05 Jun Understanding Maternal Sepsis and Best Practices for Management

Understanding Maternal Sepsis and Best Practices for Management
Maternal sepsis is a severe infection that poses significant risks to both the mother and the fetus. It remains a leading cause of maternal mortality globally, particularly in low-resource settings. Effective management is crucial for improving outcomes. Studies have shown that the incidence of maternal sepsis ranges between 0.1% and 0.4% of pregnancies, depending on the setting (Hensley et al., 2019); (Admon et al., 2019). Notably, it is estimated that 63% of maternal deaths from sepsis are preventable with timely recognition and appropriate management (CMQCC, 2021).
Causes of Maternal Sepsis
Maternal sepsis is typically caused by bacterial infections, although viral and fungal infections can also be culprits. The common sources of infection include:
- Urinary Tract Infections (UTIs): UTIs are common during pregnancy and can progress to pyelonephritis, which can lead to sepsis if untreated.
- Chorioamnionitis: This infection of the fetal membranes (chorion and amnion) typically occurs during labor and can lead to maternal and neonatal sepsis.
- Postpartum Infections: Infections of the uterine lining (endometritis) after childbirth, particularly following cesarean sections, are a significant cause of maternal sepsis.
- Surgical Site Infections: Infections at the site of a cesarean section or episiotomy can develop into sepsis if not properly managed.
- Pneumonia: Respiratory infections such as pneumonia can become severe in pregnant women due to changes in the immune system and decreased lung volume from the growing baby. These changes can compromise the body’s ability to fight off infections effectively, potentially leading to sepsis.
- Influenza: Pregnant women are at higher risk of severe flu complications, which can include secondary bacterial infections leading to sepsis (Sepsis Alliance, 2020); (End Sepsis, 2021).
Pregnant women are more susceptible to sepsis due to immunological changes, the need for procedures or surgery, and complications such as premature rupture of membranes or gestational diabetes (Sepsis Trust, 2020).
Impact on Fetal Health
Maternal sepsis significantly impacts fetal health, with increased risks of neonatal complications, including neonatal shock and sepsis. The incidence of maternal sepsis is relatively low, but the impact on fetal outcomes can be severe, with complications such as preterm birth, low birth weight, and increased neonatal mortality (Ozarslan et al., 2023).
Ensuring maternal hemodynamic stability, adequate oxygenation, and effective infection control are crucial for optimizing fetal outcomes during maternal sepsis(Chau & Tsen, 2014). Technological advancements, such as continuous fetal monitoring and clinical decision support tools, can help in timely intervention and improving both maternal and fetal prognosis.
Impact on Maternal Health
Maternal sepsis can have devastating effects on the mother, leading to severe complications such as organ failure, septic shock, and even death. The physiological changes during pregnancy can mask the early signs of sepsis, making timely diagnosis challenging. Early and aggressive treatment is essential to prevent the progression of sepsis to severe sepsis and septic shock. Studies indicate that approximately 0.1% of pregnancies are affected by maternal sepsis, with significant morbidity and mortality associated with delayed treatment (Acosta et al., 2013); (Zhong et al., 2022).
Maternal sepsis is the second leading cause of mortality in obstetric patients and is responsible for at least five percent of maternal intensive care unit admissions in the United States (Sundin et al., 2021). It accounts for approximately 10.7% of all maternal deaths globally (Firoz & Woodd, 2017). Effective management includes prompt antibiotic administration, fluid resuscitation, and source control. Multidisciplinary care involving obstetricians, anesthetists, and critical care specialists is crucial for managing complex cases and improving outcomes (Lloyd & Bell, 2020).
Importance of Early Recognition and Intervention
Timely diagnosis and intervention are critical in reducing maternal sepsis-related mortality. Early recognition involves vigilance for signs and symptoms of sepsis, which can be subtle and easily masked by the physiological changes of pregnancy. Key signs include fever, increased heart rate, and abnormal white blood cell count. Early identification allows for prompt treatment, which is essential for improving outcomes (Shields et al., 2021); (Shields et al., 2021).
Critical Management Strategies
Management of maternal sepsis includes several critical components:
- Antibiotic Therapy: Initiating broad-spectrum antibiotics within the first hour of recognizing sepsis is crucial. Delays in antibiotic administration can significantly increase mortality rates (Foeller & Gibbs, 2019).
- Fluid Resuscitation: In cases of sepsis-induced hypoperfusion, rapid fluid resuscitation helps maintain blood pressure and organ perfusion. This intervention should be started immediately upon diagnosis (Barclay et al., 2016).
- Source Control: Identifying and managing the source of infection is paramount. This may involve surgical intervention or other procedures to remove infected tissue or drain abscesses (Lissauer et al., 2019).
- Multidisciplinary Approach: Management of maternal sepsis often requires a coordinated effort from a multidisciplinary team, including obstetricians, anesthetists, and critical care specialists. This approach ensures comprehensive care and improves patient outcomes (Lloyd & Bell, 2020).
Role of Decision Support Tools
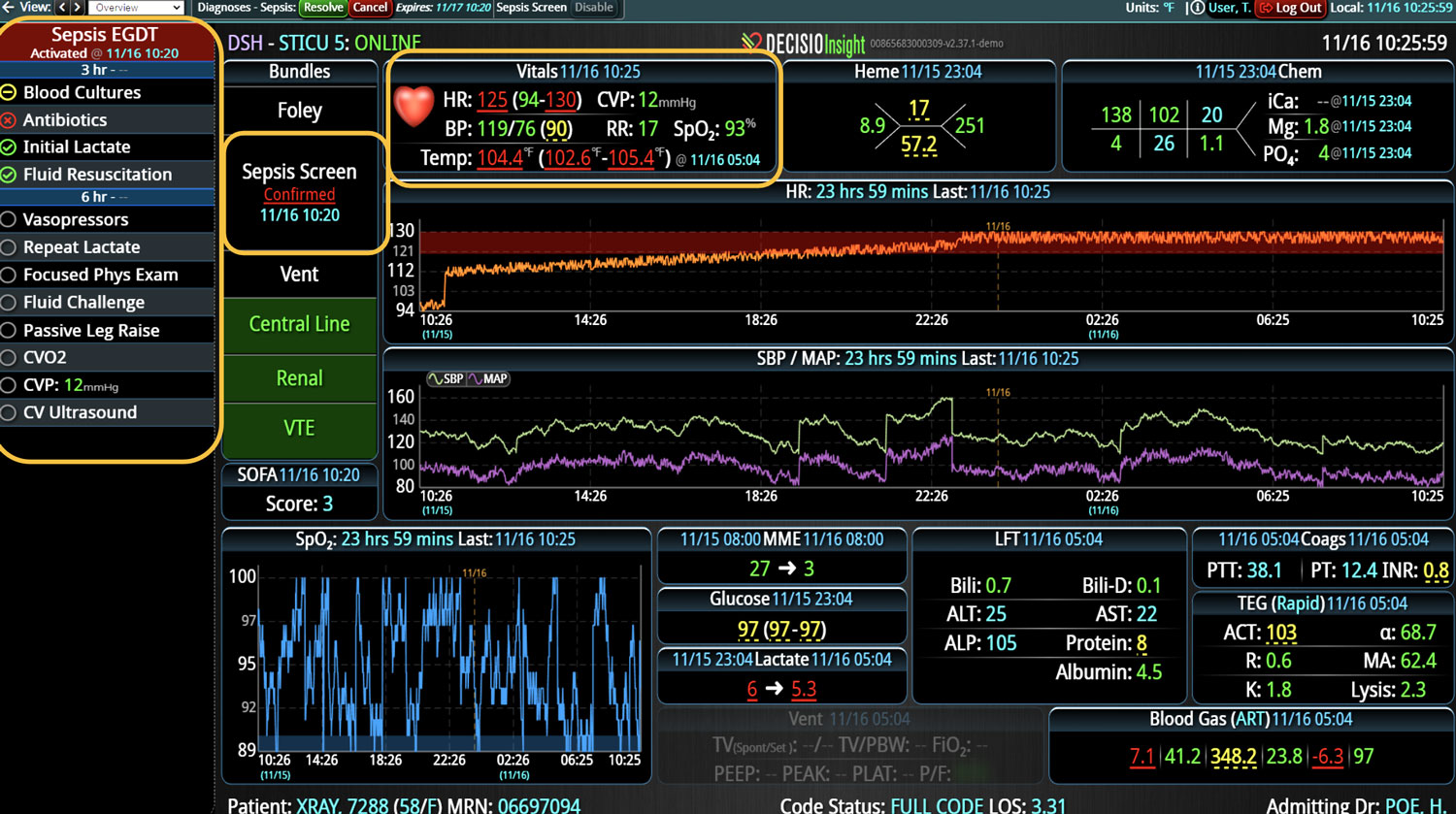
Decision support tools, such as the Sepsis in Obstetrics Score, are crucial in identifying and managing maternal sepsis. These tools help clinicians recognize early signs of deterioration in obstetric patients and provide a systematic approach to treatment. The Sepsis in Obstetrics Score model, for instance, identifies the risk of morbidity from sepsis in pregnant women and ensures that high-risk patients receive appropriate care (Albright et al., 2015).
Bedside Assessment Tools
Bedside assessment tools are essential in the early detection of maternal sepsis, which can be challenging due to the normal physiological changes of pregnancy masking the signs and symptoms of sepsis. Commonly used tools include:
- Modified Obstetrics Early Warning Screen (MEOWS): This tool was piloted to detect sepsis in maternal patients and proved effective in a quality improvement pilot at an academic tertiary care center ([Abo-zed et al., 2023](Abo-zed et al., 2023)).
- Sepsis Screening Tools: Implementation of sepsis screening tools has been shown to increase nurses’ awareness and recognition of maternal sepsis, leading to improved knowledge and empowerment in making recommendations for patient care (Lu et al., 2019).
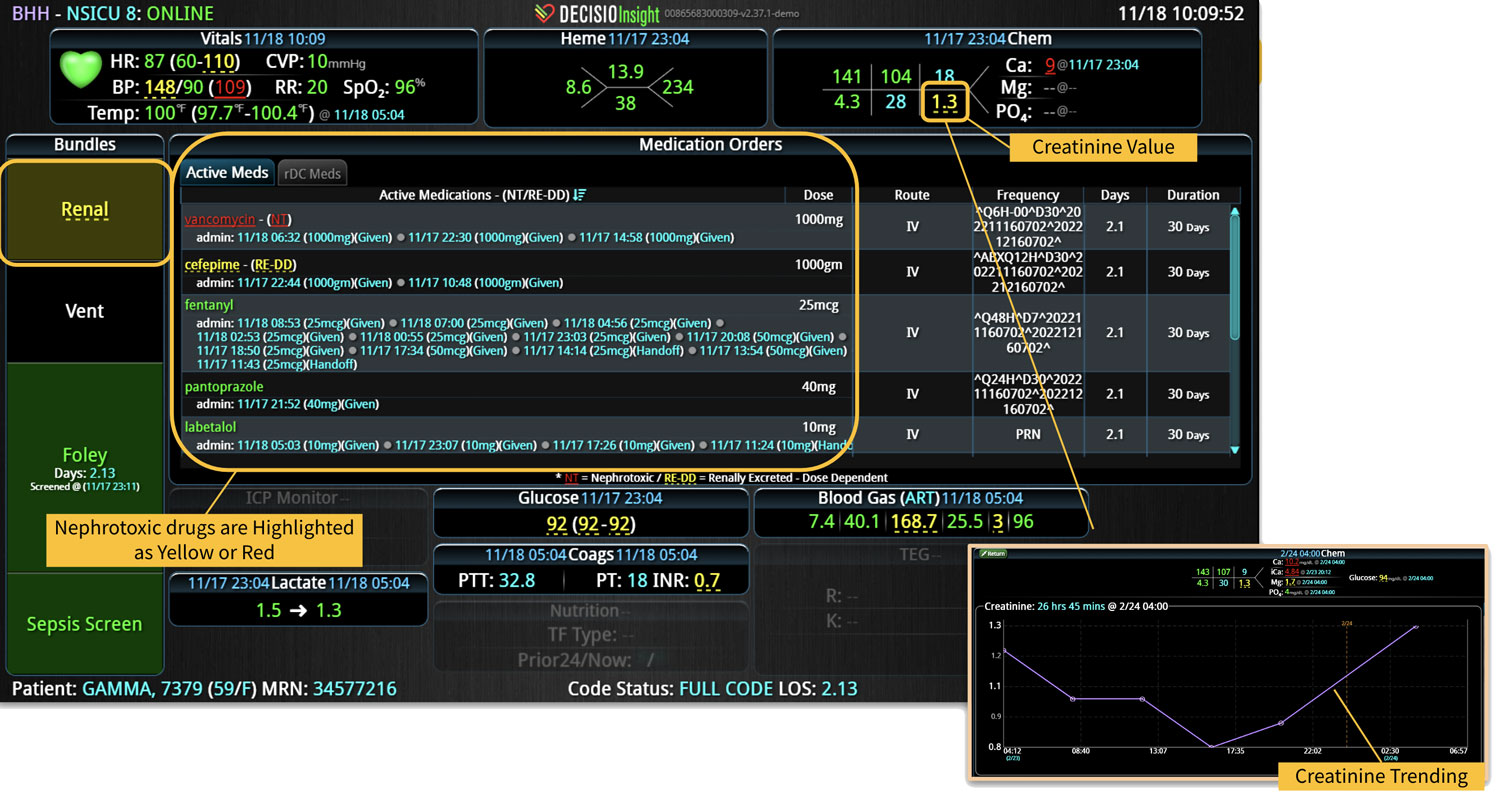
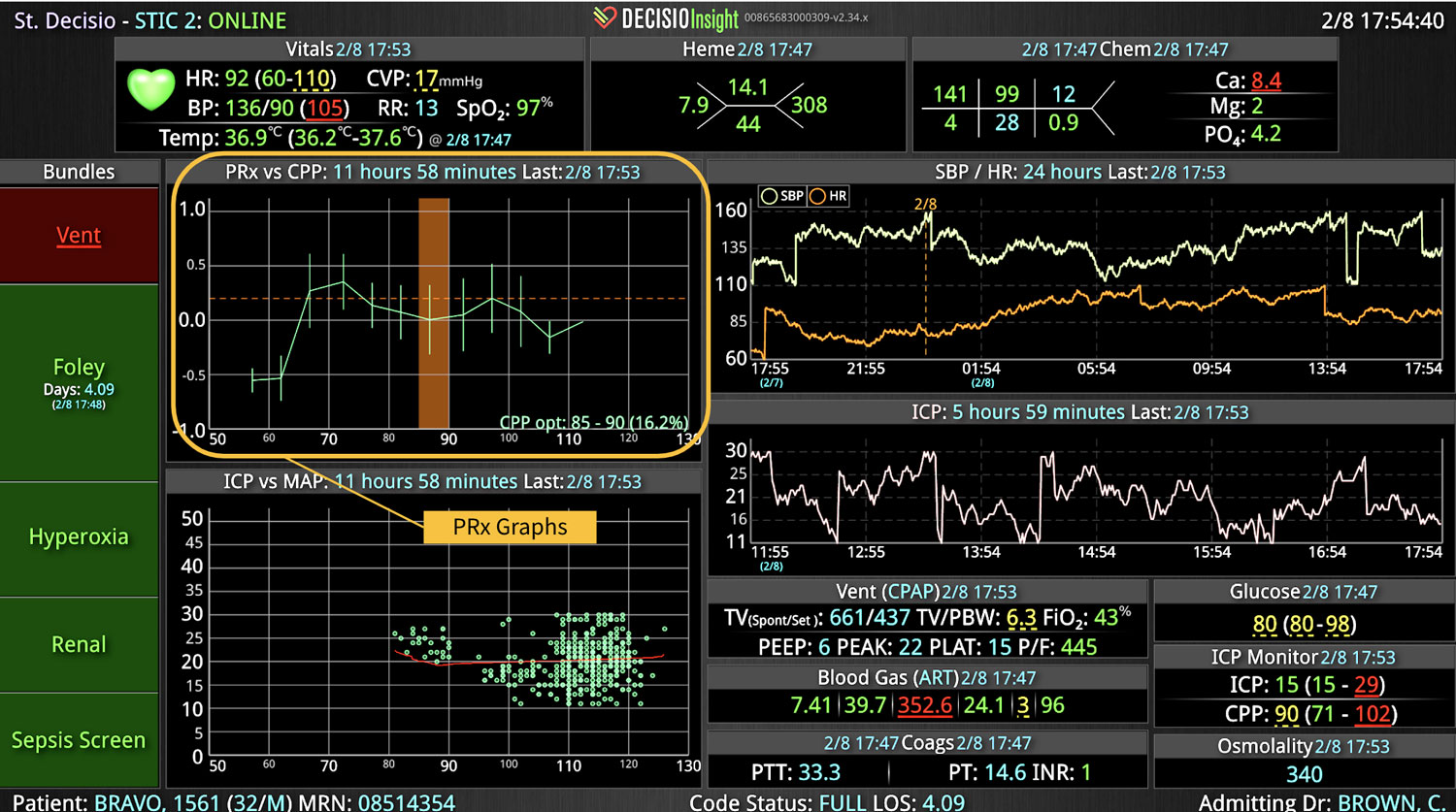
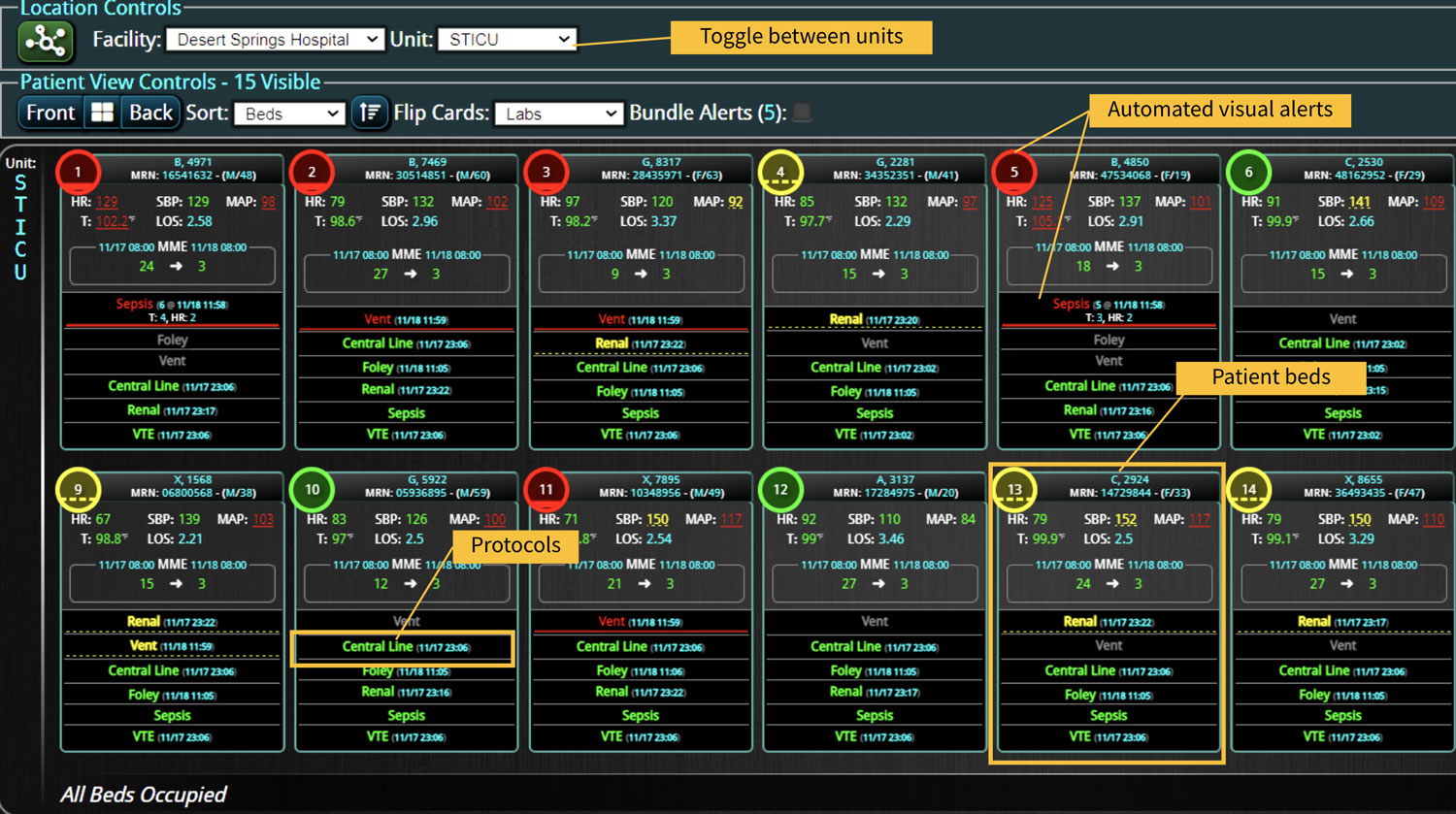
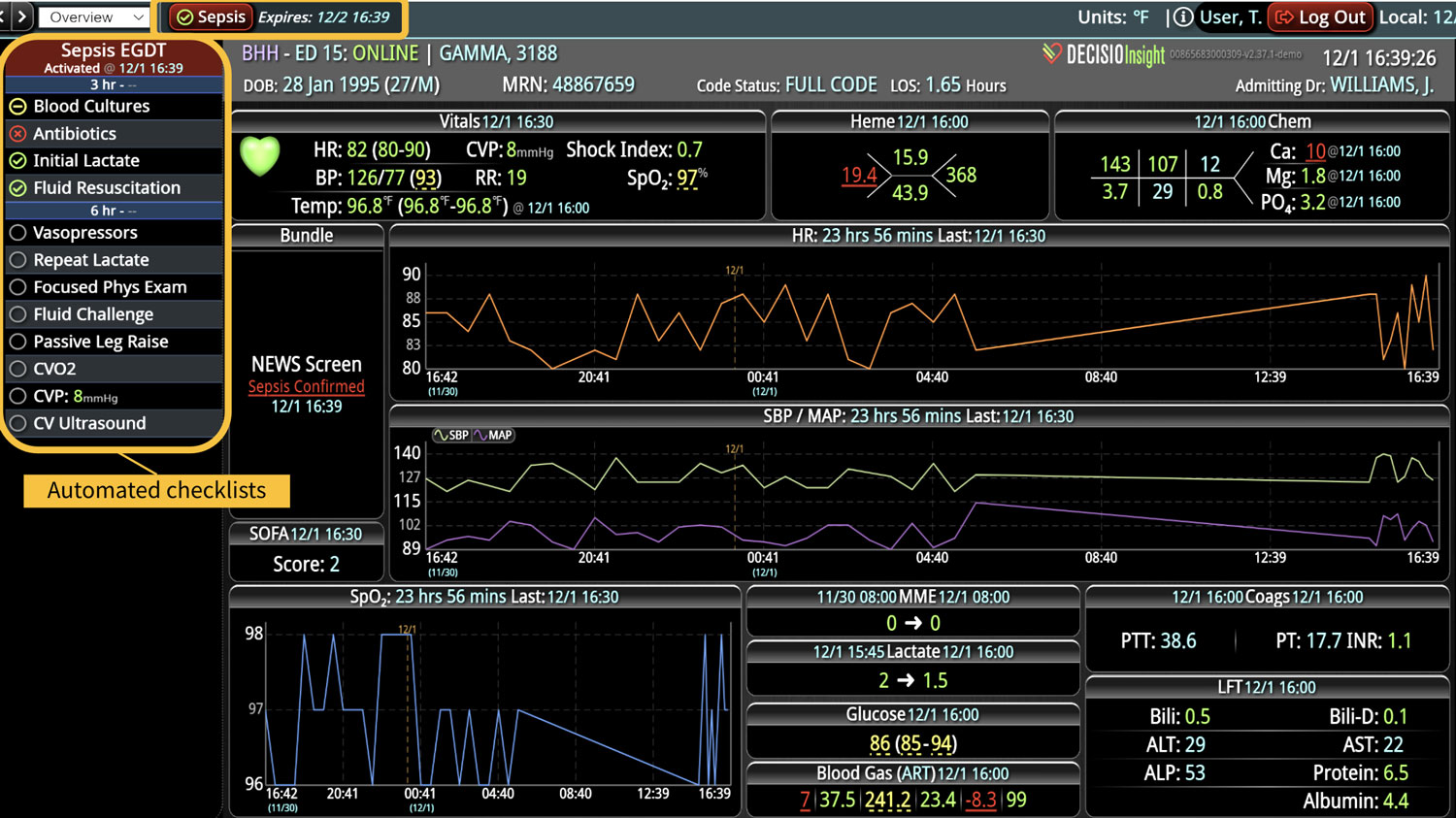
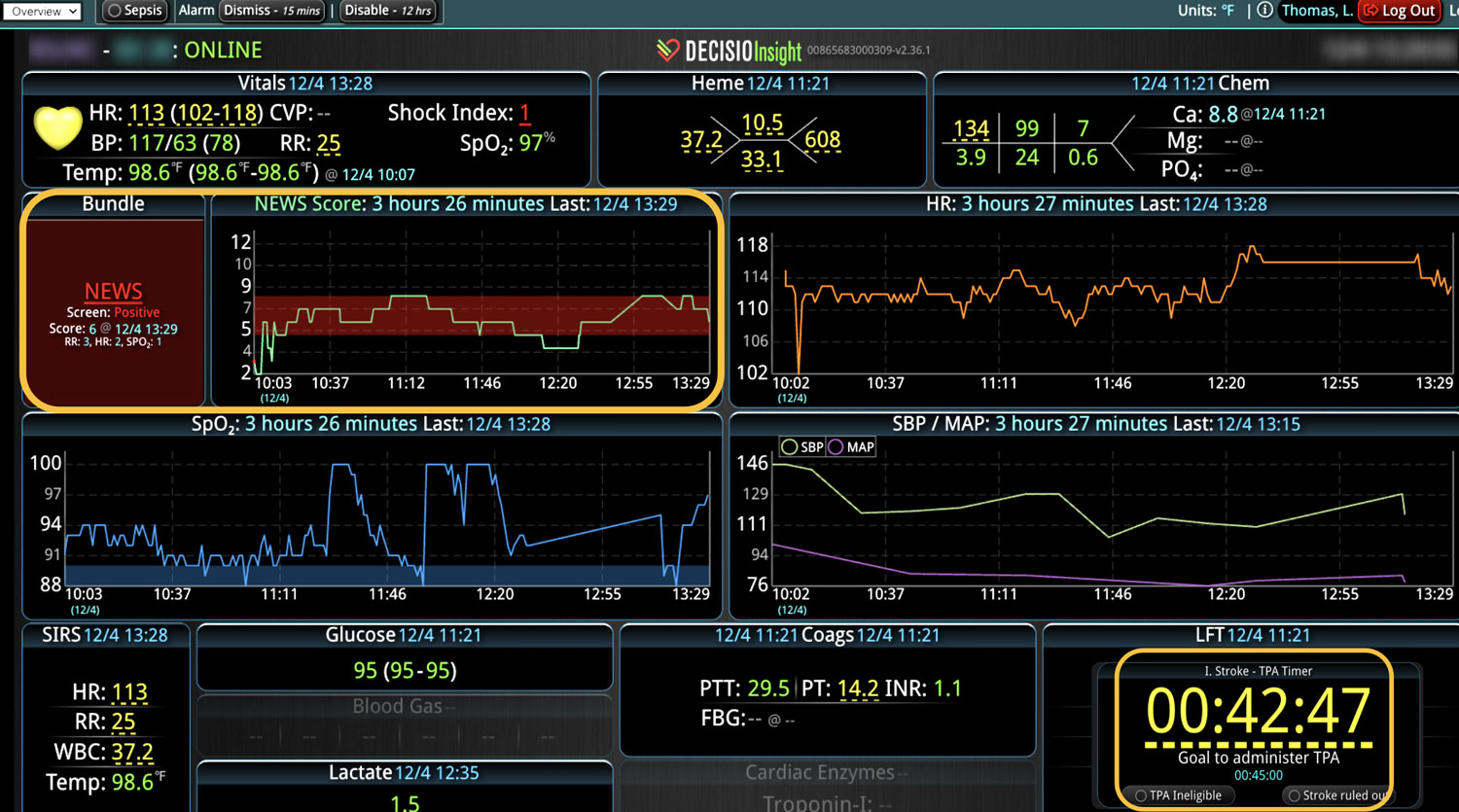
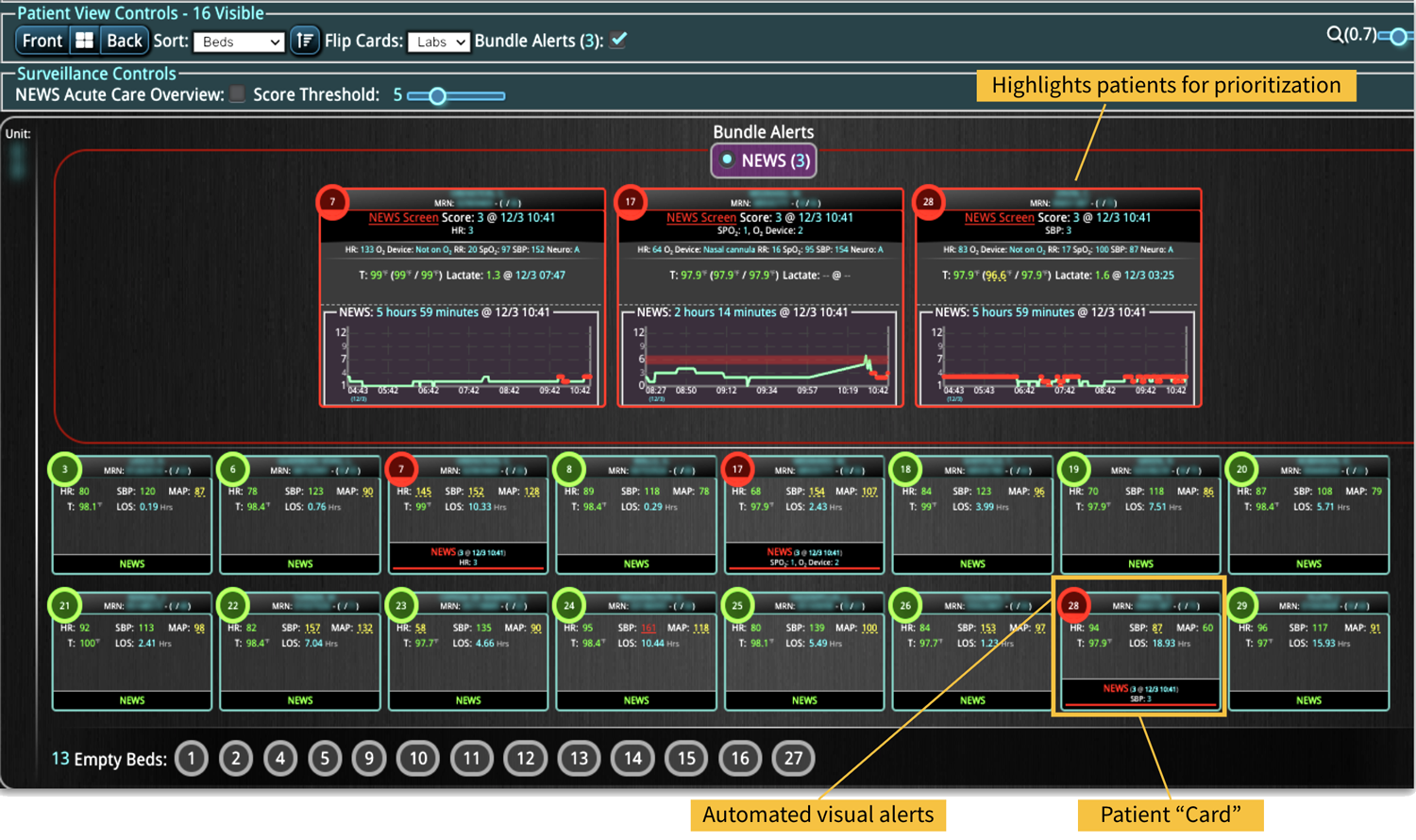
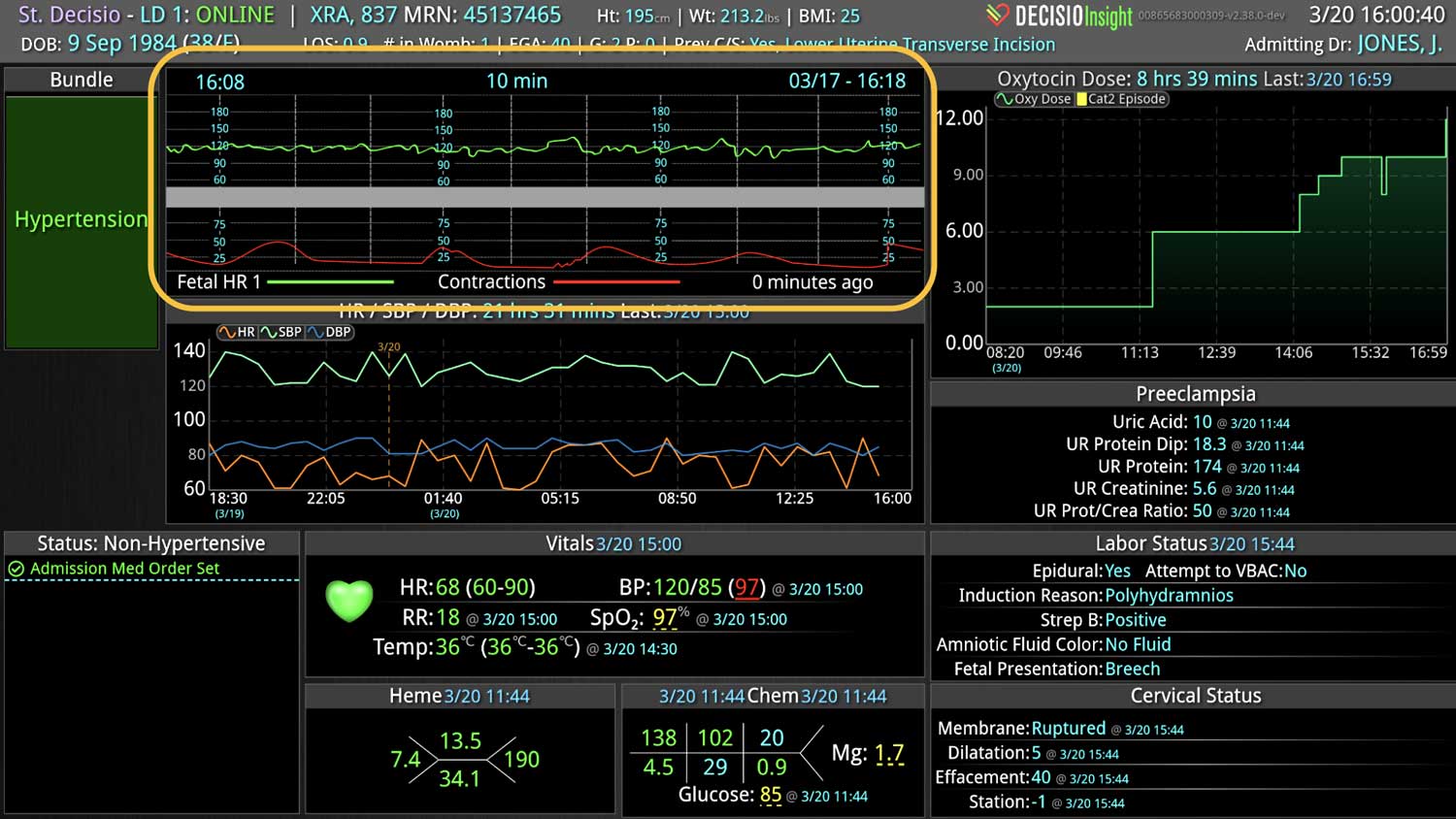
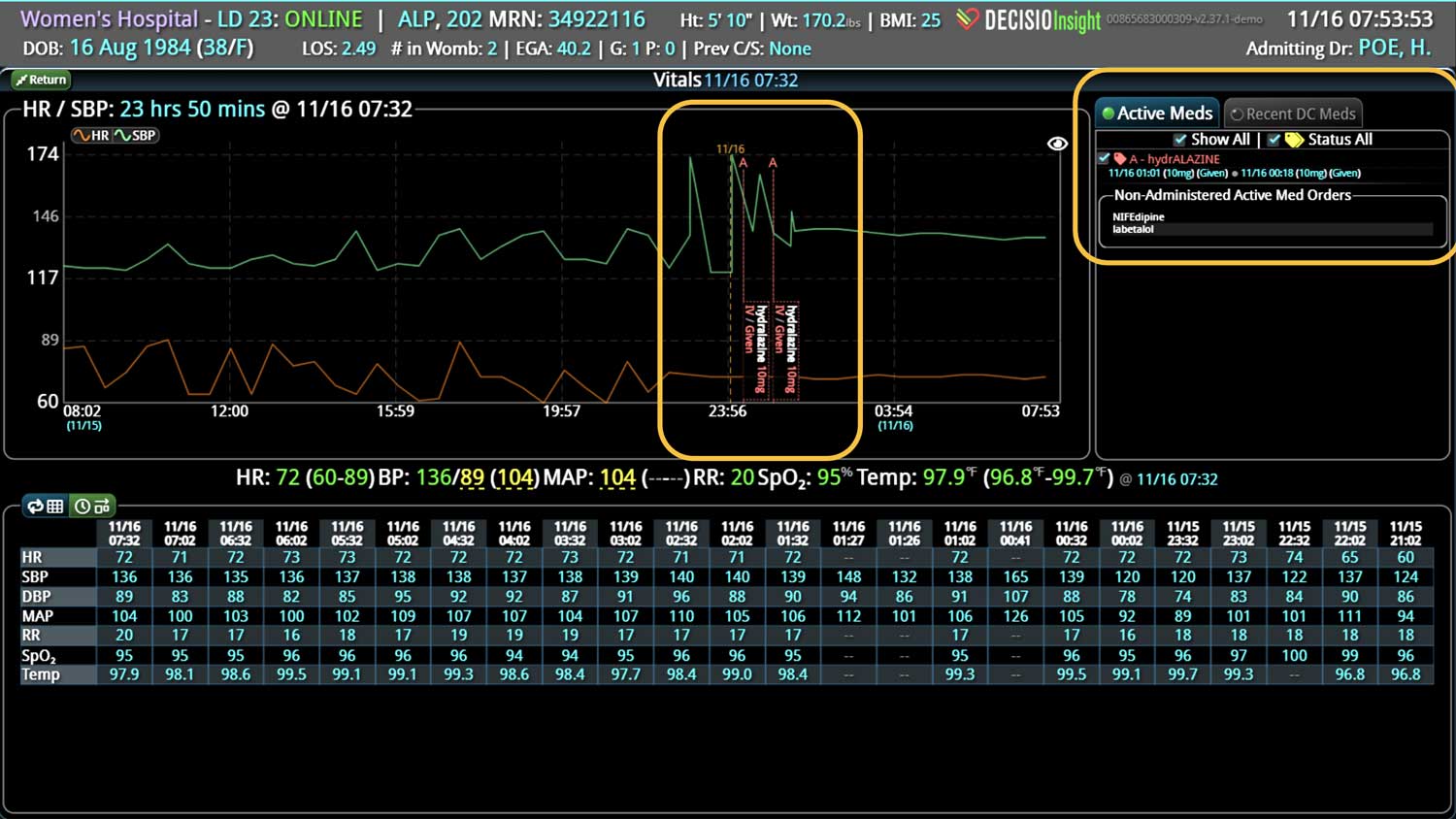
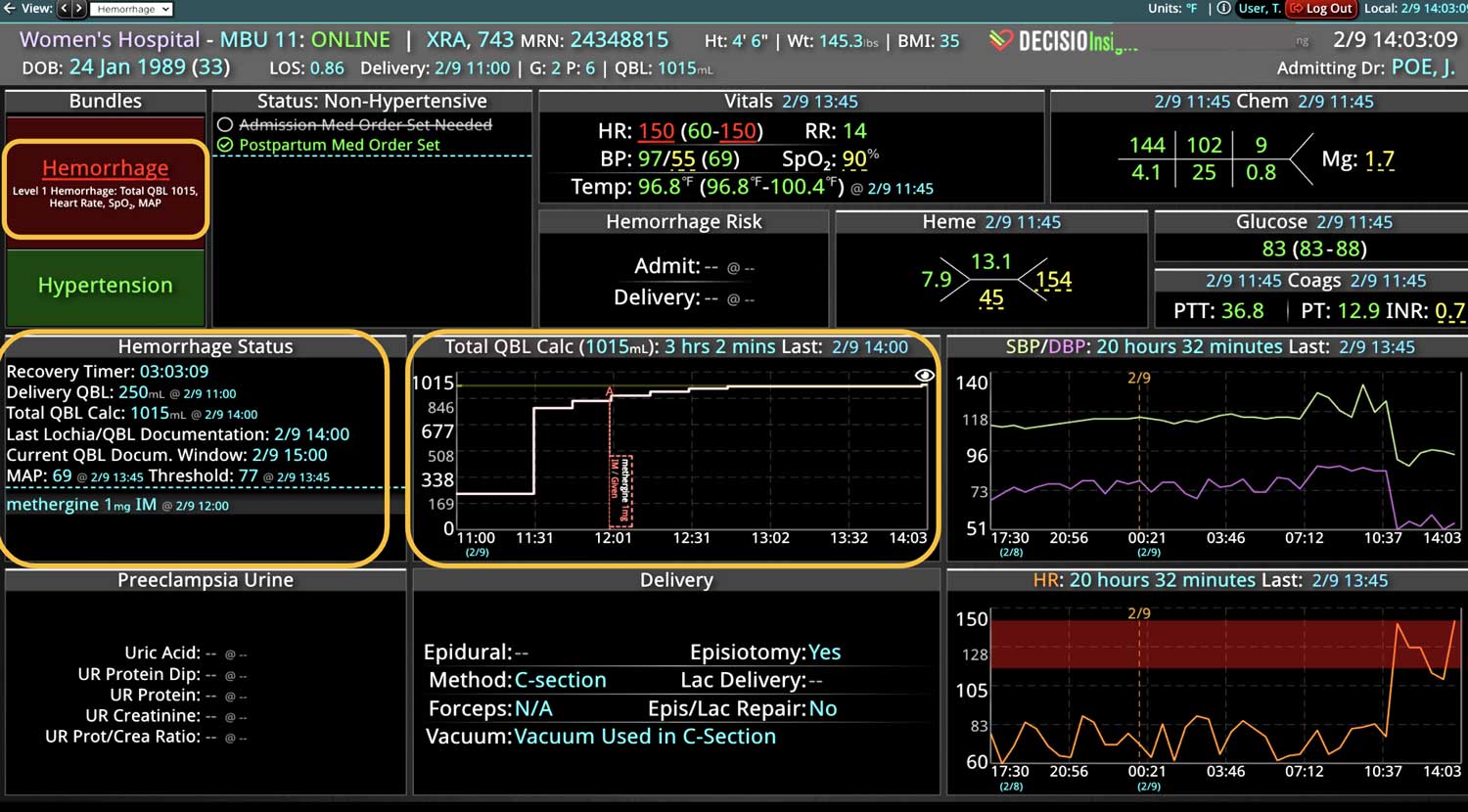
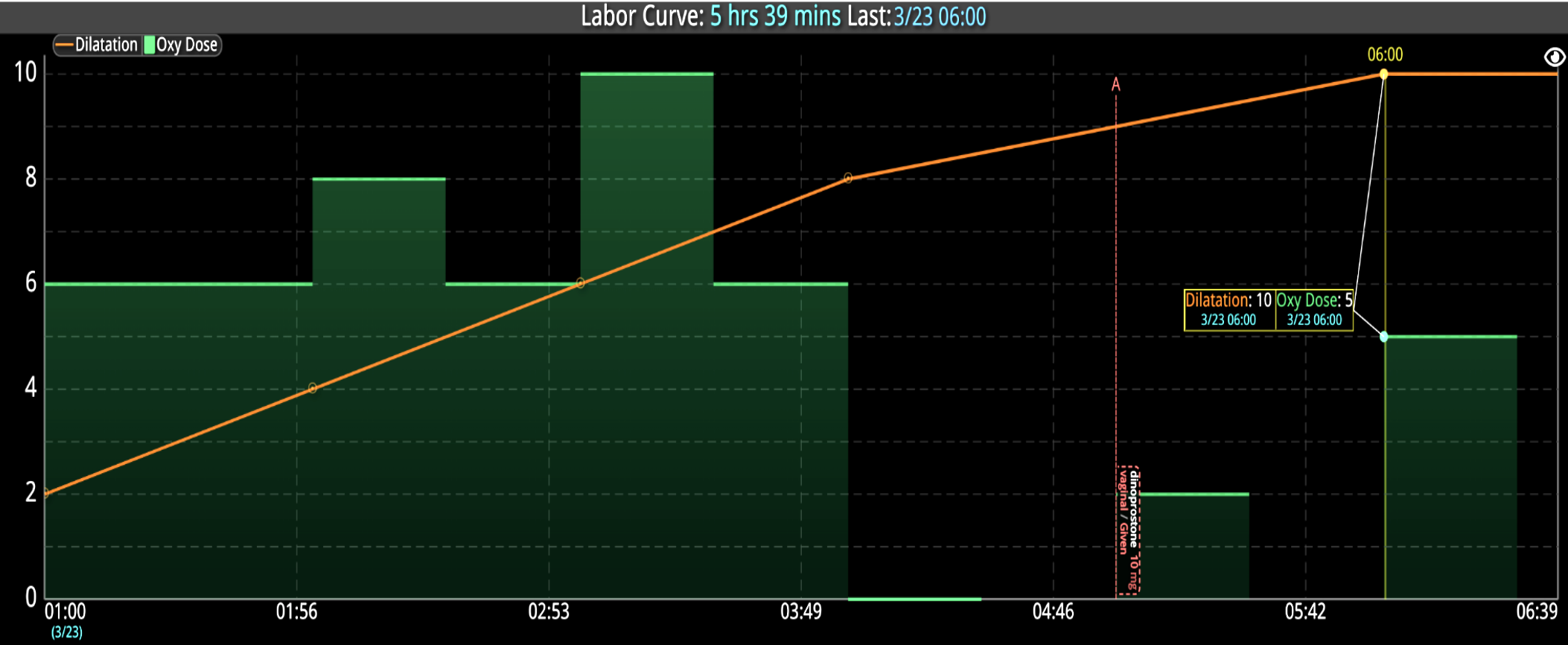
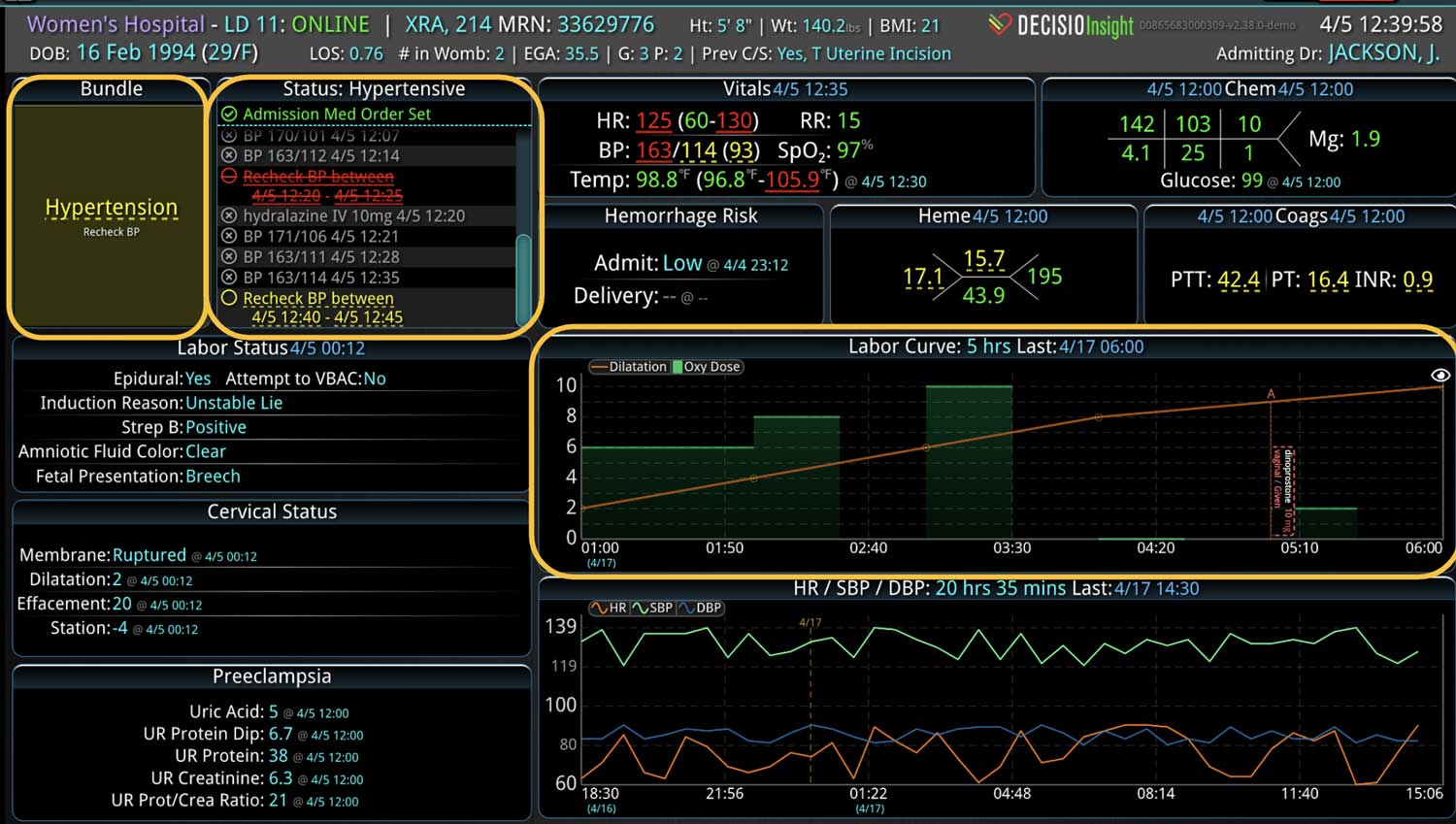
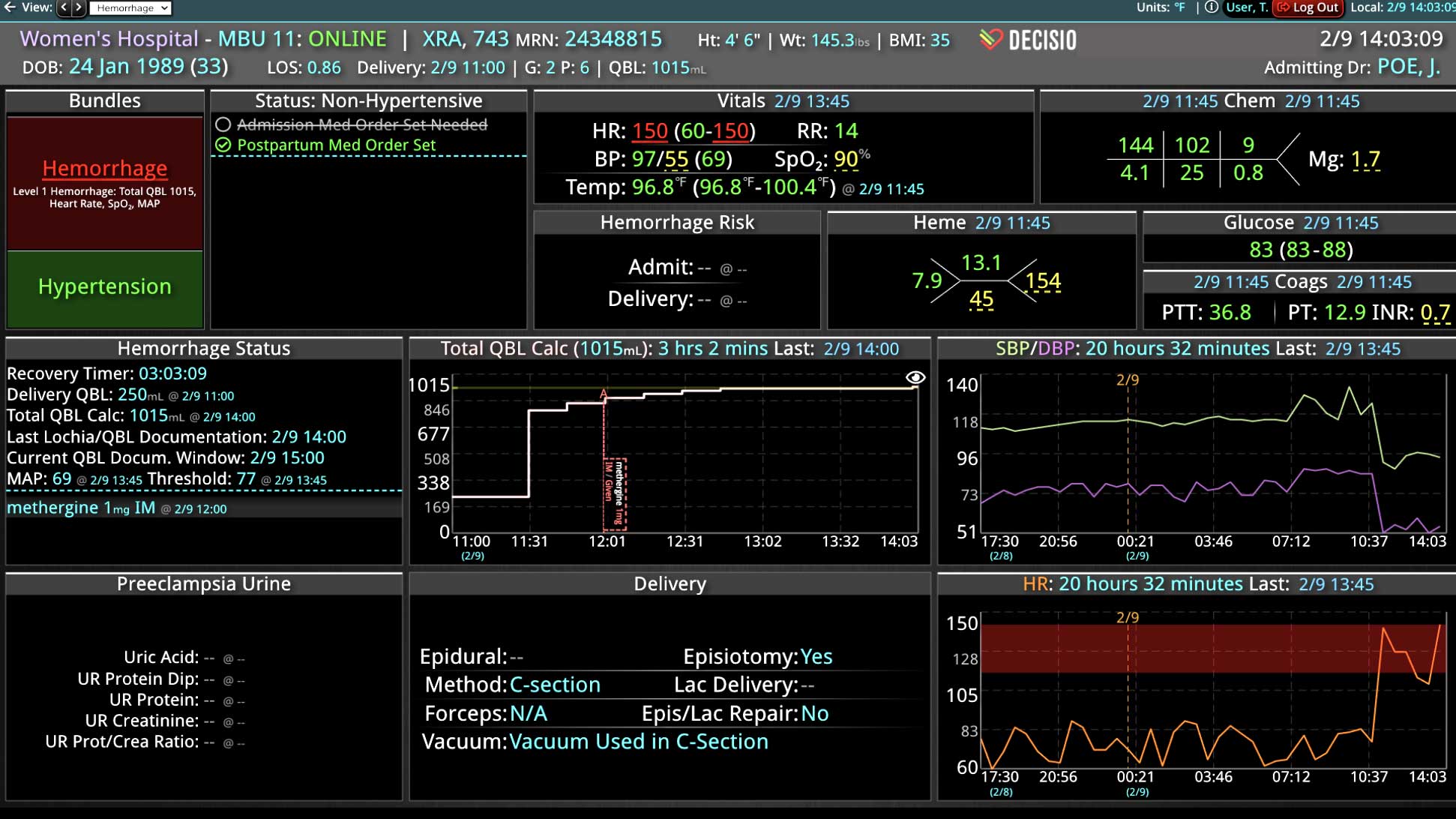
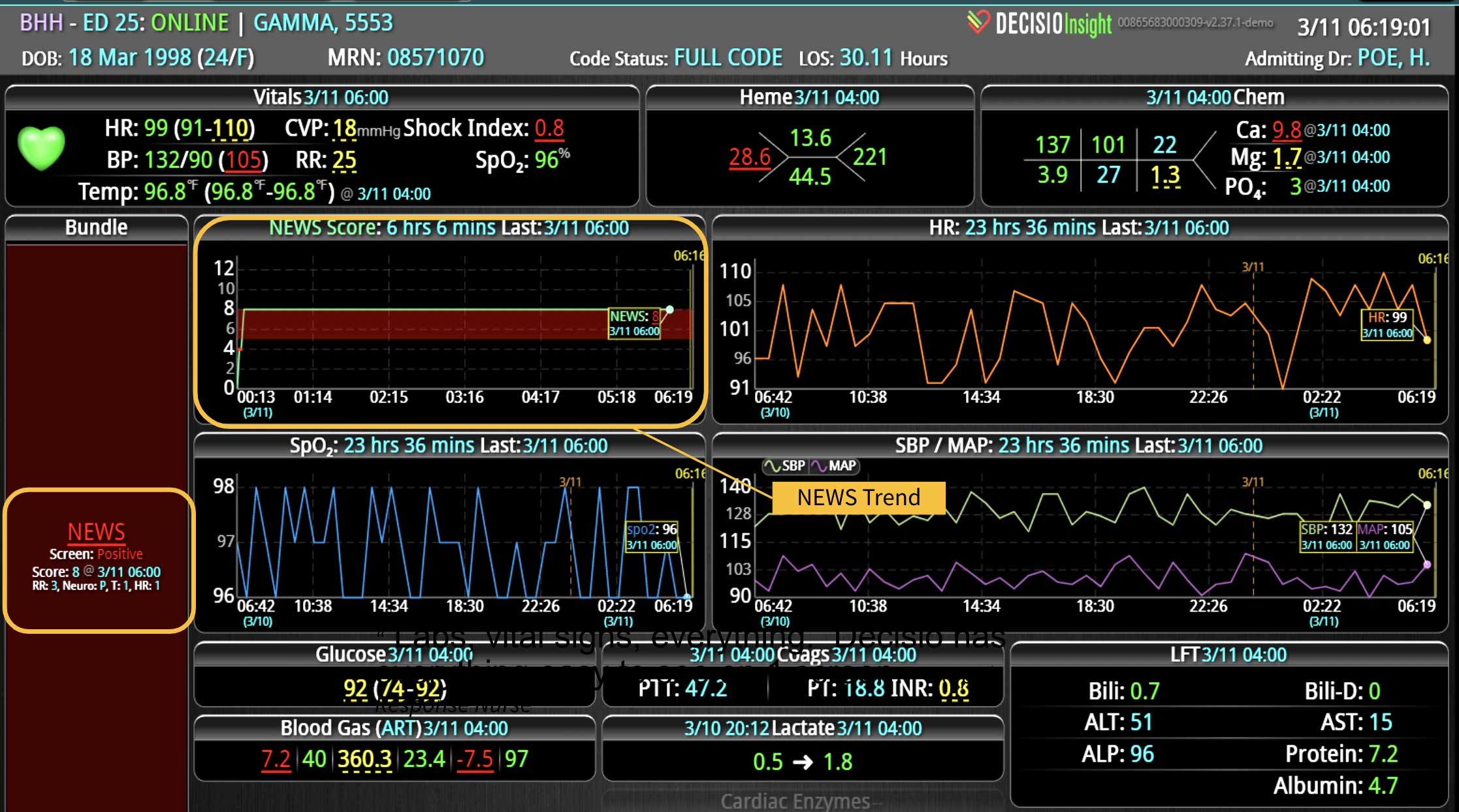
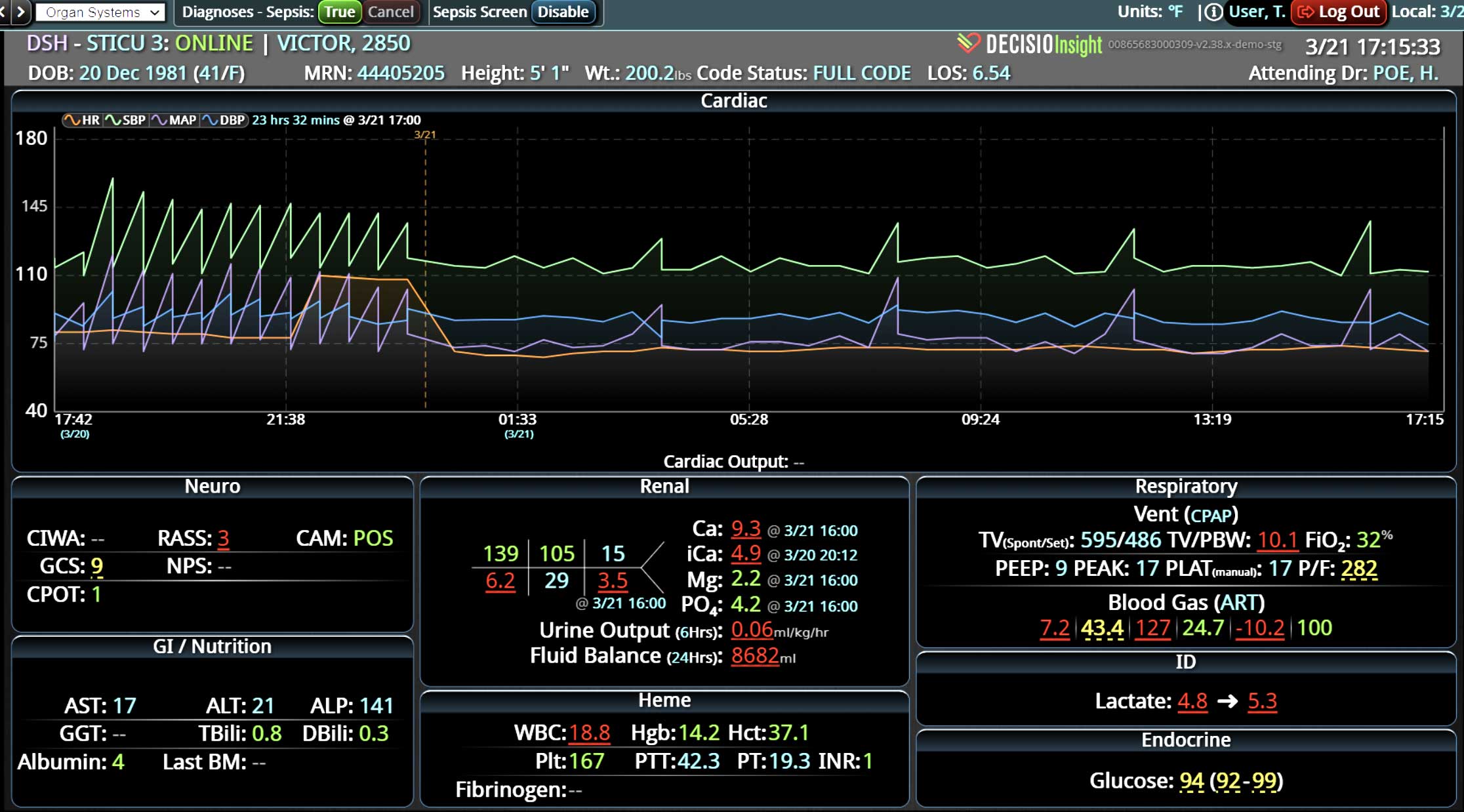
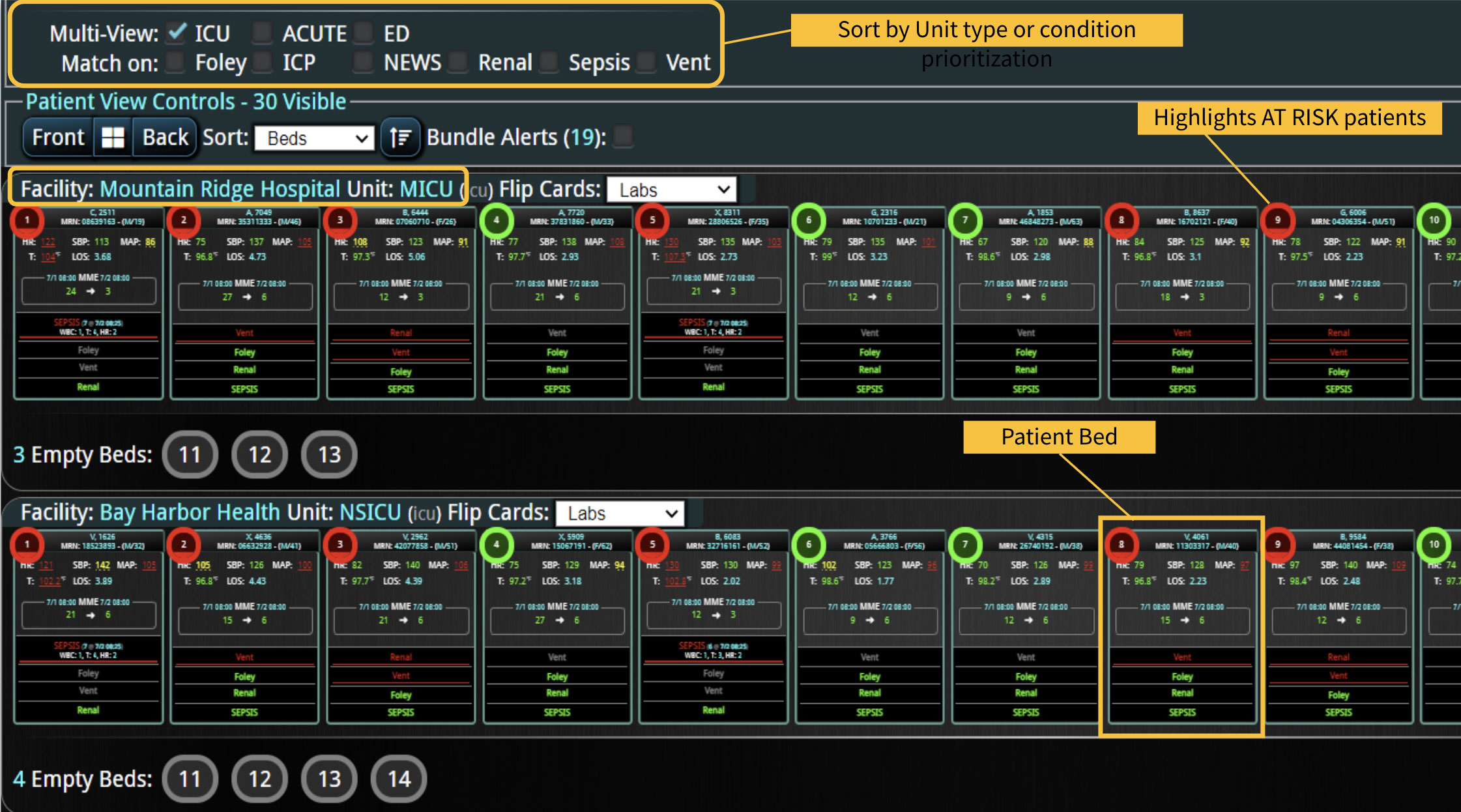
Additionally, Decisio Health’s platform, Decisio, enhances the monitoring and treatment of maternal sepsis by providing a near real-time clinical surveillance system that improves both the speed and quality of care. Here’s how Decisio supports the management of maternal sepsis:
- Near real-time Data Integration: It integrates data from diverse sources within a hospital, such as EHRs, lab results, and monitoring equipment, offering a comprehensive view of a patient’s health status crucial for early sepsis detection.
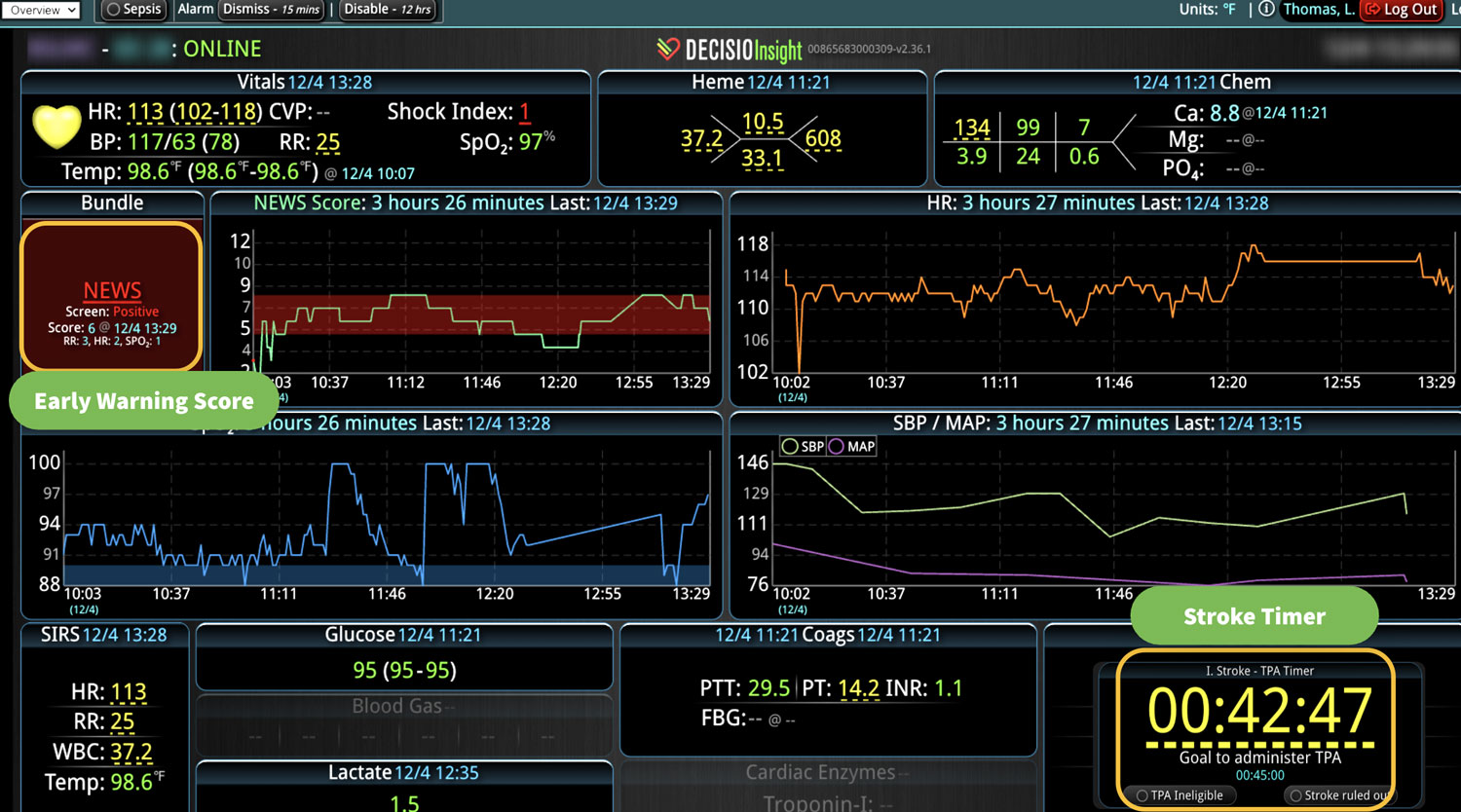
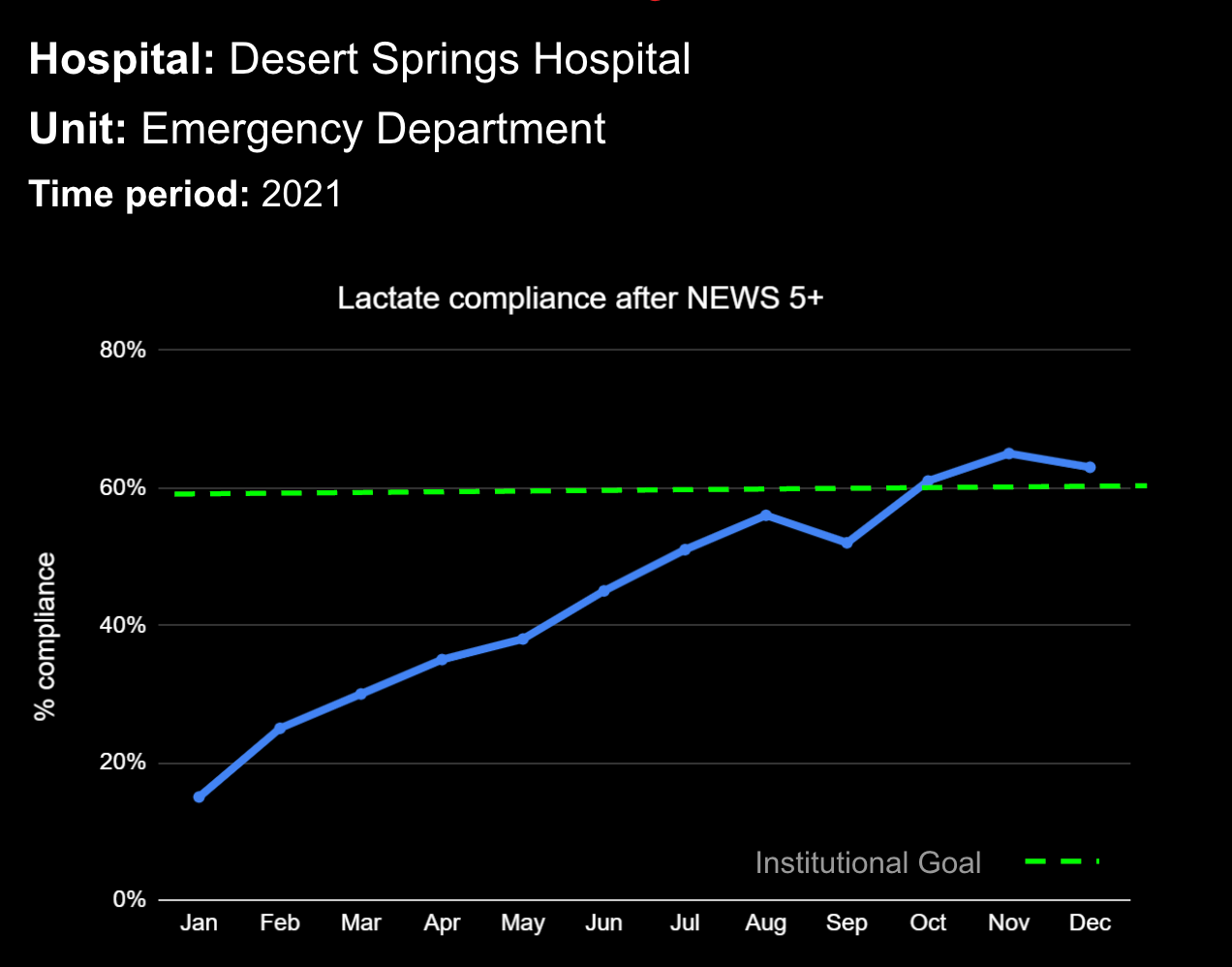
- Early Warning Scores: The system employs early warning scores tailored for detecting signs of sepsis, alerting healthcare providers to subtle changes in a patient’s condition that may indicate the onset of sepsis and facilitating early intervention.
- Clinical Decision Support: Decisio provides decision support tools that aid clinicians in adhering to best practice protocols for sepsis management, including timely administration of antibiotics and fluid resuscitation.
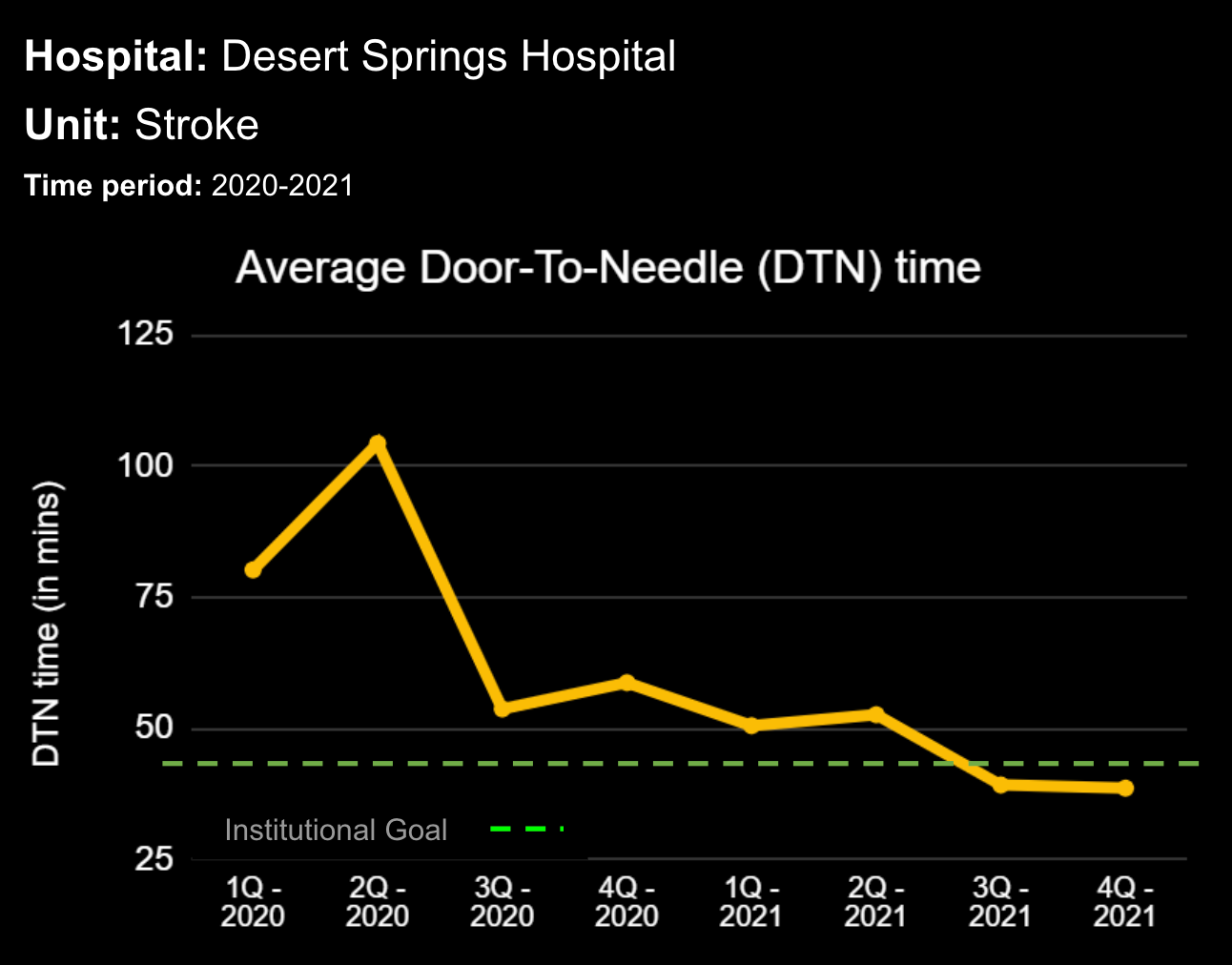
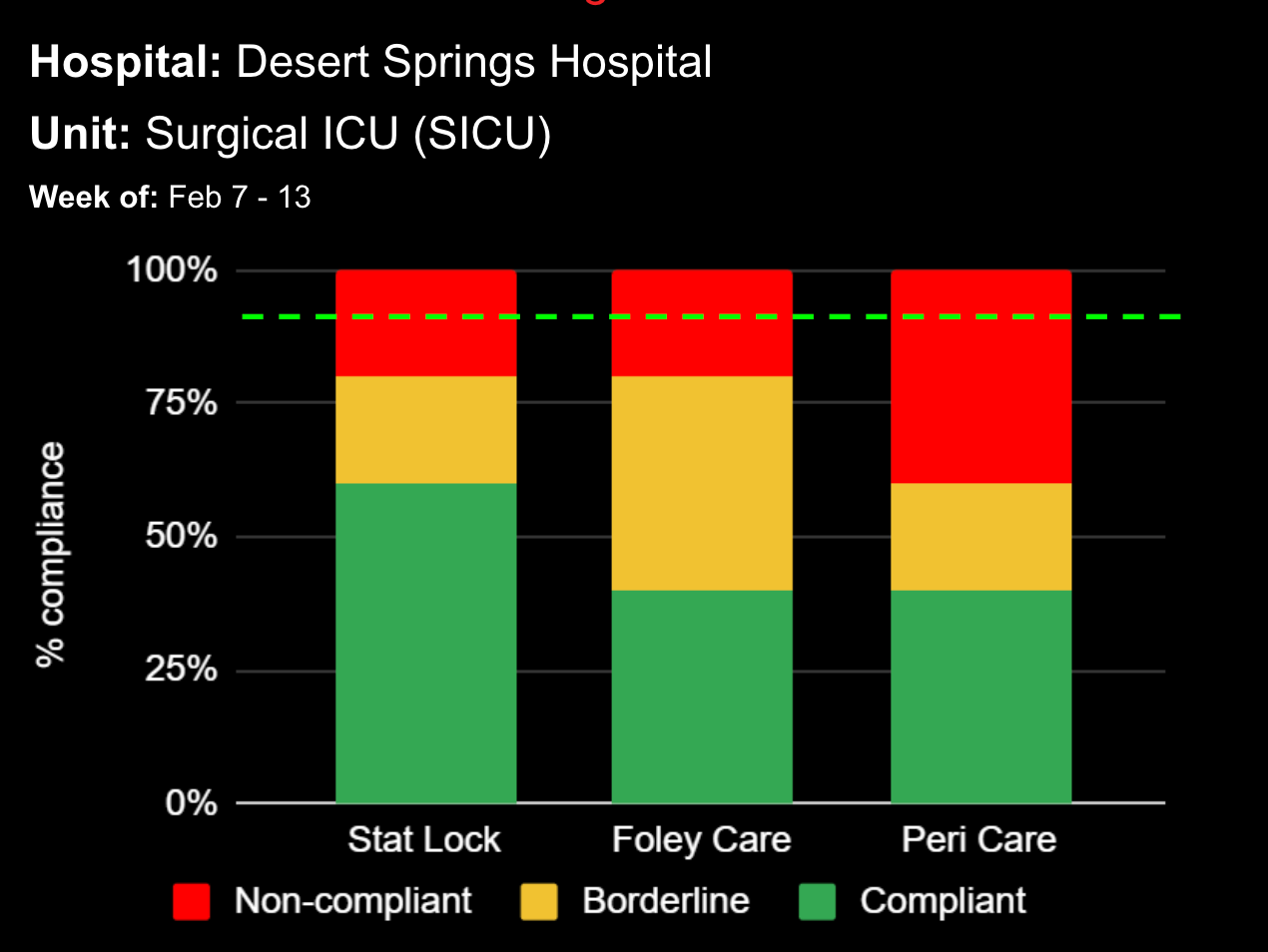
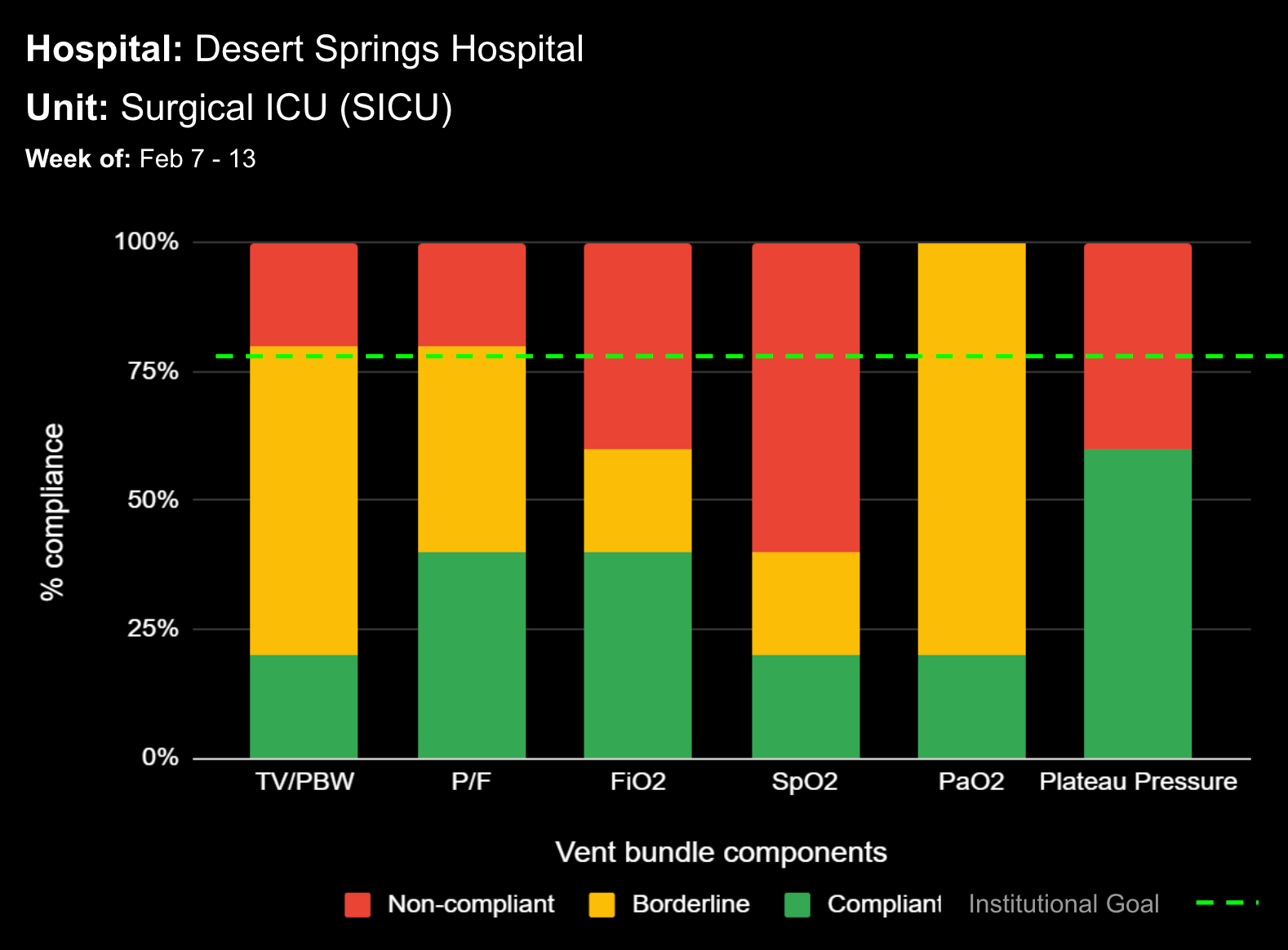
- Visualization Tools: The platform presents data in an easily digestible format using dashboards and visual alerts, helping clinicians quickly understand complex information and make informed decisions swiftly.
- Communication and Coordination: By offering a central point of access to near real-time patient data, Decisio improves communication and coordination among the healthcare team, which is crucial in a fast-paced environment like maternal care.
- Data Analytics and Reporting: The platform also provides analytics tools that allow healthcare institutions to analyze trends in sepsis cases, evaluate the effectiveness of protocols, and identify areas for improvement in patient care.
These tools and systems collectively enhance the ability to detect and manage maternal sepsis effectively, ultimately improving patient outcomes.
Additional Strategies and Resources
- Improving Diagnosis and Treatment Toolkit: The California Maternal Quality Care Collaborative (CMQCC) has developed a comprehensive toolkit that includes a two-step screening and confirmation process to more accurately diagnose and treat maternal sepsis (CMQCC, 2021).
- Preventative Measures: Preventative strategies include up-to-date vaccinations, especially flu vaccines, practicing good hygiene, and ensuring clean birthing practices. Pregnant women should seek immediate medical attention if they suspect an infection (Sepsis Alliance, 2020).
- Support for Survivors: Recovery from sepsis can be challenging. Support resources are available for survivors and their families, providing guidance and assistance during the recovery process (Sepsis Trust, 2020).
Conclusion
Maternal sepsis remains a significant challenge, but early recognition and timely intervention are key to improving outcomes. Bedside assessment tools and decision support systems play a crucial role in ensuring prompt and effective treatment, ultimately saving lives and improving both maternal and fetal health.
Learn more About How we help clinicians improve patient outcomes
Schedule a call with our team to discuss how we are helping our clients revolutionize how clinicians manage patient interventions.