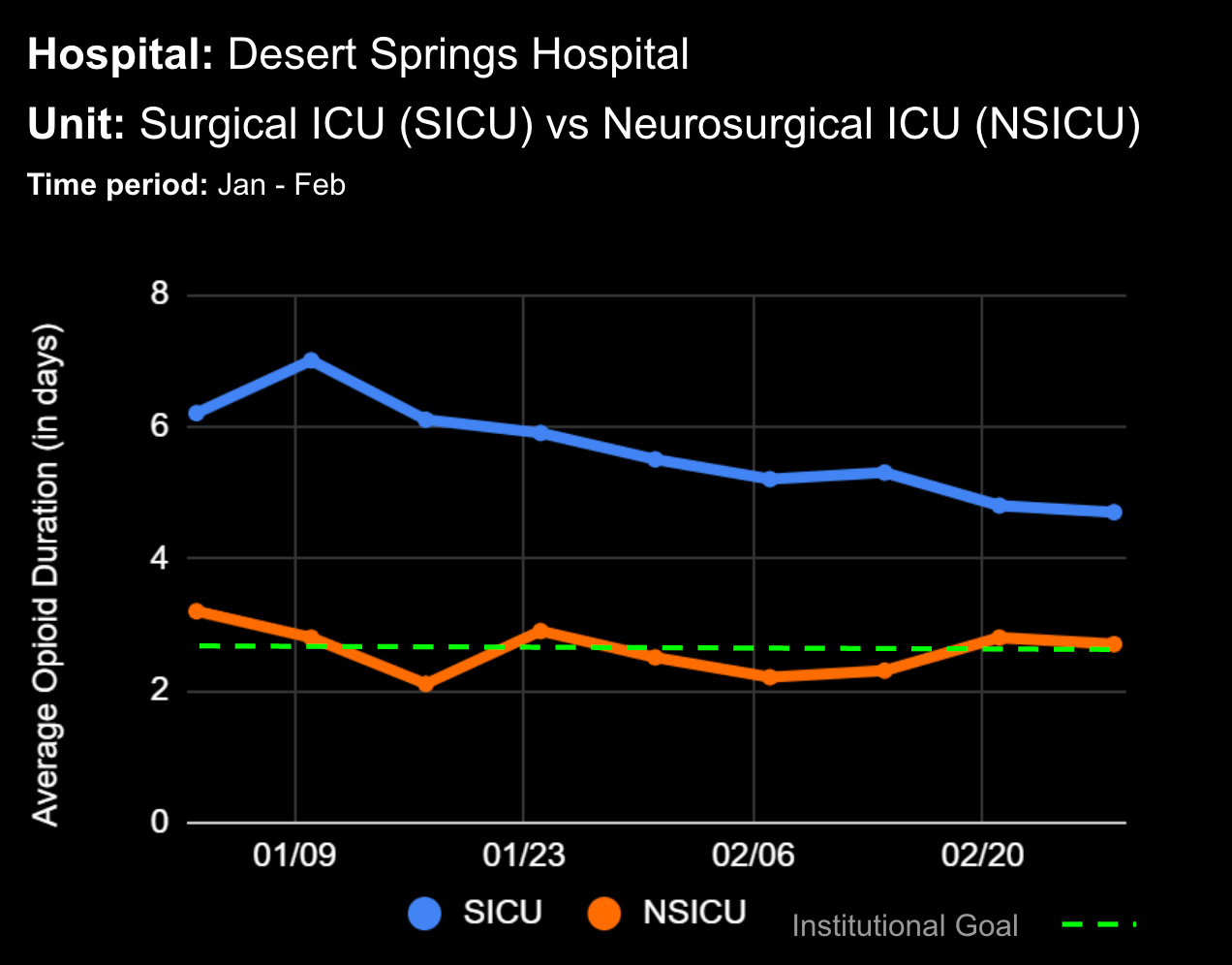
- Real-time medication monitoring: CDS can continuously monitor medication orders, dosage changes, medication administration, and the effect of those medications on the patient’s vital signs.
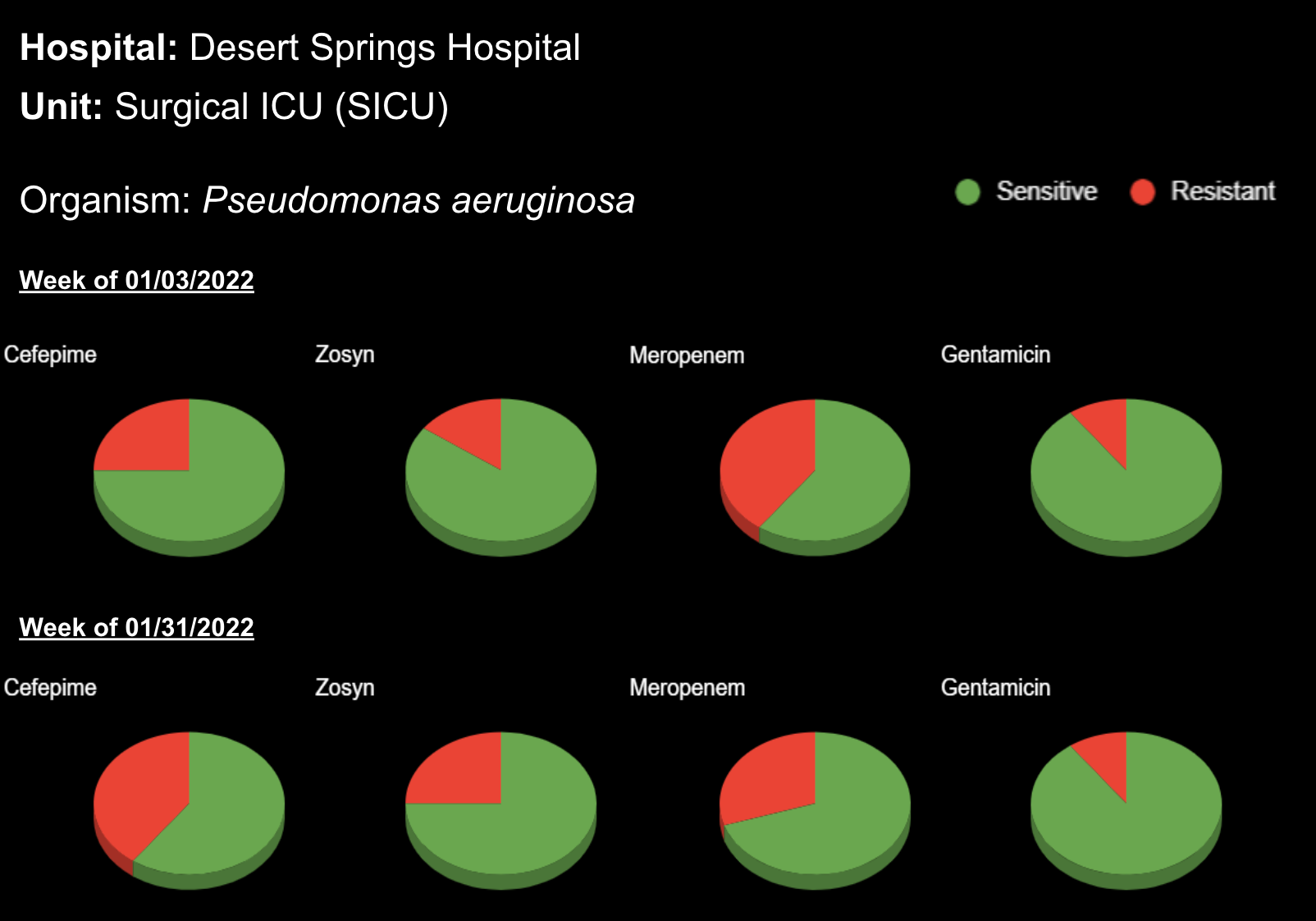
- Evidence-based recommendations: CDS can provide clinicians with the latest evidence-based guidelines and recommendations for medication use, including up-to-date sensitivity patterns for antibiotic administration.
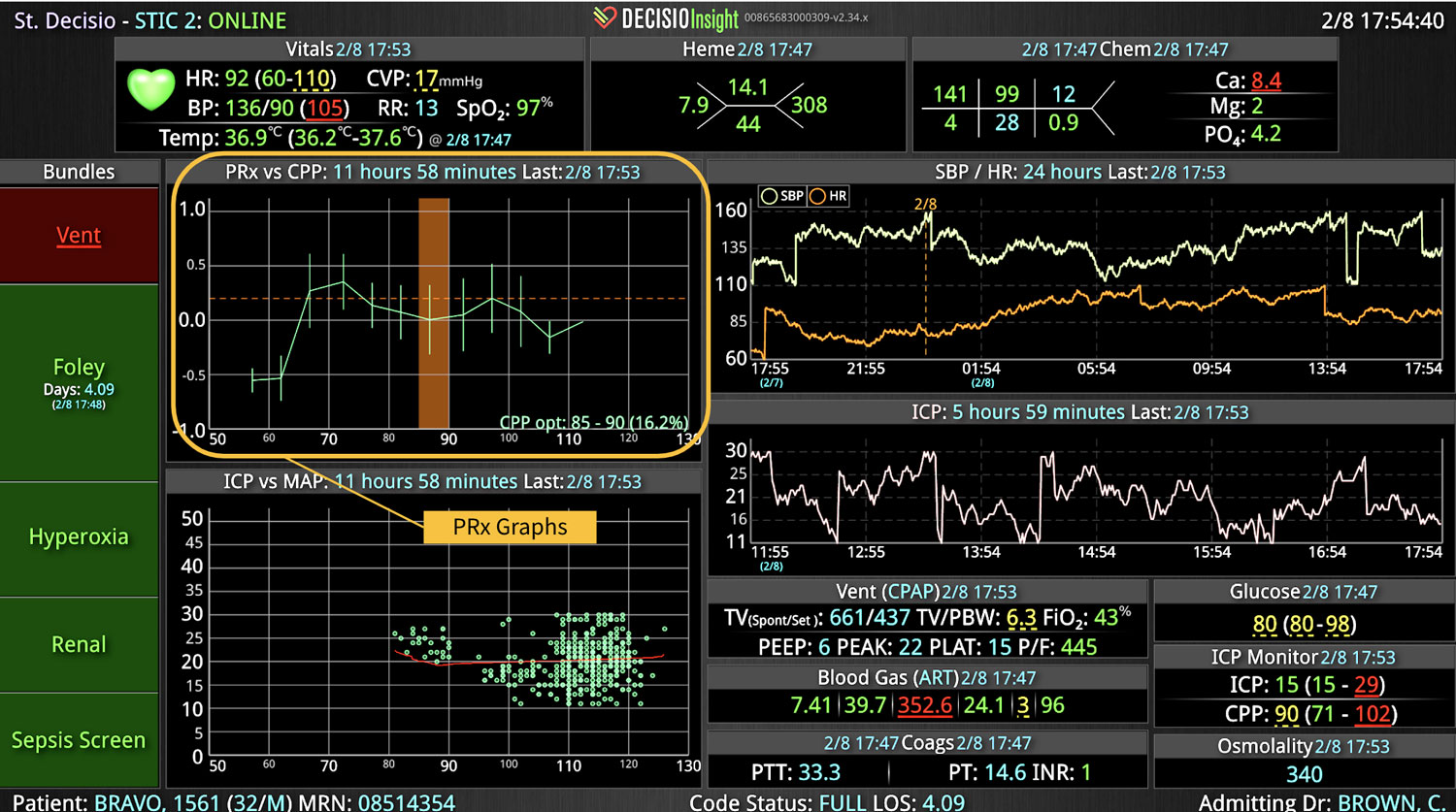
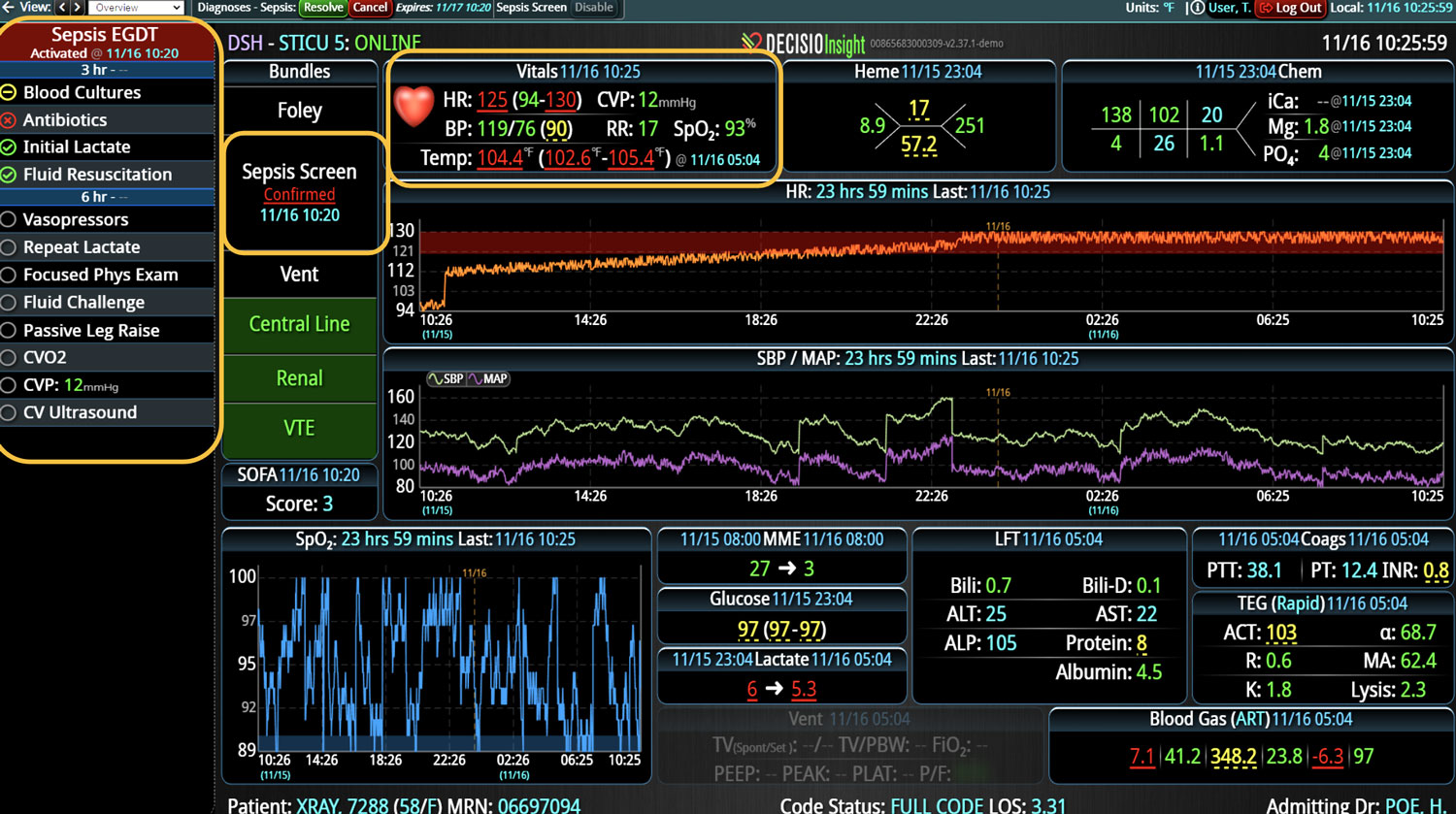
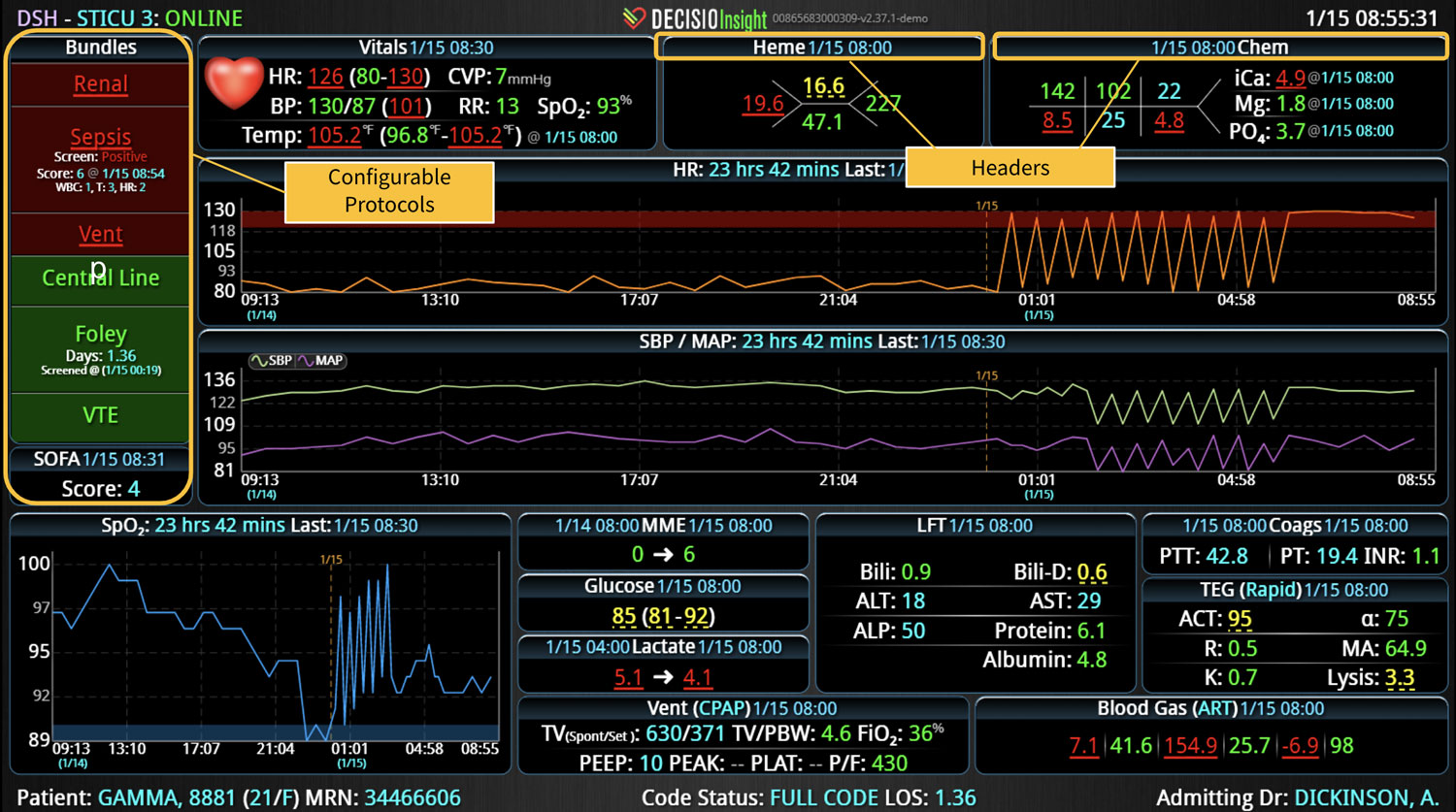
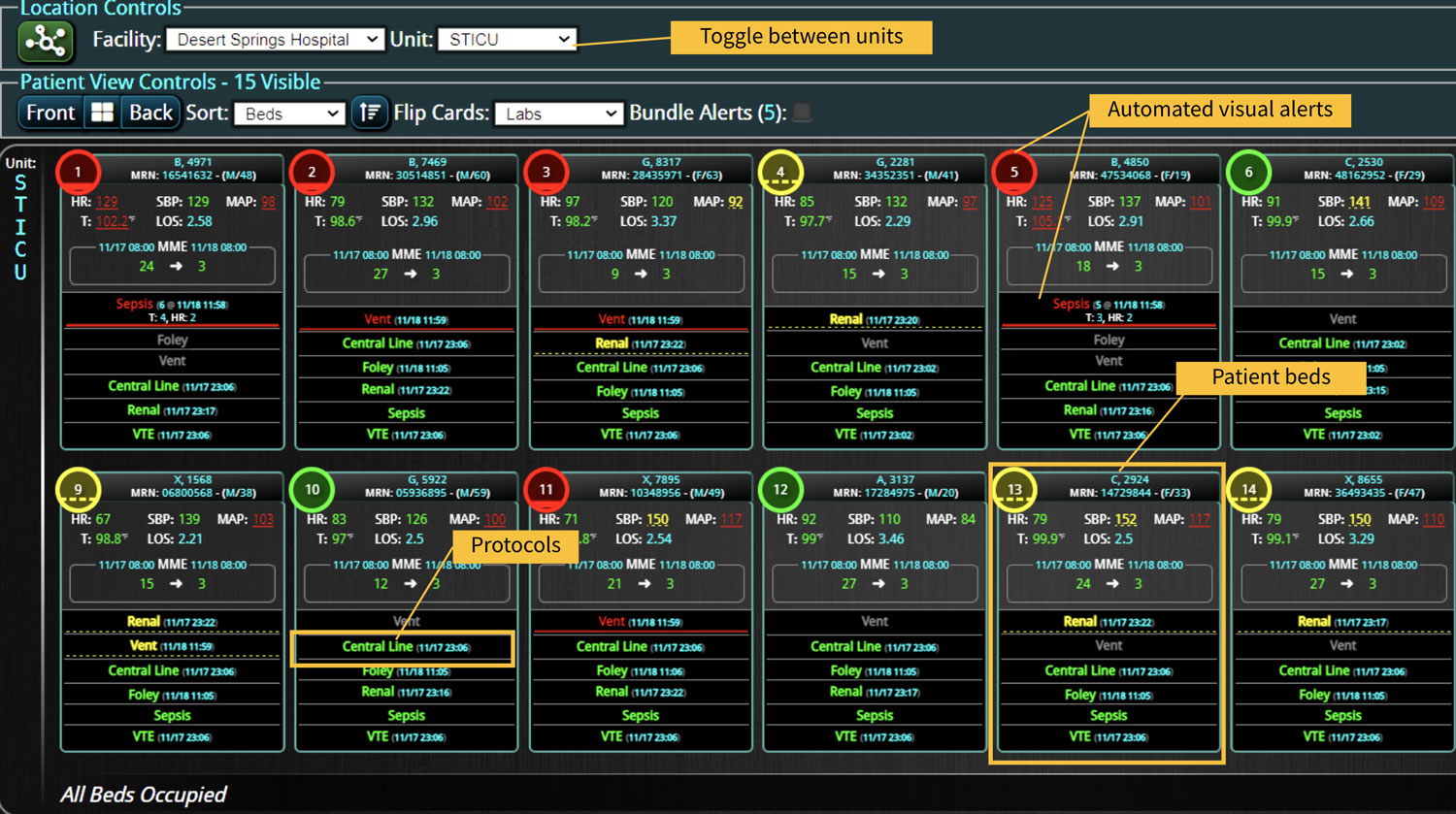
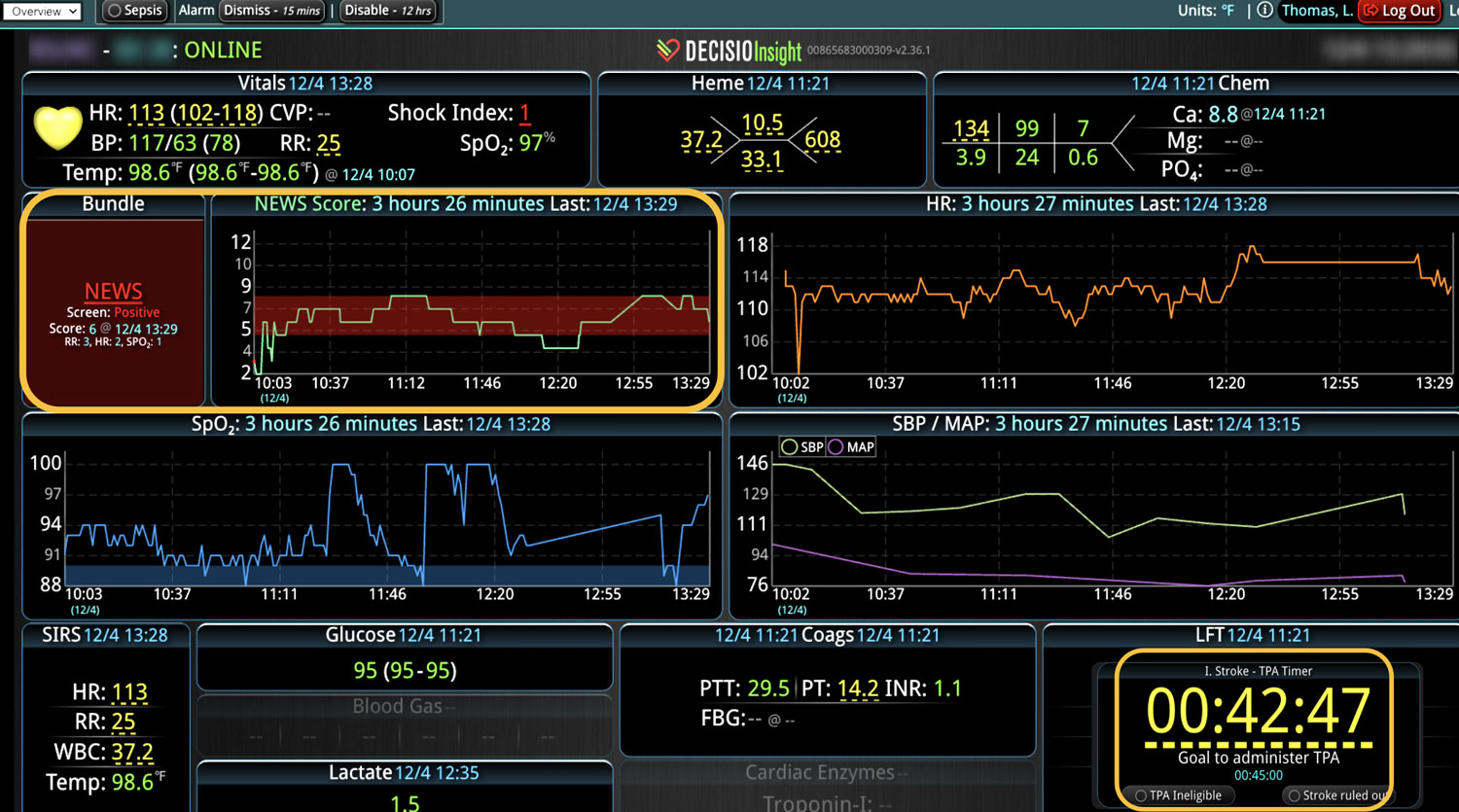
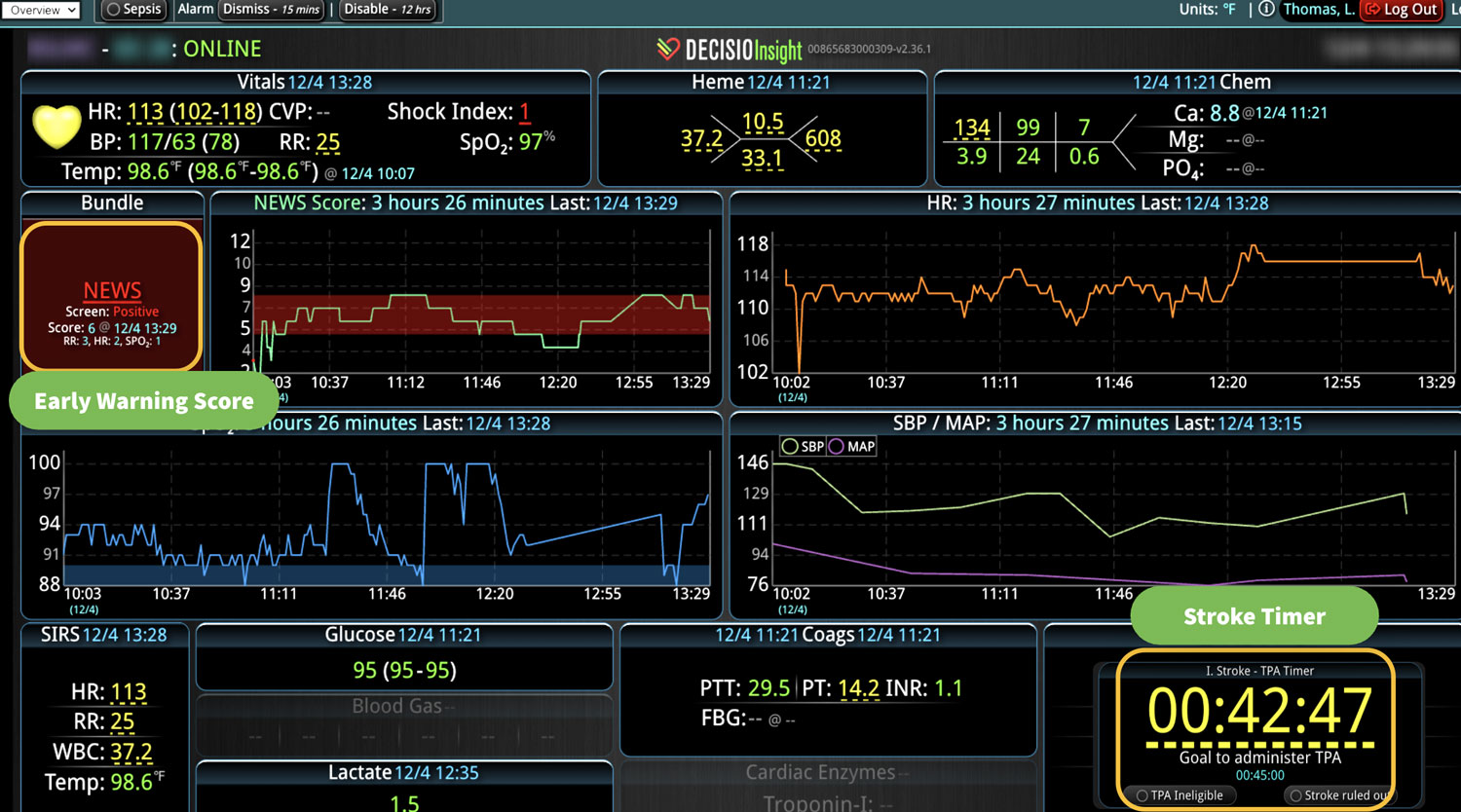
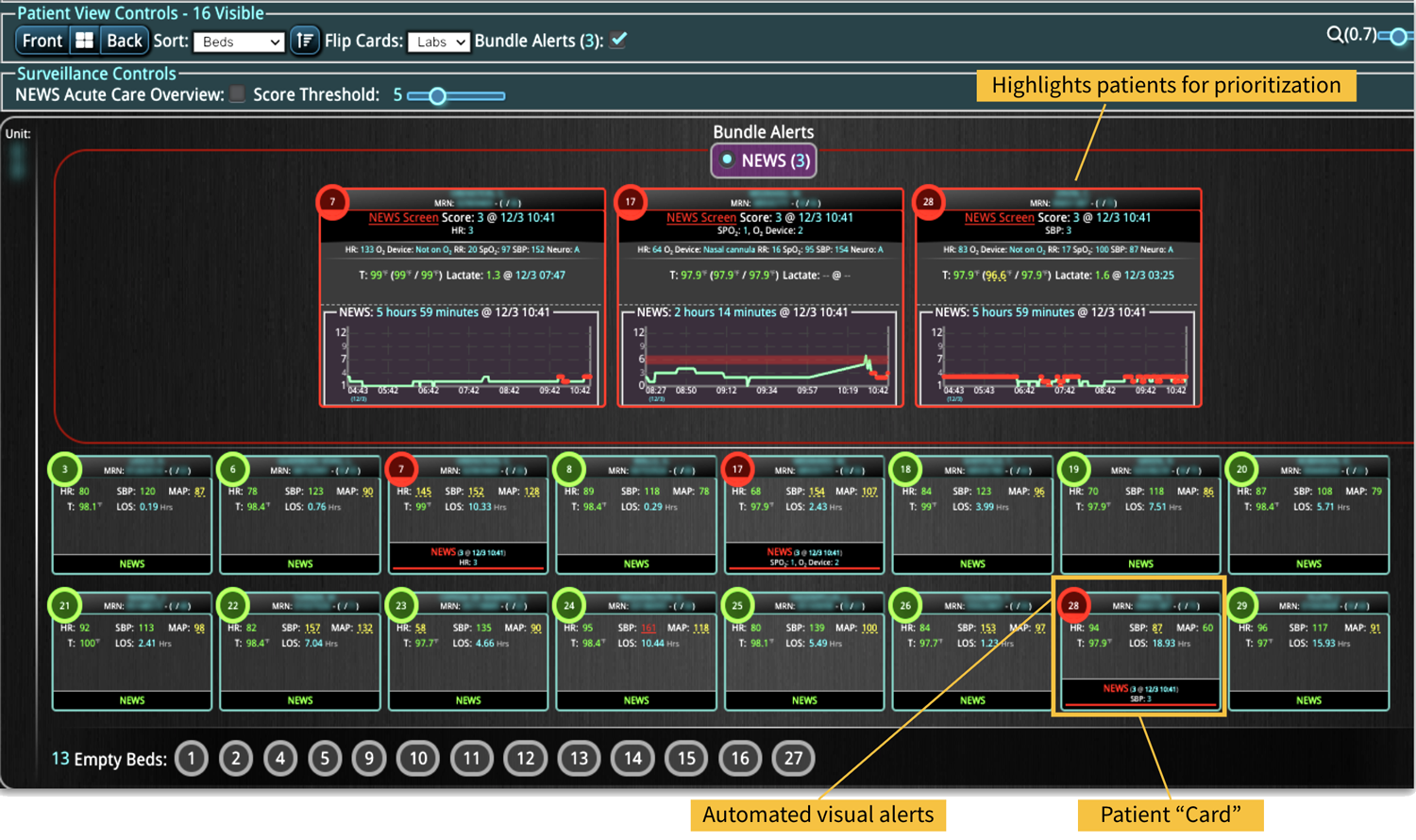
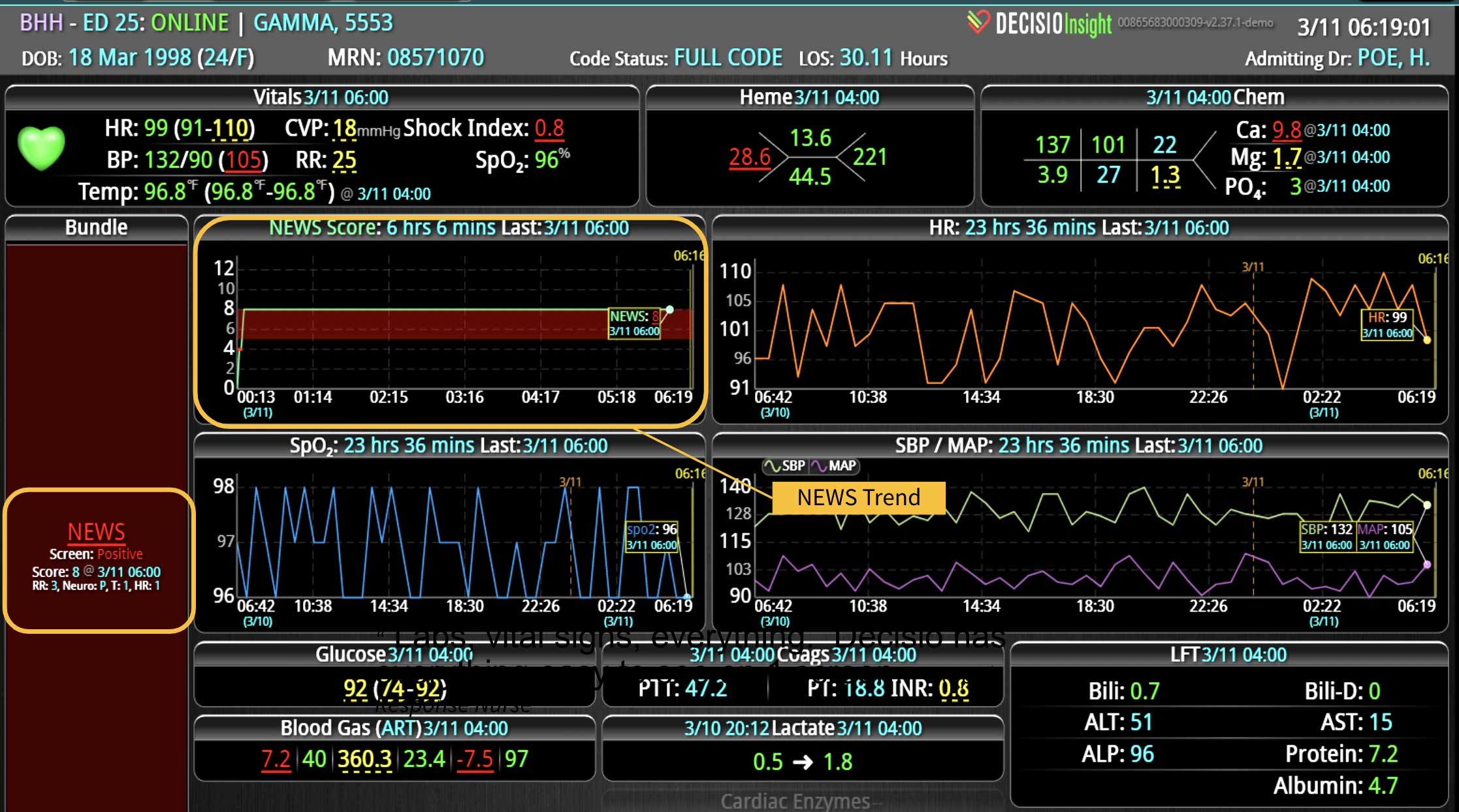
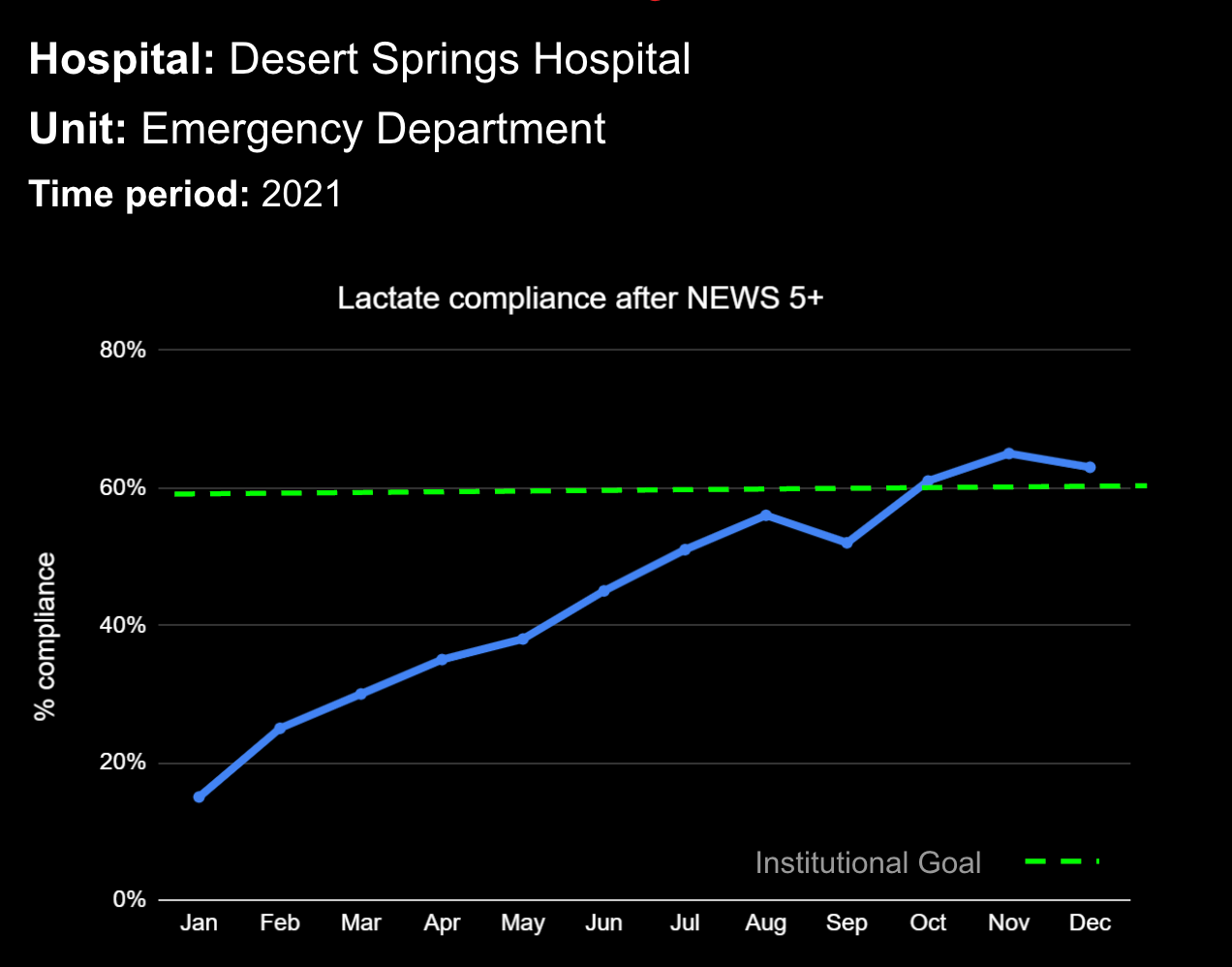
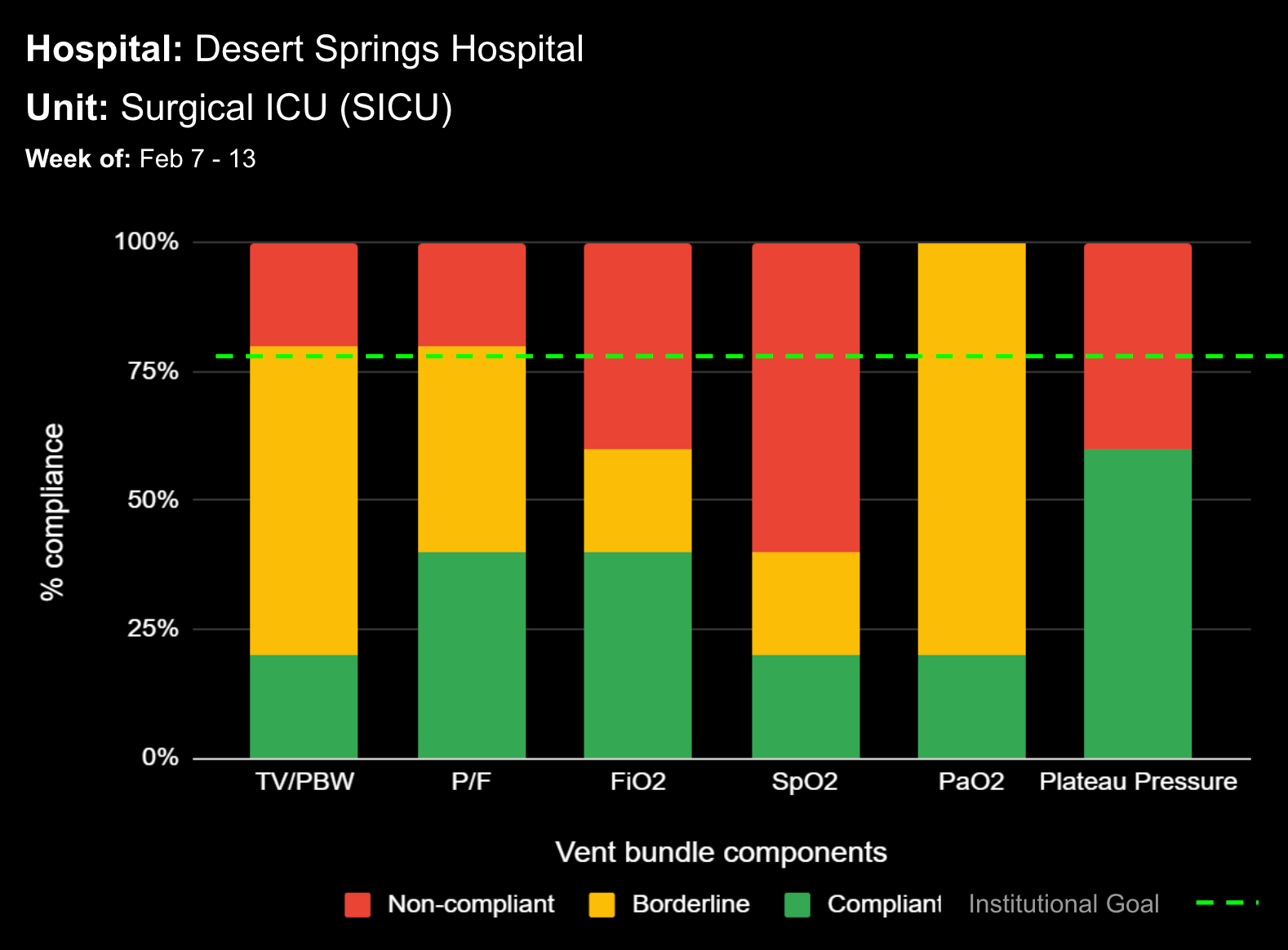
In a similar fashion, CDS systems can improve patient safety by identify impending adverse events. In addition to alerting a healthcare team to potential drug interactions or allergies, CDS systems can remind providers of relevant, patient-specific information when making treatment decisions. As most clinical teams are managing multiple patients, optimal CDS will monitor both the patient condition and their test results so that alerts or alarms can be sent when any abnormal laboratory results or vital sign indicates action is needed. Additionally, by integrating and analyzing data in real time, CDS systems can monitor all of the patients in the hospital, identify trends and patterns that may indicate an increased risk of adverse events, allowing healthcare providers or rapid response teams to take preventive measures before an adverse event occurs.
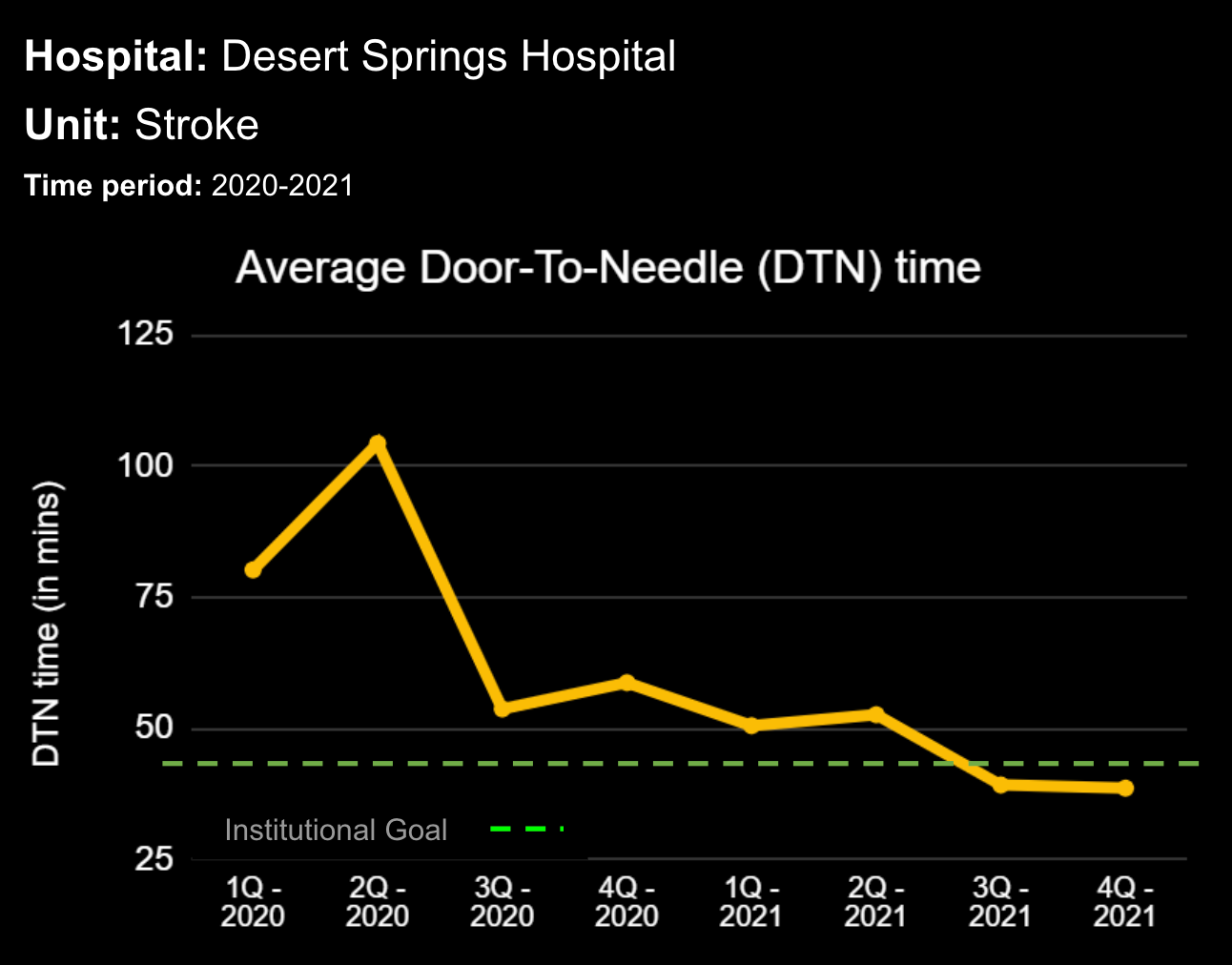
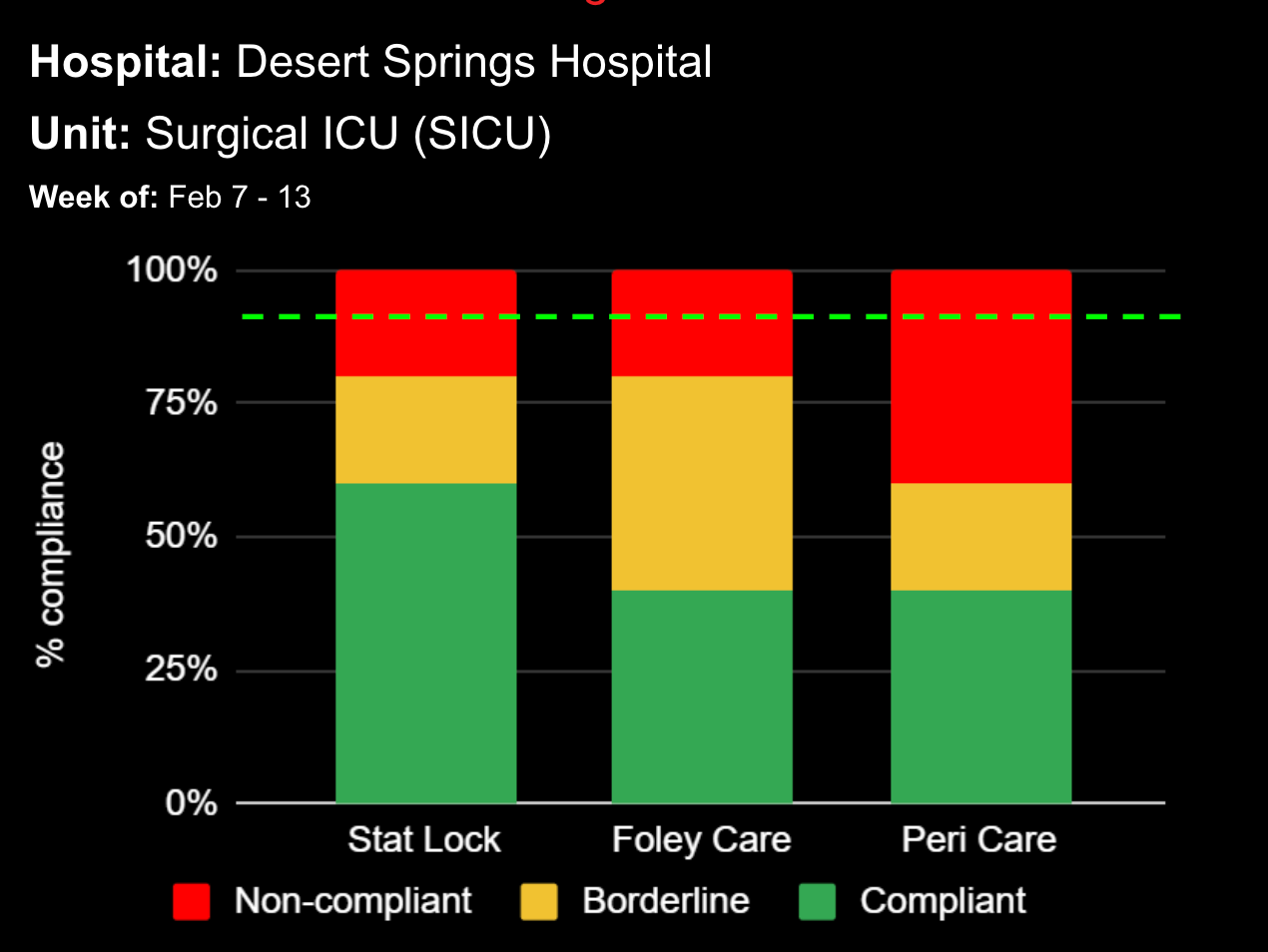
Most importantly, CDS systems can provide evidence-based guidelines and recommendations for clinical decision-making, promoting best practices that have been shown to reduce the risk of adverse events and improve patient outcomes. As medicine continues to evolve rapidly, appropriate guidelines and recommendations also continue to change. CDS helps providers comply with the latest medical guidelines, ensuring that the most appropriate care is provided. Additionally, use of a CDS to simplify presentation of data and calculate risk scores can improve patient safety by reducing the time before appropriate action is taken.
Most importantly, CDS can facilitate communication and collaboration among multidisciplinary healthcare teams and the patient. Improved and transparent communication can enable informed decisions. When integrated, real-time data is reviewed and discussed by all stakeholders, a more timely diagnoses can enable rapid and accurate treatments to be carried out. Further, many systems now seek to involve the patients and caregivers to build trust by promoting transparency of care and also making the patient feel like they are a part of the care team.
By providing healthcare providers with real-time patient-specific information, promoting evidence-based practices, and facilitating communication and collaboration, CDS systems can help avoid adverse events, improve patient safety, and ultimately improve patient outcomes.
References
- What is the Relationship between the HITECH, HIPAA and Electronic Medical Records? The HIPAA Journal [Website]. Published January 1, 2023. Available at: https://www.hipaajournal.com/relationship-between-hitech-hipaa-electronic-health-medical-records/
- Gold M, McLaughin C. Assessing HITECH Implementation and Lessons: 5 Years Later. Milbank Q. 2016;94(3):654-687. doi:10.1111/1468-0009.12214
- Mills S. Electronic Health Records and Use of Clinical Decision Support. Crit Care Nurs Clin North Am. 2019;31(2):125-131. doi:10.1016/j.cnc.2019.02.006
- Chertow GM, Lee J, Kuperman GJ, et al. Guided medication dosing for inpatients with renal insufficiency. JAMA. 2001;286(22):2839-2844. doi:10.1001/jama.286.22.2839
- Judge J, Field TS, DeFlorio M, et al. Prescribers’ responses to alerts during medication ordering in the long term care setting. J Am Med Inform Assoc. 2006;13(4):385-390. doi:10.1197/jamia.M1945
Learn more About How we help clinicians improve patient outcomes
Schedule a call with our team to discuss how we are helping our clients revolutionize how clinicians manage patient interventions.