13 Dec Is the hospital-at-home model the future of healthcare?

Is the hospital-at-home model the future of healthcare?
The pandemic served as a catalyst for change and innovation in the digital health world and at-home care. The combination of telehealth and hospital-at-home (HaH) services will have lasting positive effects but requires comprehensive and proactive remote technology to provide quality care to patients. With the advancement of technology, more hospitals and physician teams are adopting the HaH model. However, many may ask if it is safe and effective. Thus, we seek to review the latest research on the impact of this healthcare model on patients and policy.
What does acute health care at home look like?
The HaH model can take a variety of forms. It has been primarily used for older patients who meet specific clinical and nonclinical eligibility criteria.1 These patients typically are at low risk of requiring complex technical procedures in a hospital setting but require continuous care and/or monitoring for certain conditions, including pneumonia, congestive heart failure, emphysema, pulmonary embolism, and other treatable conditions.1
Effective HaH models include face-to-face clinical care from nurses and physicians, diagnostic testing, continuous monitoring, and specific treatments, such as administering intravenous medication. The care plan for home-based patients typically includes visits by care providers and is driven by telehealth technologies. Digital platforms allow for consistent remote monitoring of patients’ status and enhanced communication.
Clinical and Organizational Research
Independent of emergency circumstances presented by the pandemic, the HaH model is a pragmatic and beneficial way to improve patient outcomes and reduce institutional costs. For many acute conditions, replacing the stressful atmosphere of hospital care with the comfort of the home creates a sense of security for the patient, which manifests in physical and mental benefits.
In fact, a meta-analysis of nine randomized clinical trials documented that when HaH models are used, readmission rates drop by 26% with reduced overall mortality and long-term care risk.2 Patients who receive HaH care report lower depression and anxiety levels and higher patient satisfaction scores than in-hospital patients.2 The benefits also extend to the caregivers involved who report lower stress scale scores.3,4
The HaH model also offers significant benefits on an organizational level. This form of care provides effective treatment at significantly lower costs, ultimately benefiting both the care providers and patients. Studies show that the costs for acute care episodes are reduced by 38% when HaH models are employed.5,6 A health-care market analysis estimated that HAH care is 19% – 30% lower than a traditional in-hospital stay and will result in $5,000 to $7,000 dollars of savings per incident.7
HaH Model Challenges
The HaH model, however, is not short of challenges. Running a telehealth program is a novel concept for many institutions; thus, time and resources are needed to ensure functional and secure digital platforms. Further, trained personnel are needed to provide the clinical care, patient education, and the technology support.
Importantly, the use of telehealth has skyrocketed since the pandemic. A McKinsey analysis estimates that telehealth usage is 38 times higher now than before the pandemic. This clinical and technological advancement has introduced new burdens on systems and personnel.
Adoption of a HaH model will require organizations to address concomitant issues such as patient data security, personnel training, and click fatigue. Indeed, HaH procedures are dependent on the management of hospitals; thus, inefficient workflow or a lack of integration across health systems could significantly impact the success of HaH models.
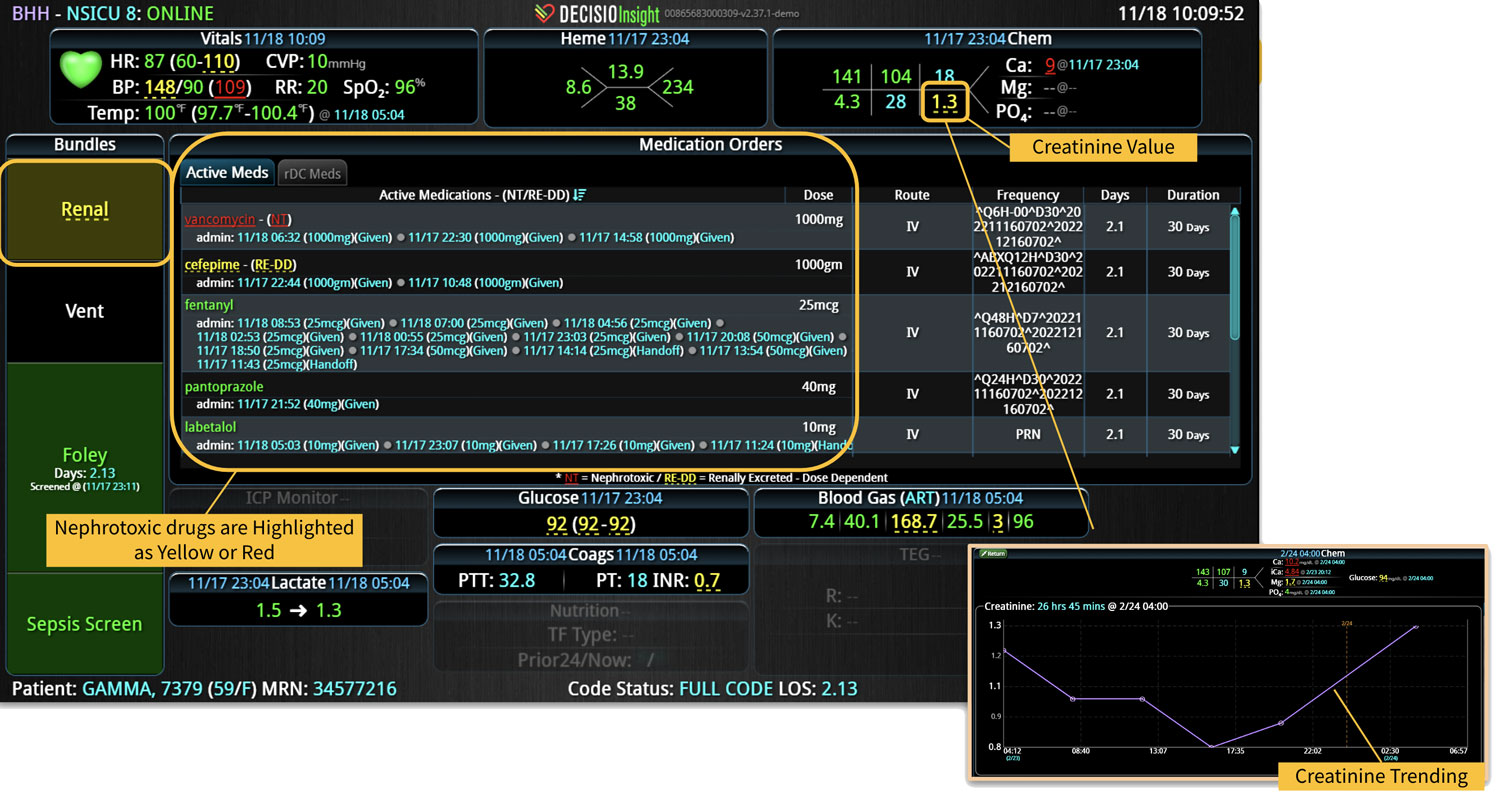
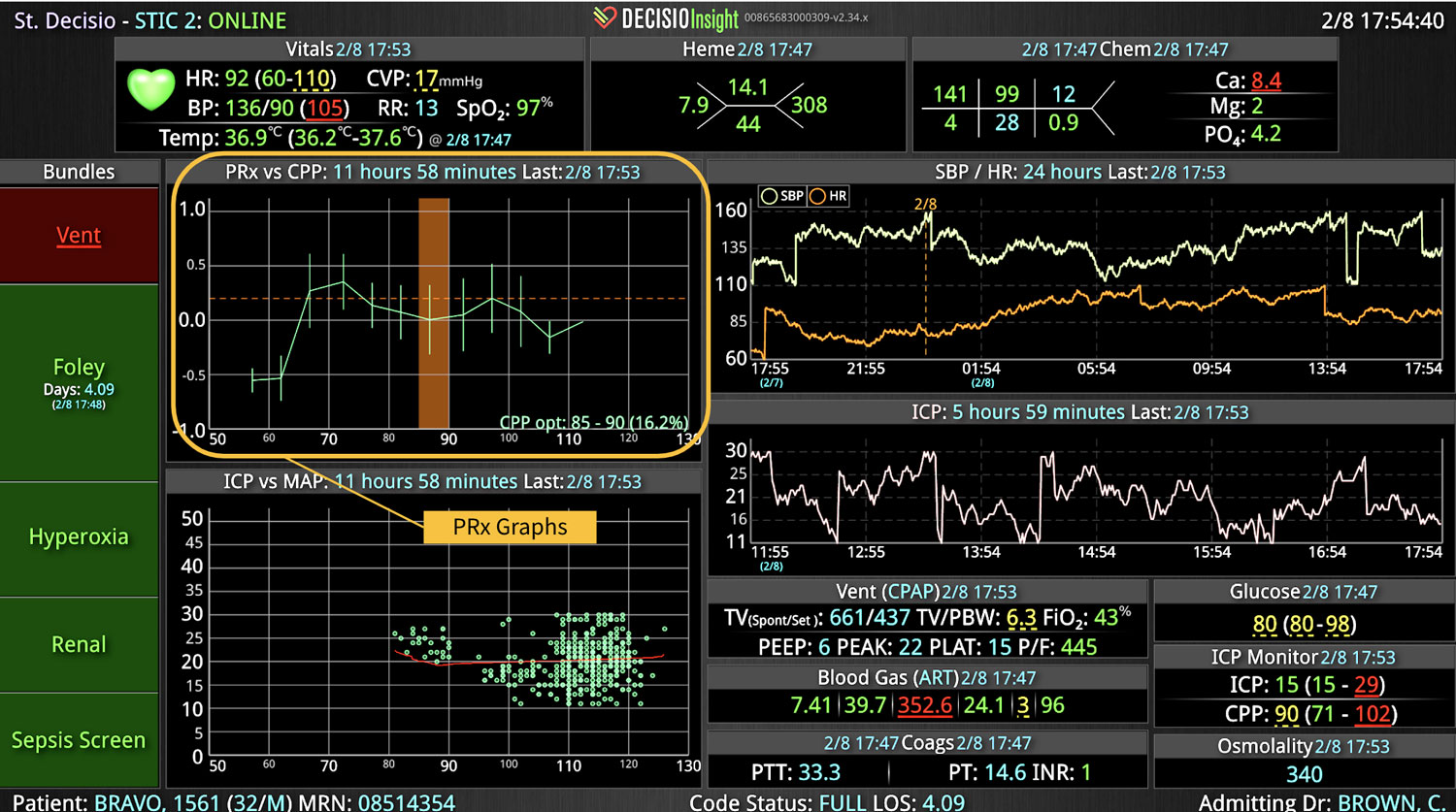
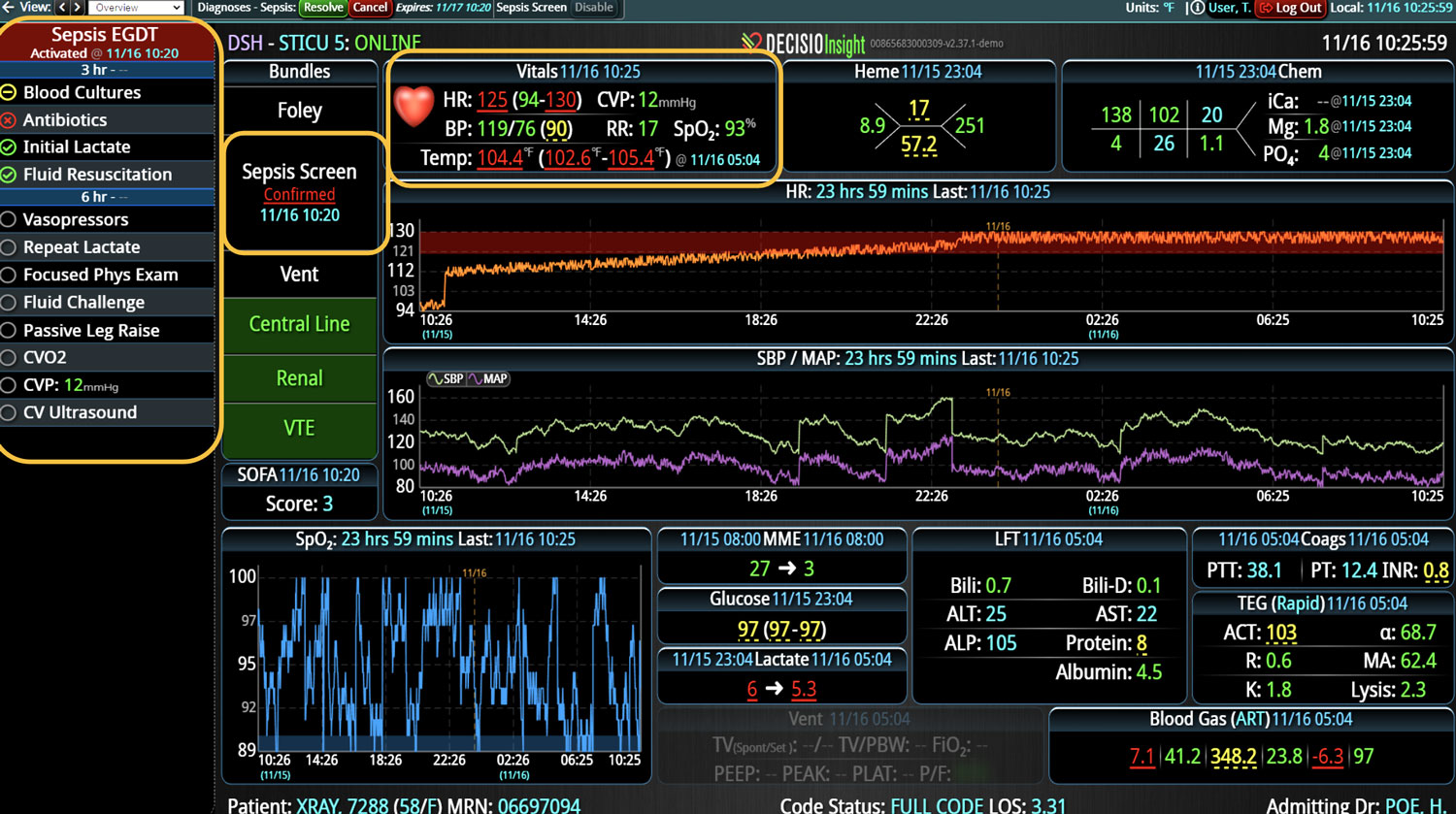
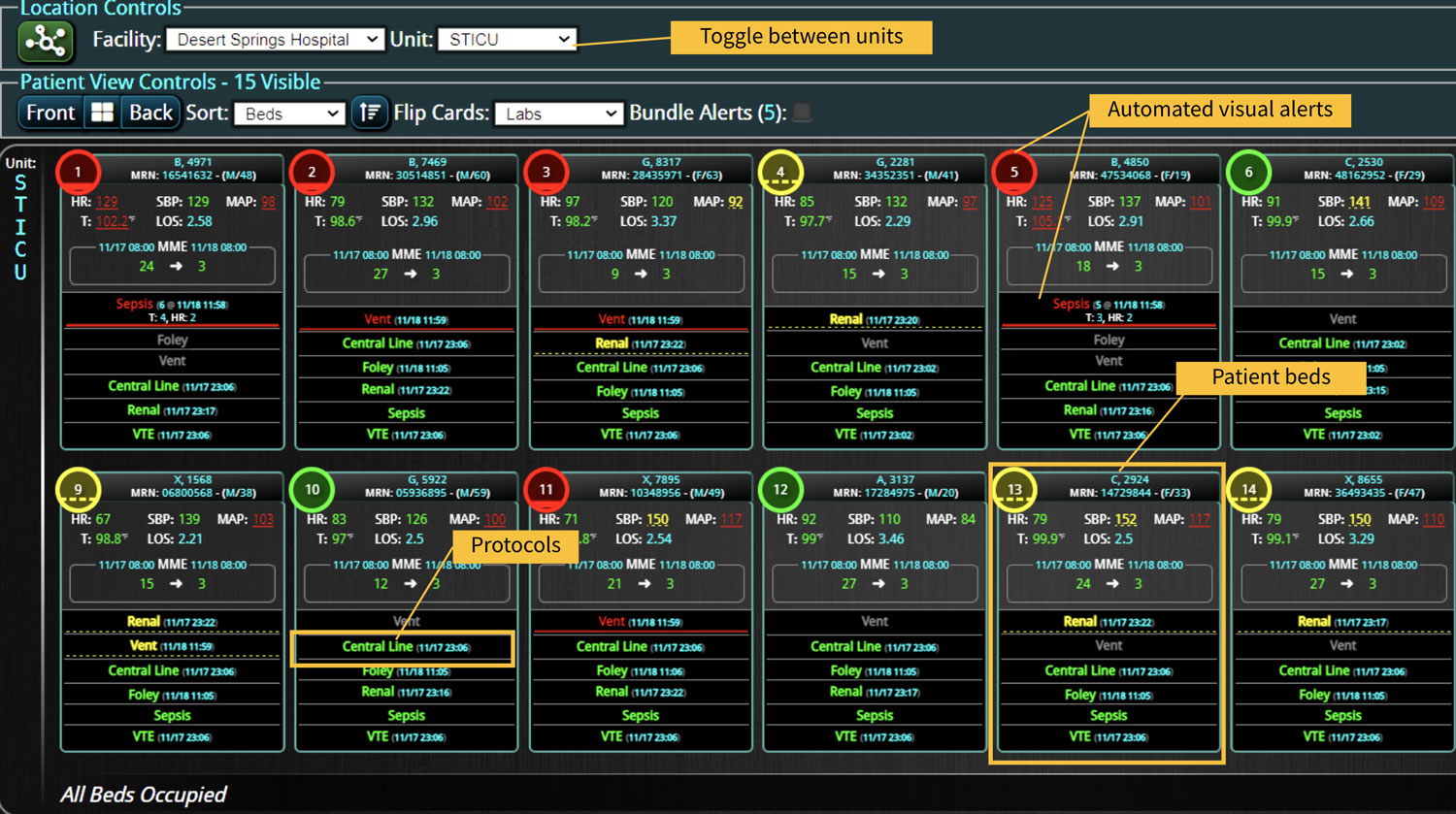
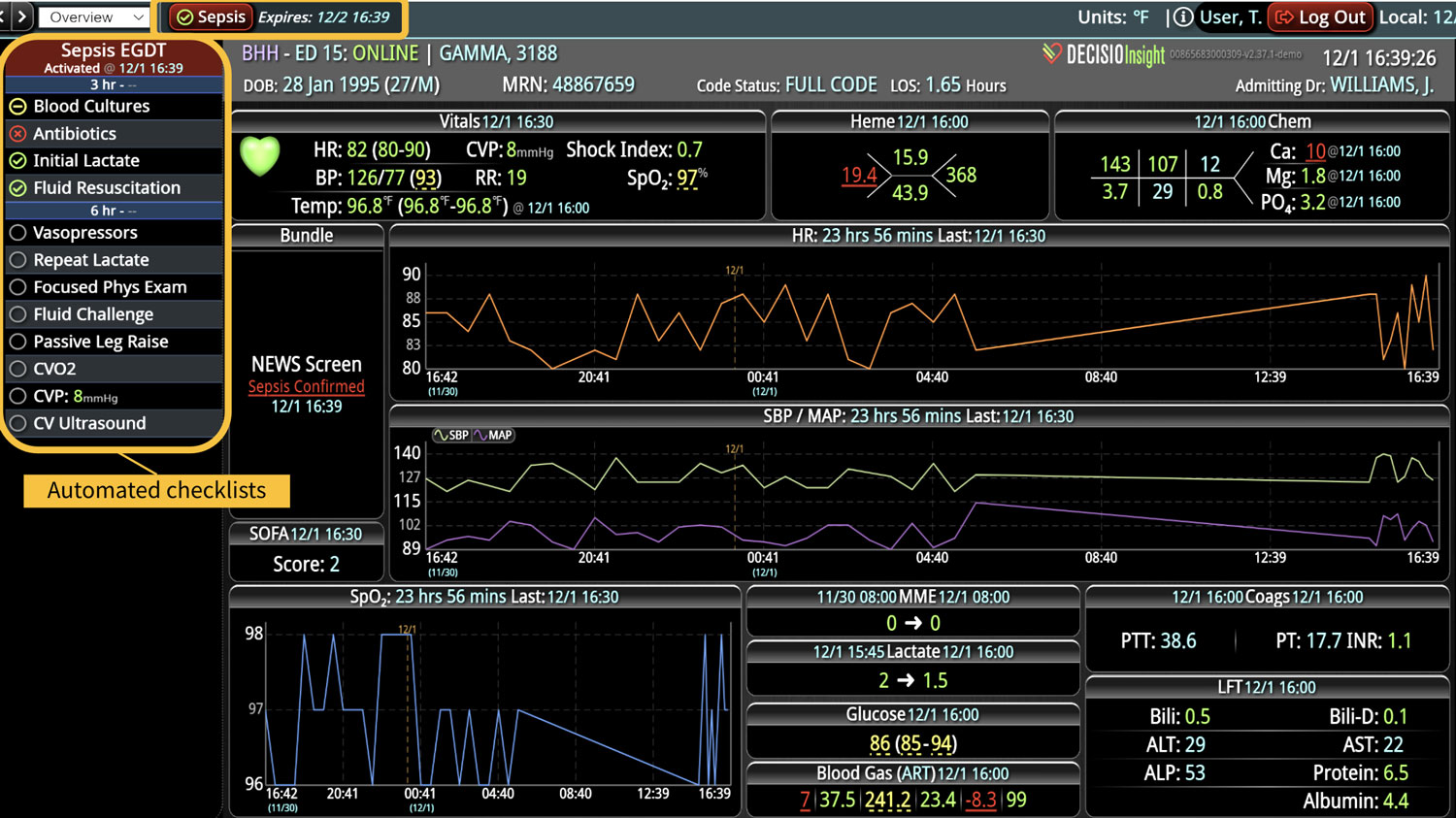
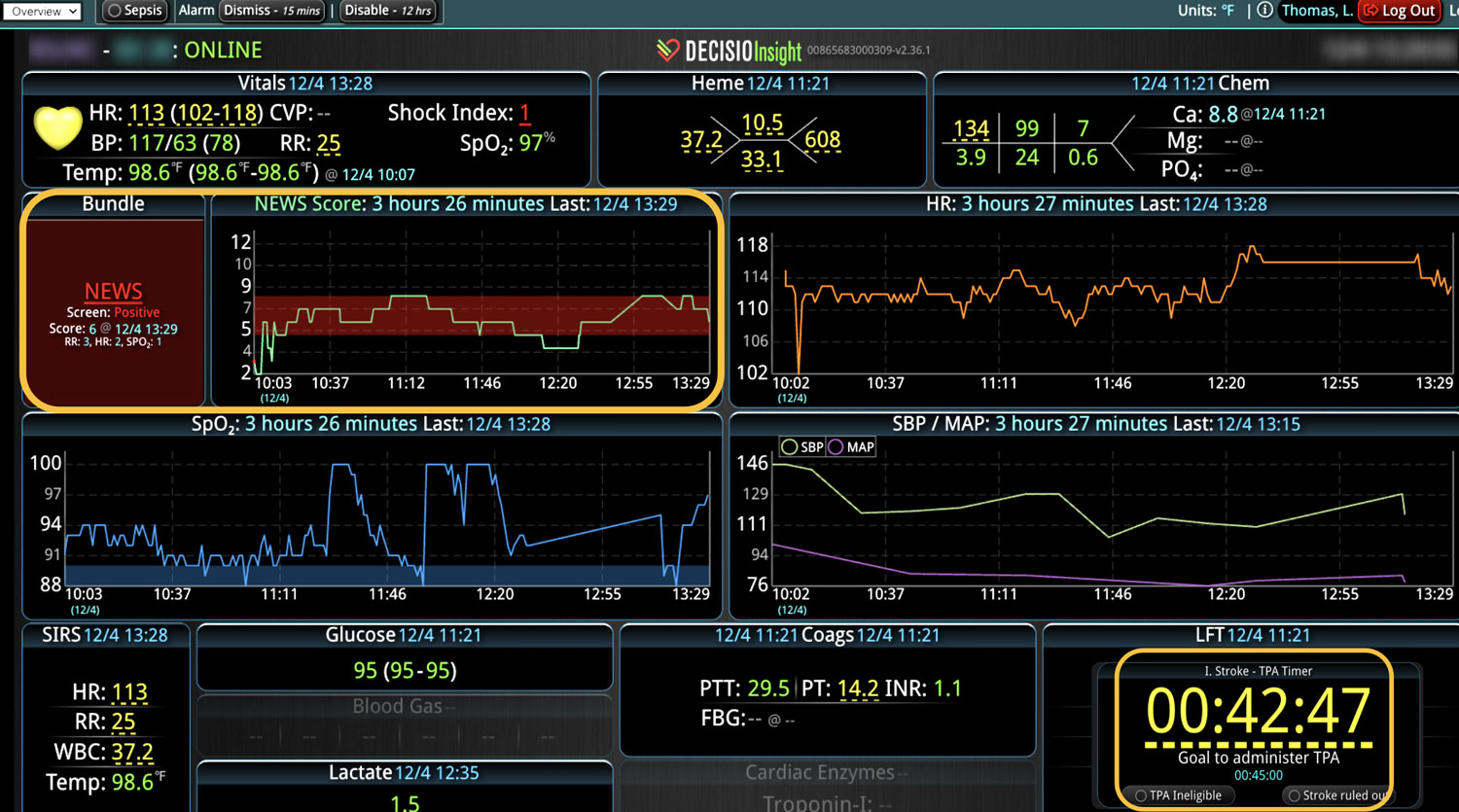
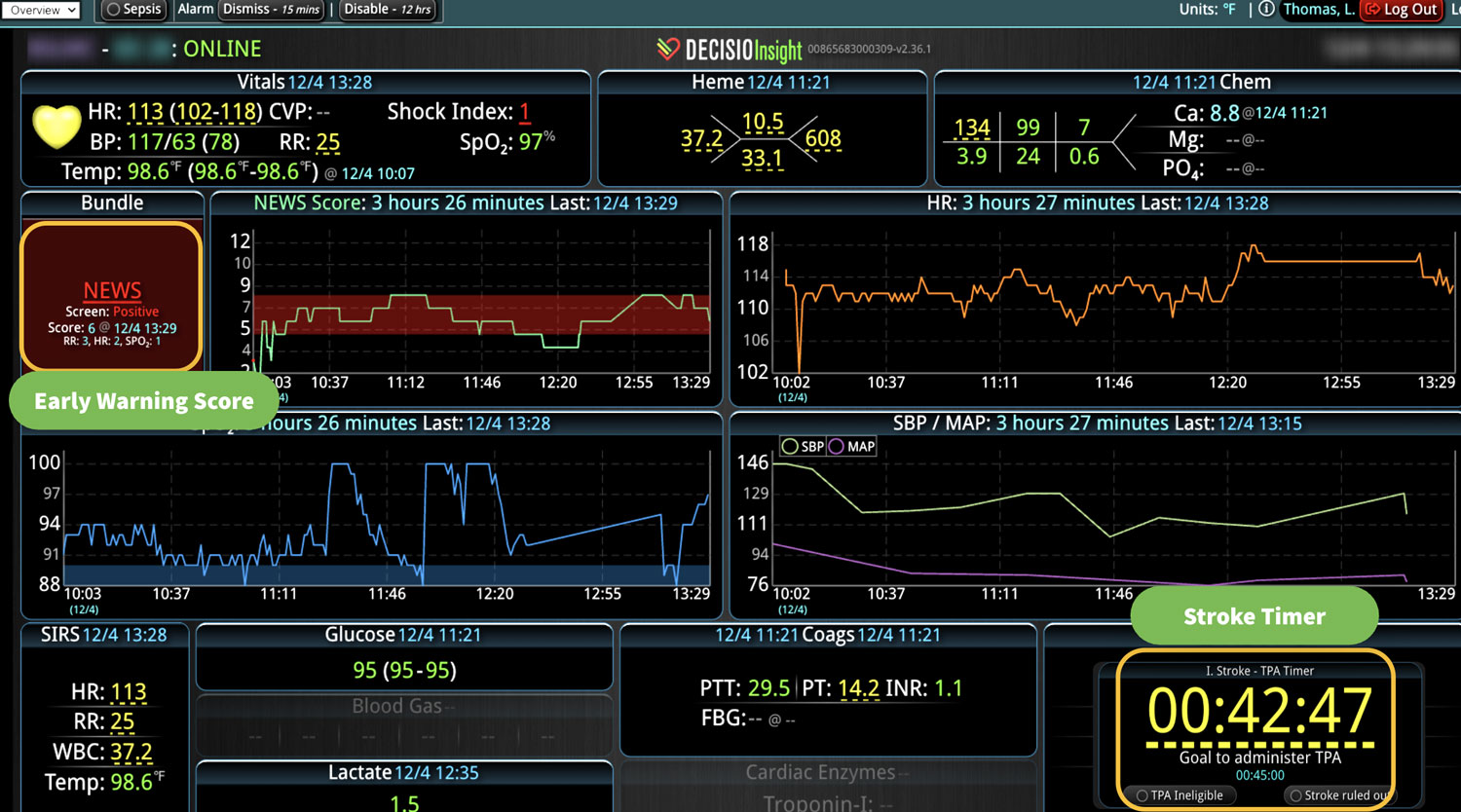
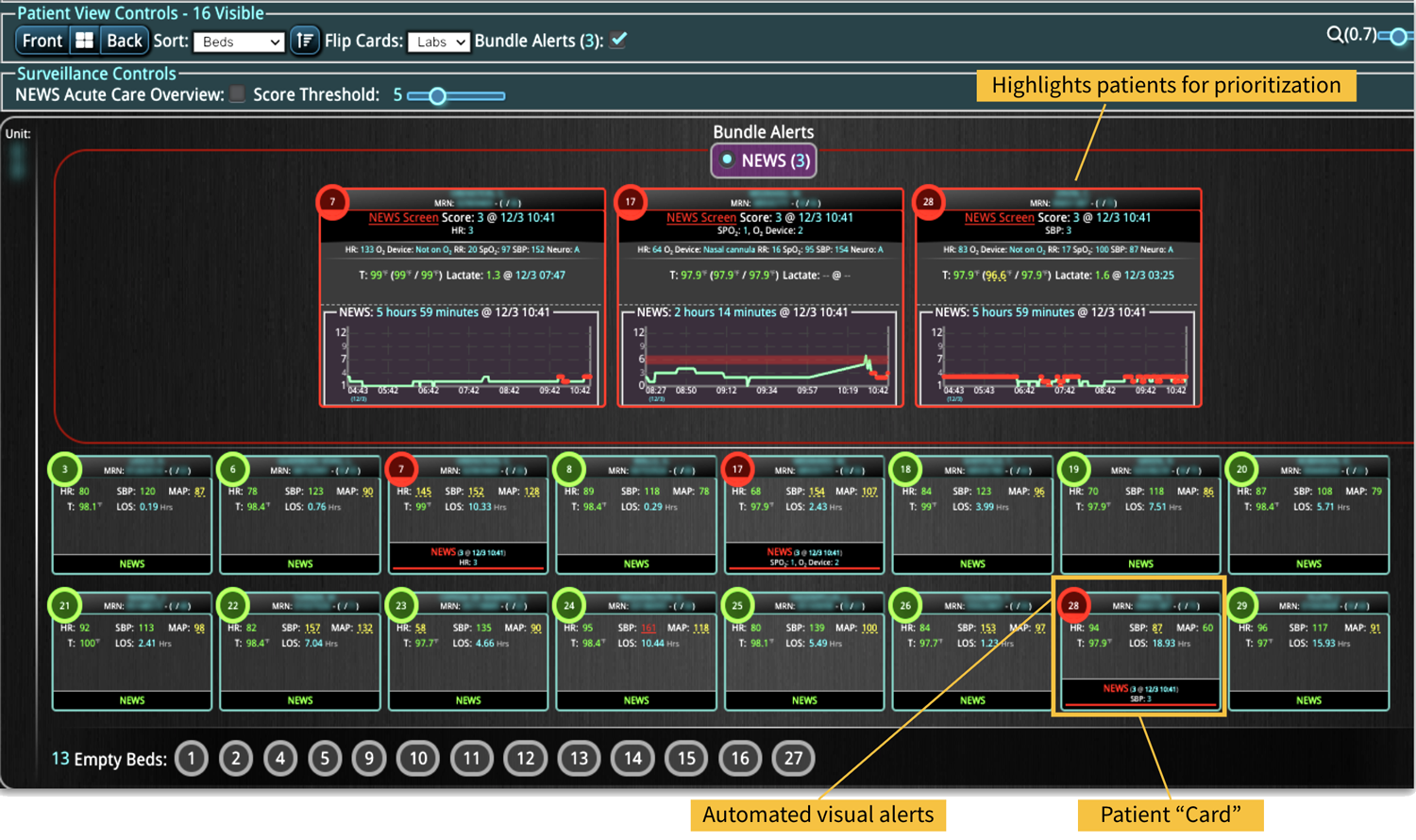
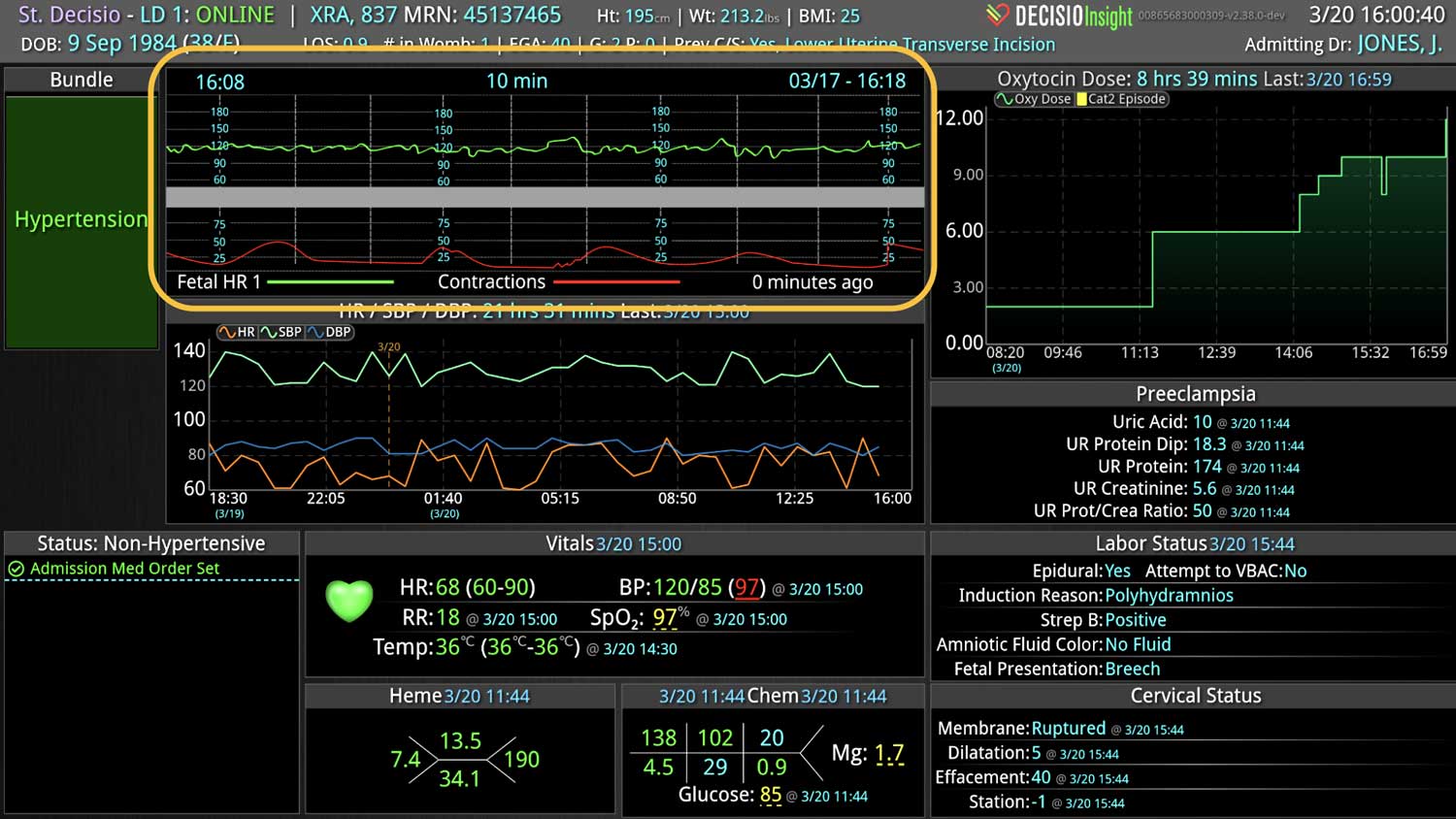
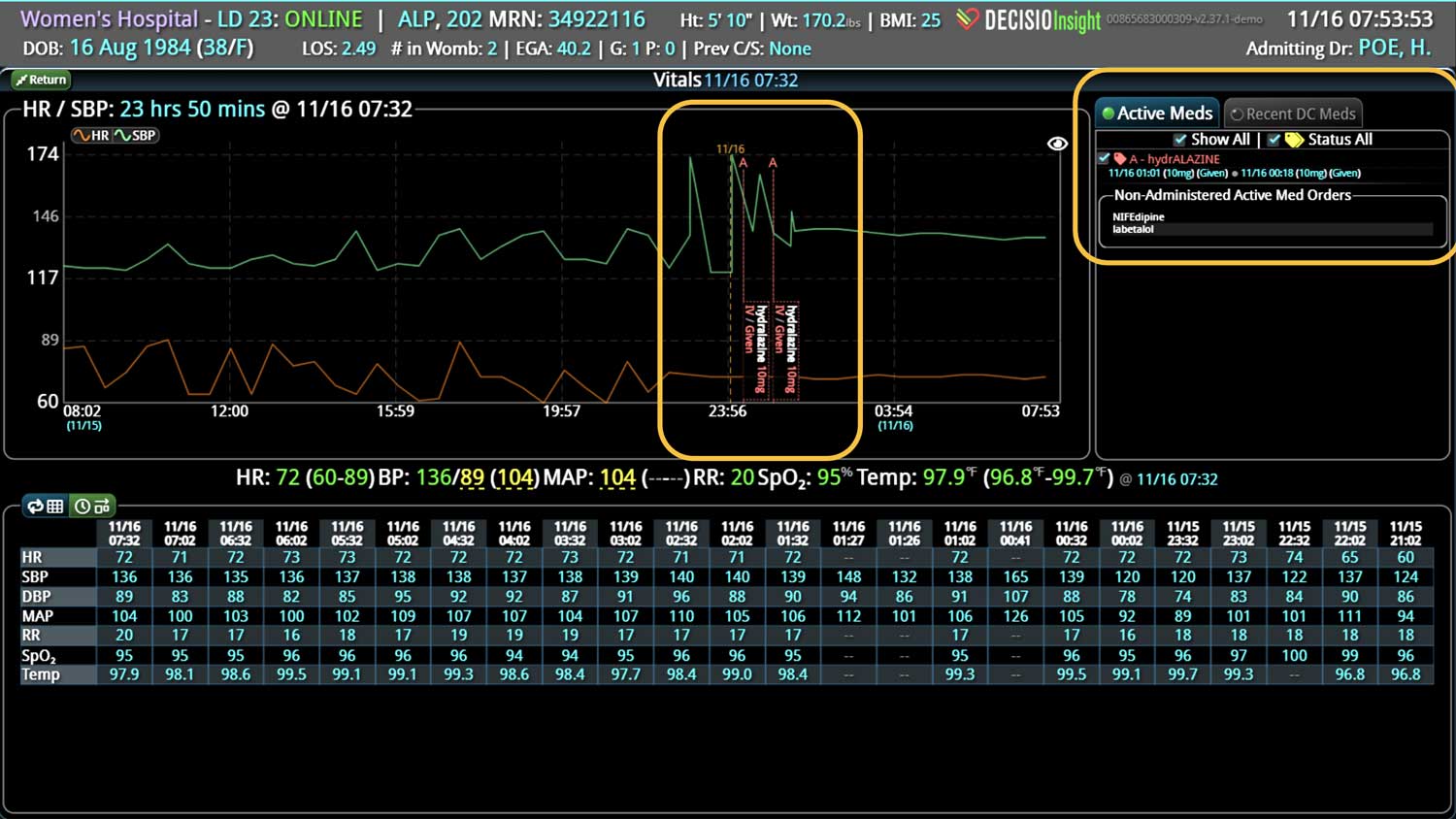
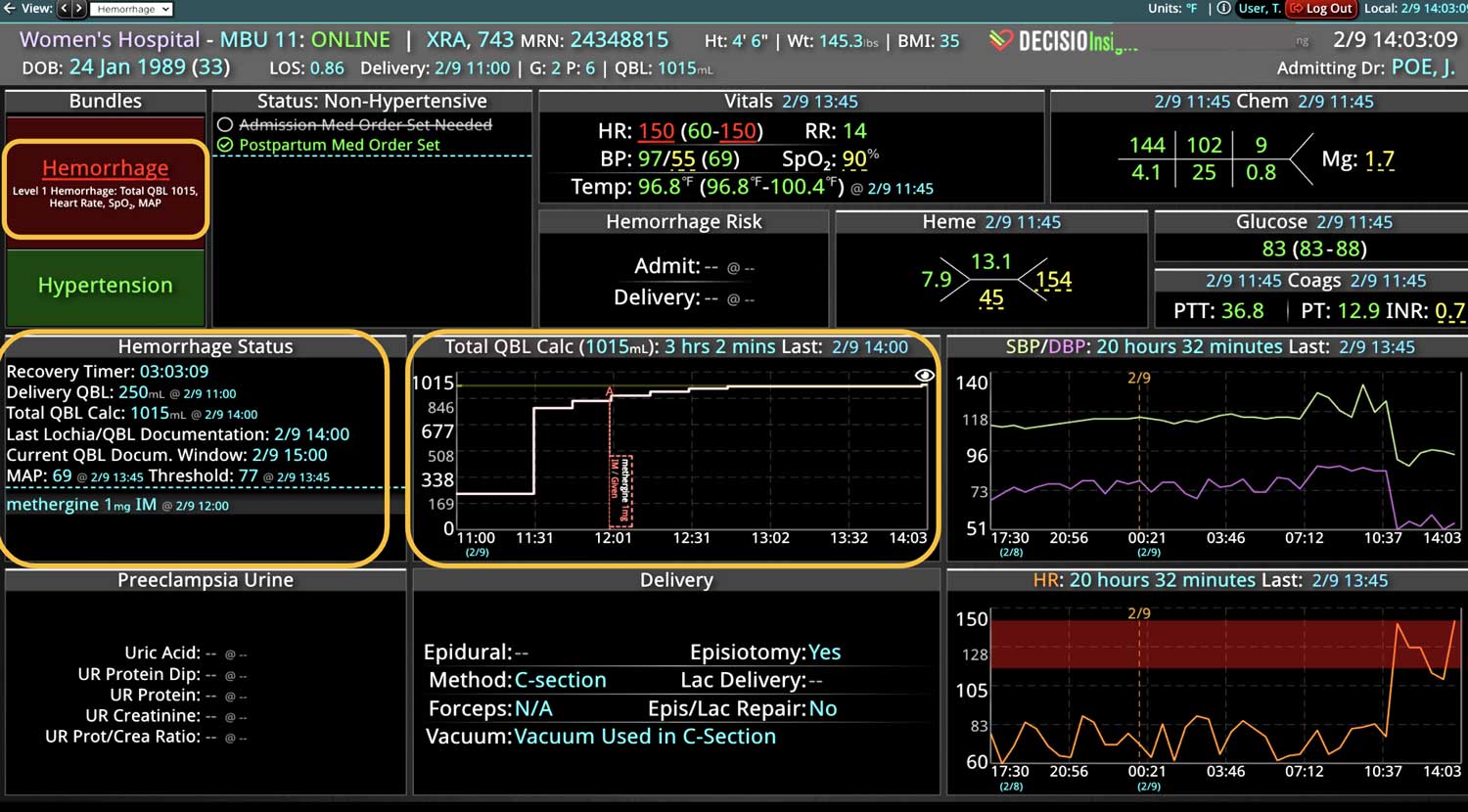
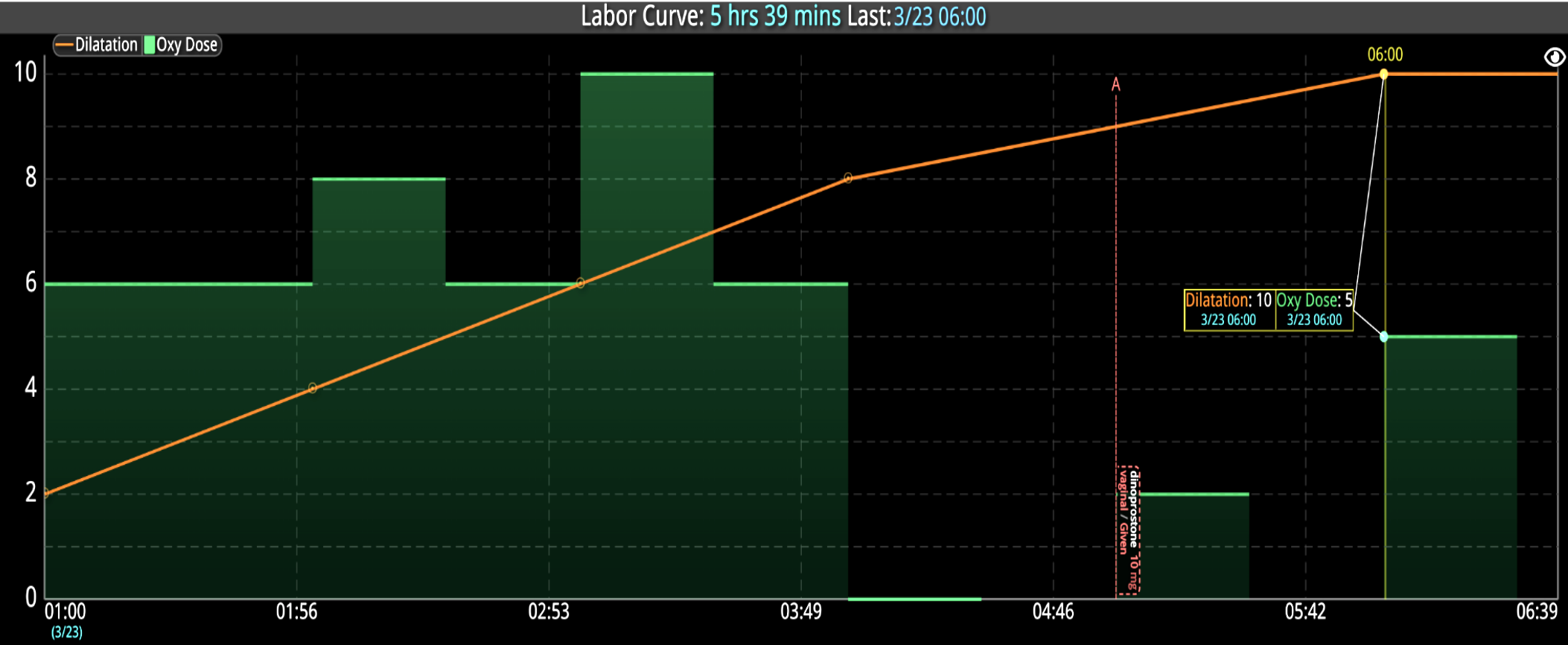
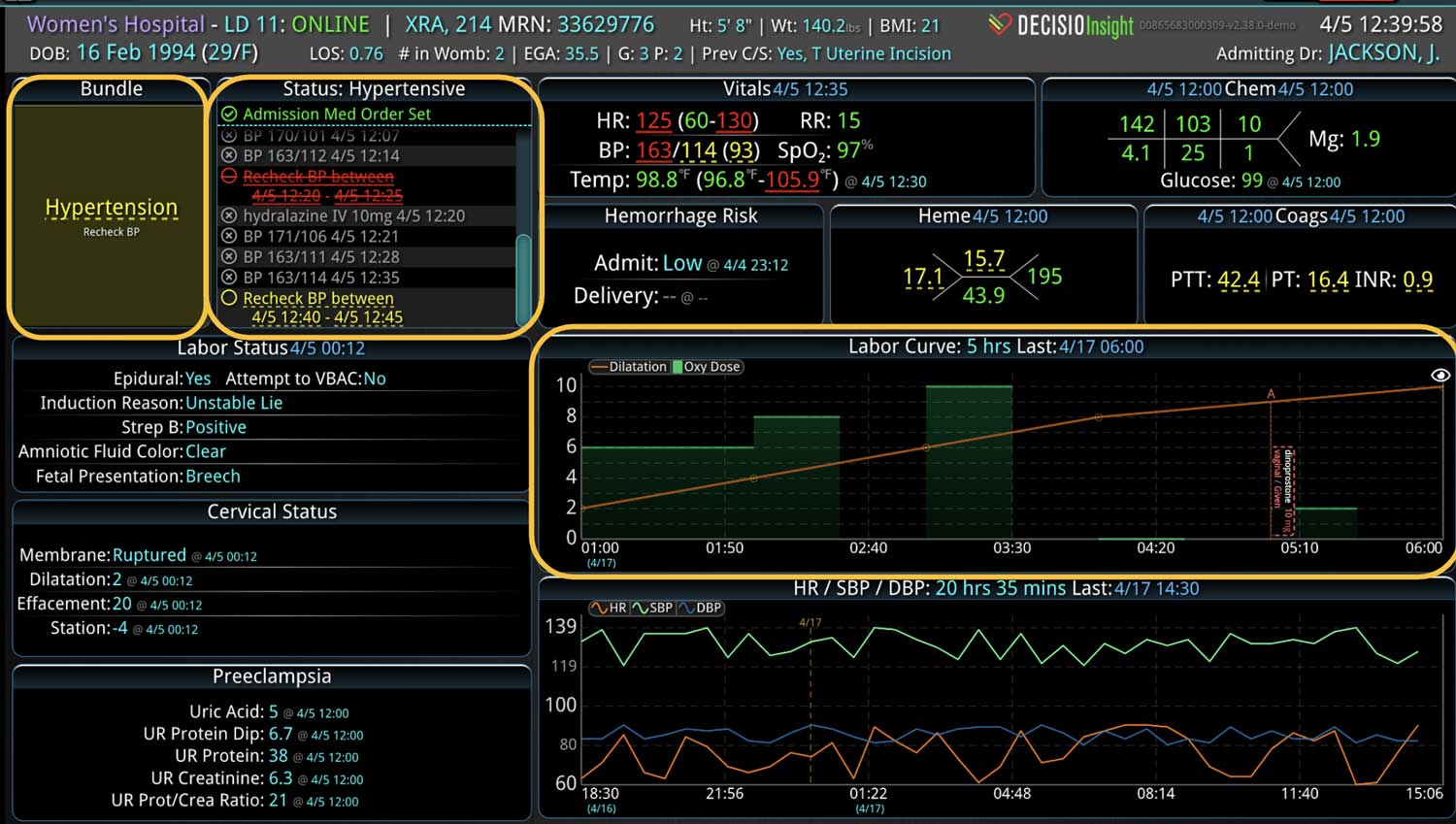
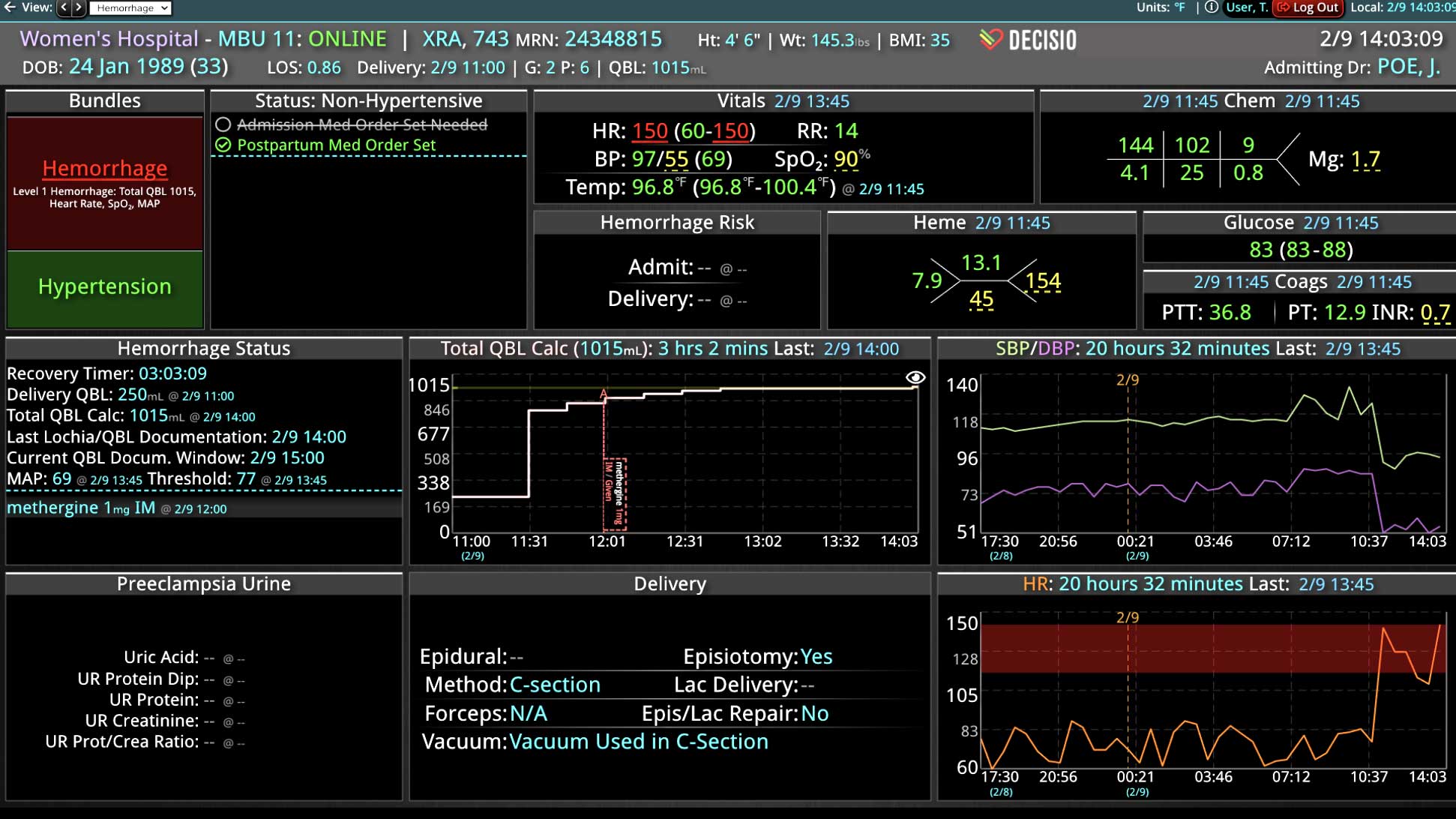
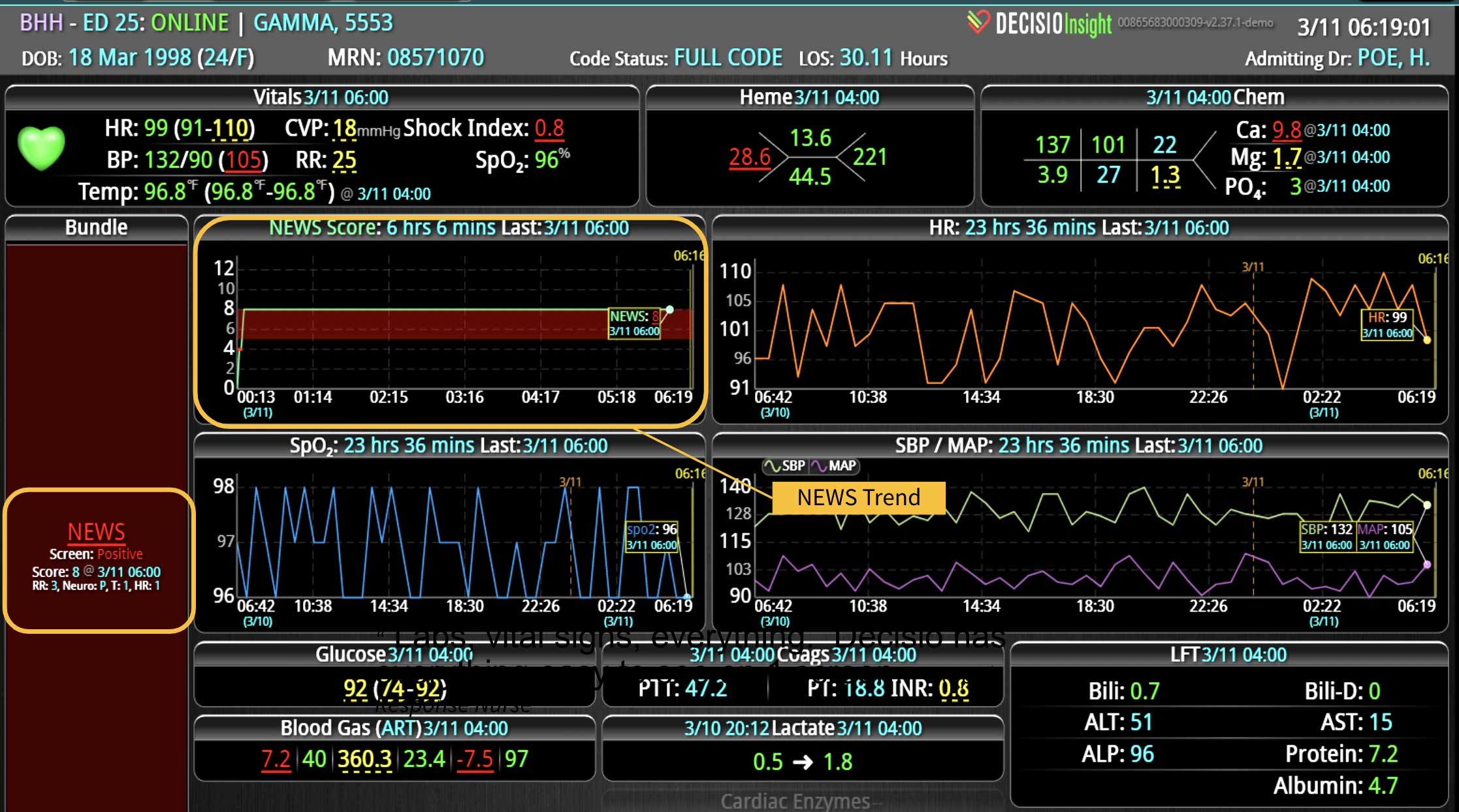
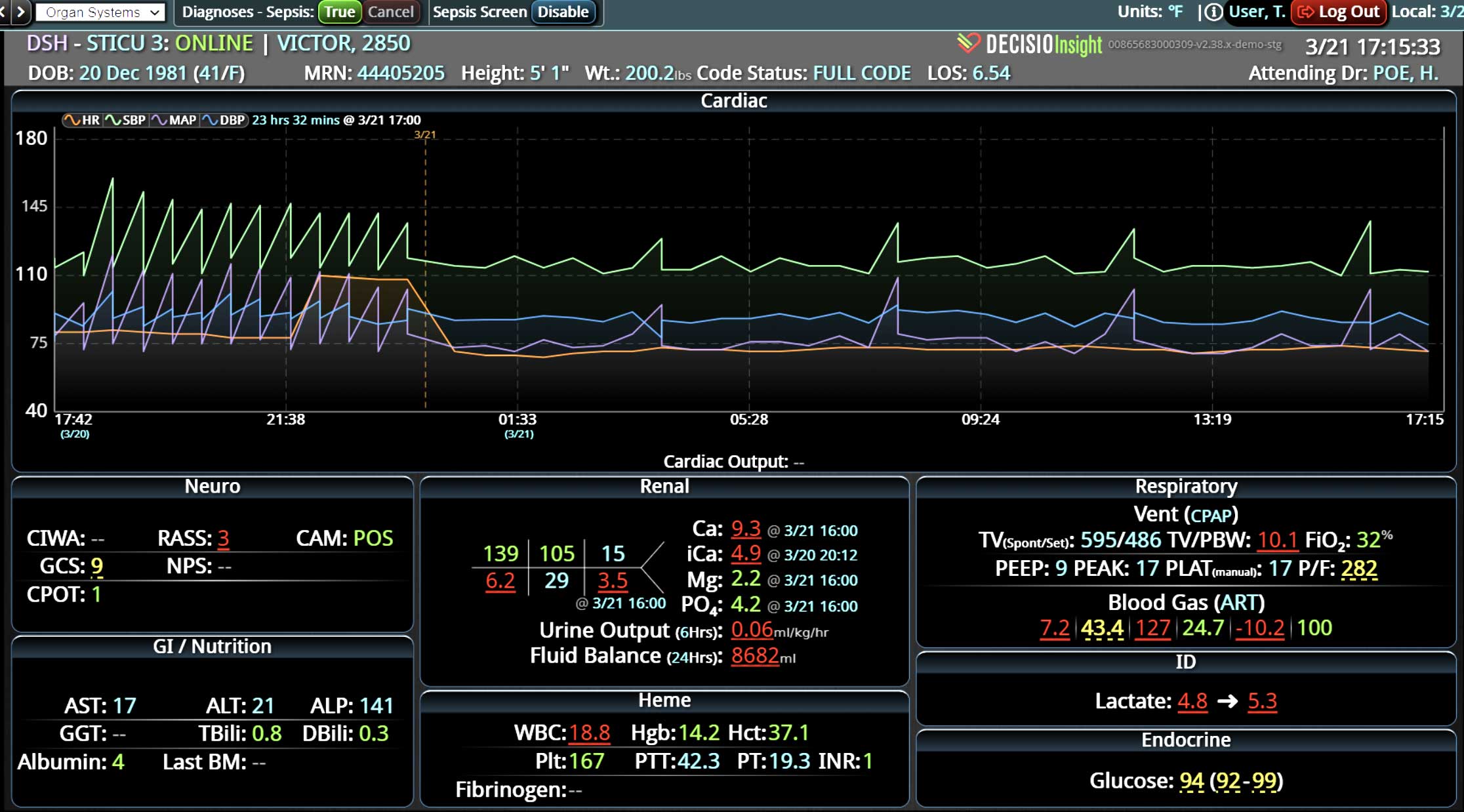
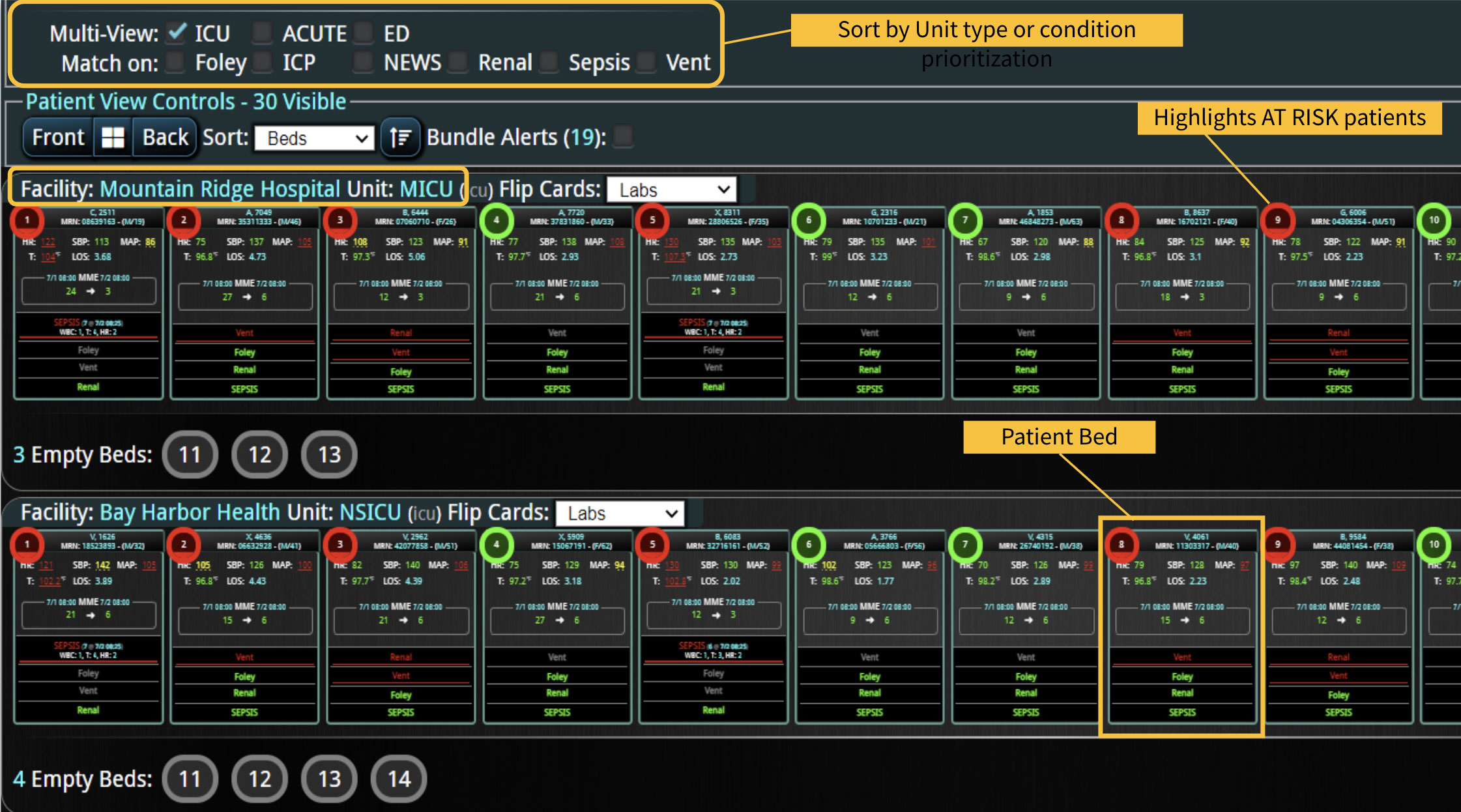
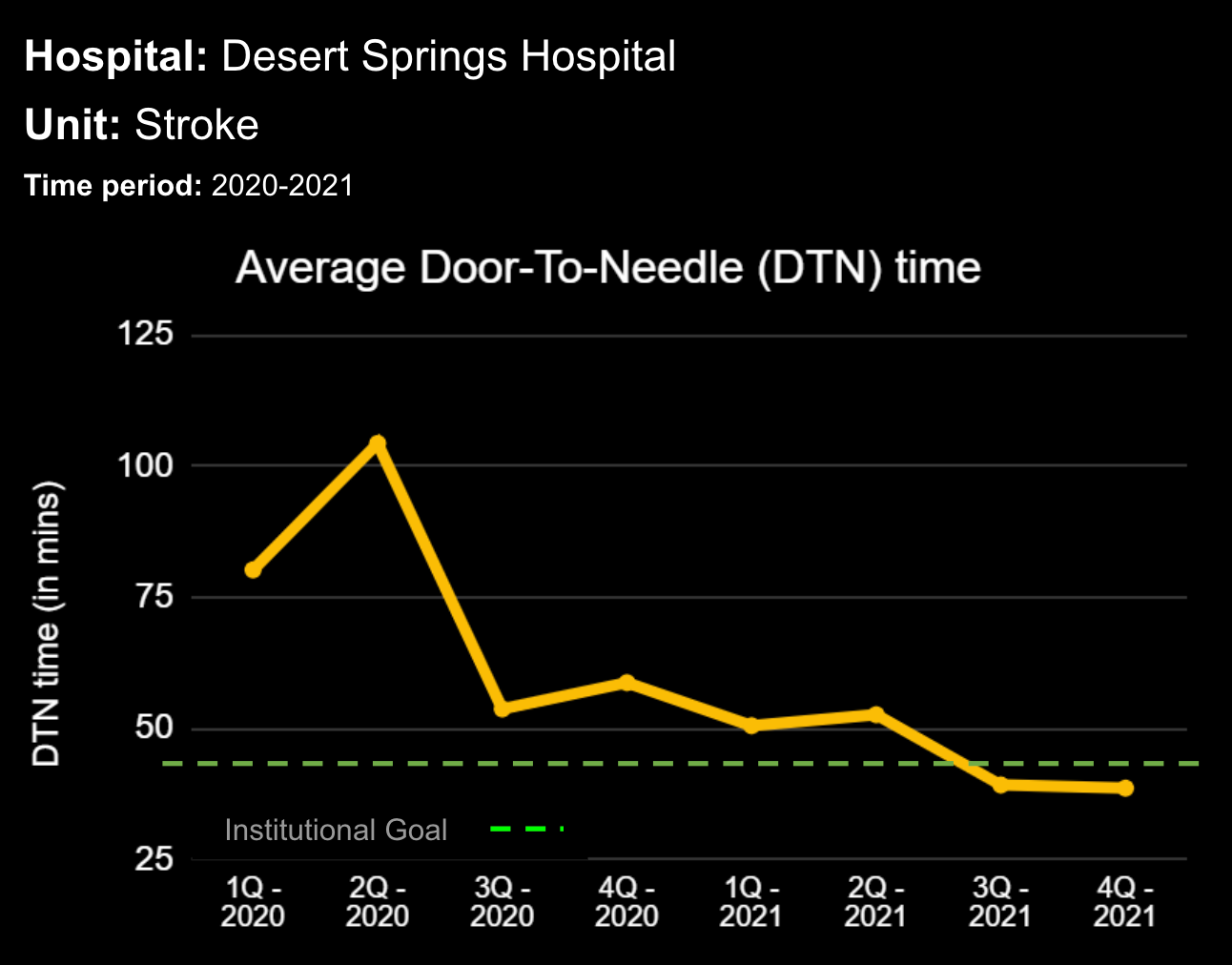
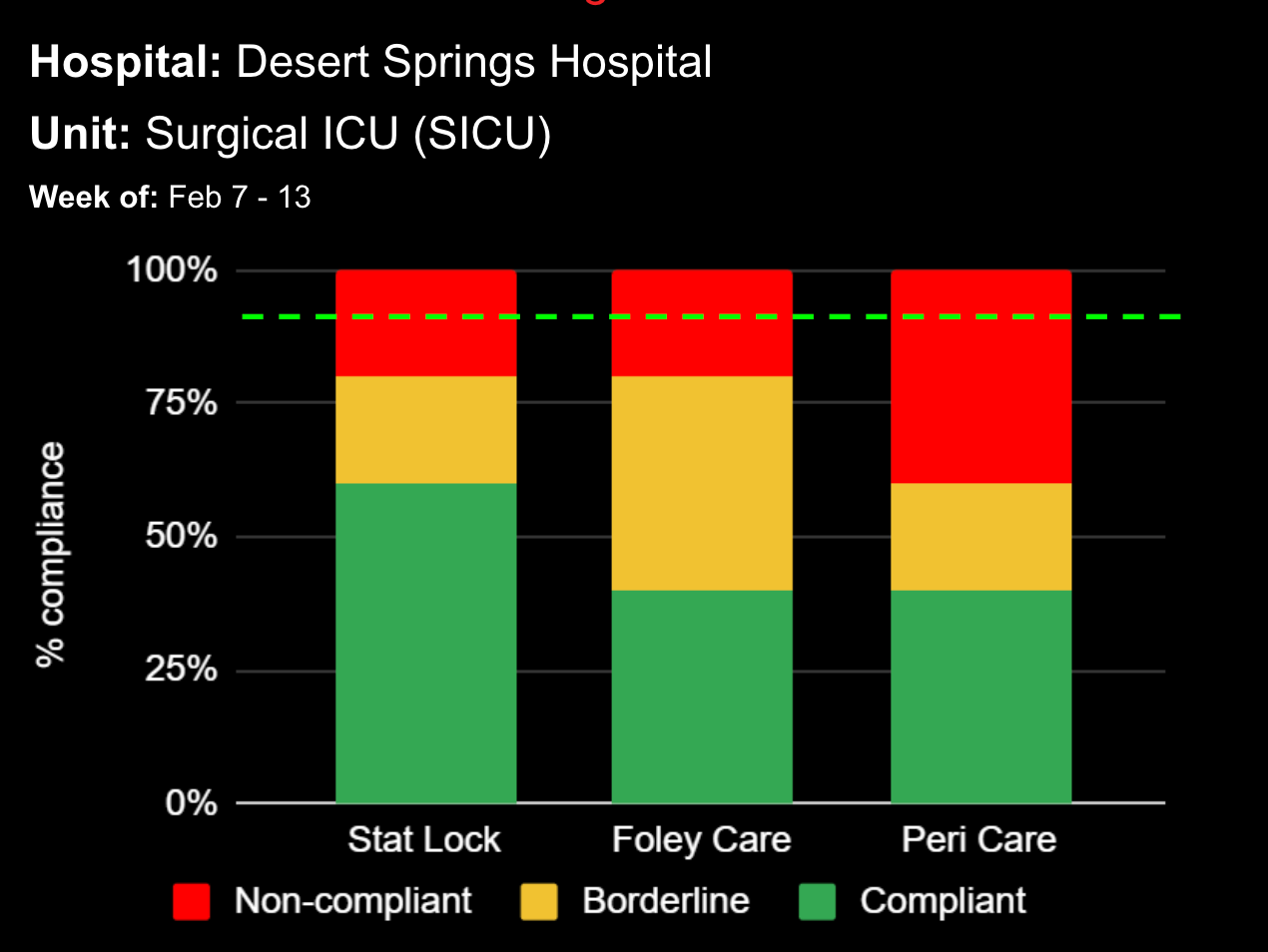
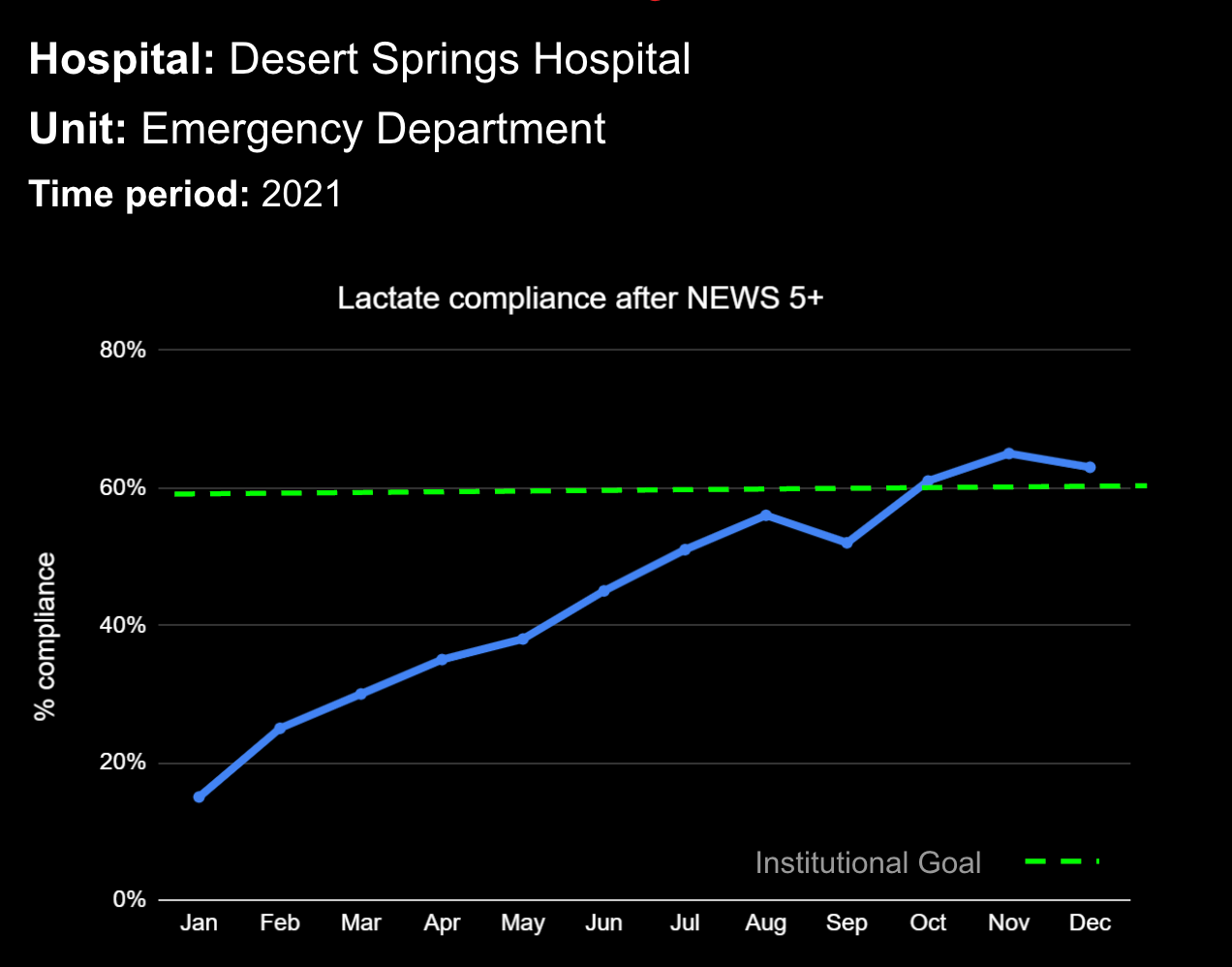
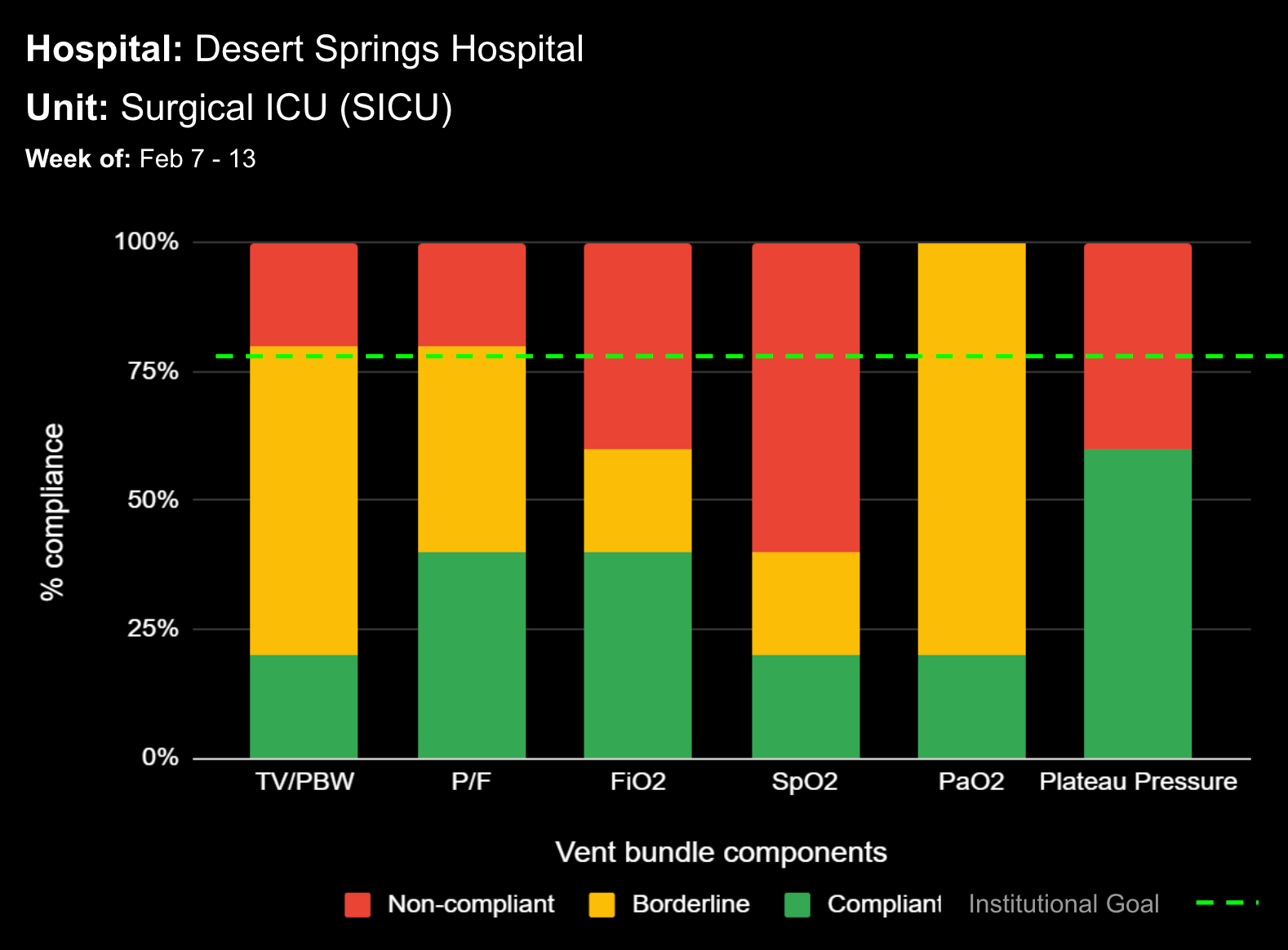
Telehealth technology that offers continuous monitoring of patients, patient data visualization, quick identification of critical patients, and promotes effective workflow is crucial for the ideal HaH system. This technology must integrate data from multiple clinical monitoring devices and the in-home clinical evaluations. Additionally, advanced audiovisual conferencing technology is vital for constant remote physician and patient communication and monitoring. However, advanced and individualized software can help alleviate the burden of today’s clinical demand.
DECISIO is a Texas-based health technology company that has developed multiple software systems that provide near real-time, secure and accurate patient monitoring capabilities. The unique integration of data and clinical guidelines allows for the user and the institutions to improve their clinical decision support and workflow optimization. Most importantly, the software can be tailored to meet the needs of an institution’s individual HaH model. Building on the existing experience and expertise with innovative health technology, DECISIO can pave the way for your organization to enter the new generation of health care—even from home sweet home!
References
- Leff B, Burton L, Bynum JW, et al. Prospective evaluation of clinical criteria to select older persons with acute medical illness for care in a hypothetical home hospital. J Am Geriatr Soc. 1997;45(9):1066-1073. doi:10.1111/j.1532-5415.1997.tb05968.x
- Arsenault-Lapierre G, Henein M, Gaid D, Le Berre M, Gore G, Vedel I. Hospital-at-Home Interventions vs In-Hospital Stay for Patients With Chronic Disease Who Present to the Emergency Department: A Systematic Review and Meta-analysis. JAMA Netw Open. 2021;4(6):e2111568. doi:10.1001/jamanetworkopen.2021.11568
- Aimonino Ricauda N, Tibaldi V, Leff B, et al. Substitutive “hospital at home” versus inpatient care for elderly patients with exacerbations of chronic obstructive pulmonary disease: a prospective randomized, controlled trial. J Am Geriatr Soc. 2008;56(3):493-500. doi:10.1111/j.1532-5415.2007.01562.x
- Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at home for elderly patients with acute decompensation of chronic heart failure: a prospective randomized controlled trial. Arch Intern Med. 2009;169(17):1569-1575. doi:10. 1001/archinternmed.2009.267
- Cryer L, Shannon SB, Amsterdam MV, Leff B. Costs For ‘Hospital at Home’ Patients Were 19 Percent Lower, With Equal Or Better Outcomes Compared To Similar Inpatients. Health Affairs (Millwood, VA). 2012;31(6):1237. doi: 10.1377/hlthaff.2011.1132
- Levine DM, Ouchi K, Blanchfield B, et al. Hospital-Level Care at Home for Acutely Ill Adults: A Randomized Controlled Trial. Ann Intern Med. 2020;172(2):77–85. doi: 10.7326/M19-0600
- Riddleberger K. Hospital-care-at-home worked during the pandemic – now the key is to expand. It. Marketwatch. 2021 Aug 13. Available at: https://www.marketwatch.com/story/hospital-care-at-home-worked-during-the-pandemic-now-the-key-is-to-expand-it-11628878416
Bestsennyy O, Gilbert G, Harris A, Rost J. Telehealth: a quarter-trillion-dollar post-COVID-19 reality? McKinsey & Company [Website]. 2021 Jul 9. Available at: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality
Learn more About How we help clinicians improve patient outcomes
Schedule a call with our team to discuss how we are helping our clients revolutionize how clinicians manage patient interventions.